Abstract
Purpose
To evaluate the prevalence of AMD among optometric telemedicine users in Spain and to identify risk factors.
Methods
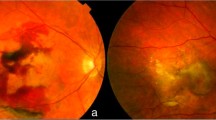
Retrospective analysis of a nationwide database conducted on subjects attending to optometry centers, between January 2013 and December 2019. Fundus photographs were performed by optometrists, using non-mydriatic cameras, and evaluated by a group of 12 retina specialists.
Results
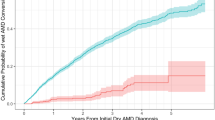
Among the 119,877 subjects included, the overall prevalence of AMD was 7.6%. The prevalence of early, intermediate, and advanced AMD was 2.9%, 2.7%, and 2.0%, respectively. Of the 9129 AMD subjects, 1161 (12.7%) had geographic atrophy, and 1089 (11.9%) had neovascular AMD, either scar (4.5%) or exudative (7.4%). There was a significant association between AMD and age (per year older, adjusted odds ratio, OR 1.116; 95% CI 1.114 to 1.119, p<0.0001). Women had higher prevalence (adjusted OR 1.17; 95% CI 1.12 to 1.23, p<0.0001). Every diopter (spherical equivalent) of progress toward hyperopia was associated with a significant increase in early AMD prevalence (adjusted OR 1.02, 95 CI 1.01 to 1.04, p=0.0074). Presence of diabetes was associated with a lower AMD prevalence (p<0.0001).
Conclusions
The prevalence of AMD (any eye and any severity) was 7.6%, with a prevalence of advanced AMD of 2.0%. Older age and women were significantly associated with a higher prevalence of AMD, whereas myopia and presence of diabetes were associated with significantly lower odds of any AMD.




Similar content being viewed by others
Abbreviations
- VI:
-
Álava
- AB:
-
Albacete
- A:
-
Alicante
- AL:
-
Almería
- O:
-
Asturias
- AV:
-
Ávila
- BA:
-
Badajoz
- IB:
-
Balearic Islands
- B:
-
Barcelona
- BU:
-
Burgos
- CC:
-
Caceres
- CA:
-
Cádiz
- S:
-
Cantabria
- CS:
-
Castellon
- CE:
-
Ceuta
- CR:
-
Ciudad Real
- CO:
-
Córdoba
- C:
-
Coruña
- CU:
-
Cuenca
- GI:
-
Gerona
- GR:
-
Granada
- GU:
-
Guadalajara
- SS:
-
Gipuzkoa
- H:
-
Huelva
- HU:
-
Huesca
- J:
-
Jaen
- LE:
-
León
- L:
-
Lerida
- LU:
-
Lugo
- M:
-
Madrid
- MA:
-
Málaga
- MU:
-
Murcia
- NA:
-
Navarre
- OU:
-
Orense
- P:
-
Palencia
- GC:
-
Las Palmas
- PO:
-
Pontevedra
- LO:
-
La Rioja
- SA:
-
Salamanca
- SG:
-
Segovia
- SE:
-
Seville
- SO:
-
Soria
- T:
-
Tarragona
- TF:
-
Tenerife
- TE:
-
Teruel
- TO:
-
Toledo
- V:
-
Valencia
- VA:
-
Valladolid
- BI:
-
Vizcaya
- ZA:
-
Zamora
- Z:
-
Zaragoza
References
Klein R, Klein BE, Linton KL (1992) Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 99(6):933–943. https://doi.org/10.1016/s0161-6420(92)31871-8
Mitchell P, Smith W, Attebo K, Wang JJ (1995) Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology. 102(10):1450–1460. https://doi.org/10.1016/s0161-6420(95)30846-9
Vingerling JR, Dielemans I, Hofman A, Grobbee DE, Hijmering M, Kramer CF, de Jong PT (1995) The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology. 102:205–210. https://doi.org/10.1016/s0161-6420(95)31034-2
Vannewkirk MR, Nanjan MB, Wang JJ, Mitchell P, Taylor HR, McCarty CA (2000) The prevalence of age-related maculopathy: the visual impairment project. Ophthalmology. 107:1593–1600. https://doi.org/10.1016/s0161-6420(00)00175-5
Augood CA, Vingerling JR, de Jong PT, et al (2006). Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE). Arch Ophthalmol. 124(4):529-535. doi: https://doi.org/10.1001/archopht.124.4.529.
Kawasaki R, Yasuda M, Song SJ, Chen SJ, Jonas JB, Wang JJ, Mitchell P, Wong TY (2010) The prevalence of age-related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology. 117(5):921–927. https://doi.org/10.1016/j.ophtha.2009.10.007
Korb CA, Kottler UB, Wolfram C, Hoehn R, Schulz A, Zwiener I, Wild PS, Pfeiffer N, Mirshahi A (2014) Prevalence of age-related macular degeneration in a large European cohort: results from the population-based Gutenberg Health Study. Graefes Arch Clin Exp Ophthalmol 252(9):1403–1411. https://doi.org/10.1007/s00417-014-2591-9
Wong WL, Su X, Li X et al (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2(2):e106–e116. https://doi.org/10.1016/S2214-109X(13)70145-1
García-Layana A, Cabrera-López F, García-Arumí J, Arias-Barquet L, Ruiz-Moreno JM (2017) Early and intermediate age-related macular degeneration: update and clinical review. Clin Interv Aging 12:1579–1587. https://doi.org/10.2147/CIA.S142685
Lüdtke L, Jürgens C, Ittermann T, Völzke H, Tost F (2019) Age-related macular degeneration and associated risk factors in the population-based study of health in Pomerania (SHIP-Trend). Med Sci Monit 25:6383–6390. https://doi.org/10.12659/MSM.915493
Klein R, Klein BEK, Linton KLP (2020) Prevalence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 127(4S):S122–S132. https://doi.org/10.1016/j.ophtha.2020.01.033
Pennington KL, DeAngelis MM (2016) Epidemiology of age-related macular degeneration (AMD): associations with cardiovascular disease phenotypes and lipid factors. Eye Vis (Lond) 3:34. https://doi.org/10.1186/s40662-016-0063-5
Serrano-Garijo P, Ramírez-Sebastián JM (1991) Detección de las alteraciones visuales en el anciano. Rev Esp Geriatr Gerontol. 26:21–28
Lago Bouza JR. Prevalencia de la degradación macular asociada a la edad en una población hospitalaria del área sanitaria de Santiago de Compostela. Available in https://dialnet.unirioja.es/servlet/tesis?codigo=109565 Last accessed July 30, 2020.
Damián J, Pastor R, Armadá F, Arias L (2006) Epidemiología de la degeneración macular asociada con la edad. Situación en España. Aten Primaria 38(1):51–57. https://doi.org/10.1157/13090016
Zapata MA, Arcos G, Fonollosa A, Abraldes M, Oleñik A, Gutierrez E, Garcia-Arumi J (2017) Telemedicine for a general screening of retinal disease using nonmydriatic fundus cameras in optometry centers: three-year results. Telemed J E Health. 23(1):30–36. https://doi.org/10.1089/tmj.2016.0020
Authors not listed. Diabetic eye screening: guidance on camera approval. Updated January 3, 2018. Available in: https://www.gov.uk/government/publications/diabetic-eye-screening-approved-cameras-and-settings/diabetic-eye-screening-guidance-on-camera-approval Last accessed July 30, 2020.
Ferris FL 3rd, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, Sadda SR, Beckman Initiative for Macular Research Classification Committee (2013) Clinical classification of age-related macular degeneration. Ophthalmology. 120(4):844–851. https://doi.org/10.1016/j.ophtha.2012.10.036
1. Instituto nacional de estadística (INE) [Internet]. INE. 2020. Available at: https://www.ine.es/jaxi/Tabla.htm?path=/t20/e245/p08/l0/&file=01002.px&L=0. Accessed 15th Oct 2020
Erke MG, Bertelsen G, Peto T, Sjølie AK, Lindekleiv H, Njølstad I (2012) Prevalence of age-related macular degeneration in elderly Caucasians: the Tromsø Eye Study. Ophthalmology. 119(9):1737–1743. https://doi.org/10.1016/j.ophtha.2012.03.016
Owen CG, Jarrar Z, Wormald R, Cook DG, Fletcher AE, Rudnicka AR (2012) The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol. 96(5):752–756. https://doi.org/10.1136/bjophthalmol-2011-301109
van Leeuwen R, Boekhoorn S, Vingerling JR, Witteman JC, Klaver CC, Hofman de Jong PT (2005) Dietary intake of antioxidants and risk of age-related macular degeneration. JAMA 294(24):3101–3107. https://doi.org/10.1001/jama.294.24.3101
Arslan S, Kadayifçilar S, Samur G (2019) The potential role of dietary antioxidant capacity in preventing age-related macular degeneration. J Am Coll Nutr. 38(5):424–432. https://doi.org/10.1080/07315724.2018.1538830
Evans JR, Lawrenson JG (2017) Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration. Cochrane Database Syst Rev. 7:CD000253. https://doi.org/10.1002/14651858.CD000253.pub4
Olmedo-Requena R, González-Donquiles C, Dávila-Batista V, Romaguera D, Castelló A, Molina de la Torre AJ et al (2019) Agreement among Mediterranean diet pattern adherence indexes: MCC-Spain study. Nutrients. 11(3):488. https://doi.org/10.3390/nu11030488
Spanish Eyes Epidemiological (SEE) Study Group (2011) Prevalence of age-related macular degeneration in Spain. Br J Ophthalmol. 95(7):931–936. https://doi.org/10.1136/bjo.2010.187773
Smith W, Assink J, Klein R, Mitchell P, Klaver CC, Klein BE, Hofman A, Jensen S, Wang JJ, de Jong PT (2001). Risk factors for age-related macular degeneration: pooled findings from three continents. Ophthalmology 108(4):697-704. https://doi.org/10.1016/s0161-6420(00)00580-7.
Evans JR, Fletcher AE, Wormald RP (2004) Age-related macular degeneration causing visual impairment in people 75 years or older in Britain: an add-on study to the Medical Research Council Trial of Assessment and Management of Older People in the Community. Ophthalmology. 111(3):513–517. https://doi.org/10.1016/j.ophtha.2003.07.012
Wang JJ, Mitchell P, Smith W (1998) Refractive error and age-related maculopathy: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 39(11):2167–2171
Ikram MK, van Leeuwen R, Vingerling JR, Hofman A, de Jong PT (2003) Relationship between refraction and prevalent as well as incident age-related maculopathy: the Rotterdam study. Invest Ophthalmol Vis Sci. 44(9):3778–3782. https://doi.org/10.1167/iovs.03-0120
Pallikaris IG, Kymionis GD, Ginis HS, Kounis GA, Christodoulakis E, Tsilimbaris MK (2006) Ocular rigidity in patients with age-related macular degeneration. Am J Ophthalmol. 141(4):611–615. https://doi.org/10.1016/j.ajo.2005.11.010
He MS, Chang FL, Lin HZ, Wu JL, Hsieh TC, Lee YC (2018) The association between diabetes and age-related macular degeneration among the elderly in Taiwan. Diabetes Care. 41(10):2202–2211. https://doi.org/10.2337/dc18-0707
Chen X, Rong SS, Xu Q, Tang FY, Liu Y, Gu H et al (2014) Diabetes mellitus and risk of age-related macular degeneration: a systematic review and meta-analysis. PLoS One 9(9):e108196. https://doi.org/10.1371/journal.pone.0108196
Srinivasan S, Swaminathan G, Kulothungan V, Ganesan S, Sharma T, Raman R (2017) Age-related macular degeneration in a South Indian population, with and without diabetes. Eye (Lond) 31(8):1176–1183. https://doi.org/10.1038/eye.2017.47
Zhou H, Zhang H, Yu A, Xie J (2018) Association between sunlight exposure and risk of age-related macular degeneration: a meta-analysis. BMC Ophthalmol 18(1):331. https://doi.org/10.1186/s12886-018-1004-y
Acknowledgements
Medical writing and editorial assistant services have been provided by Ciencia y Deporte S.L. and covered by a Grant from Allergan.
Optretina reading group
Miguel A Zapata (MD, PhD)1,2; Gabriel Arcos (MD)3,4; Anniken Burés (MD,PhD)3,5; Alex Fonollosa (MD, PhD)3,6; Ignacio Flores-Moreno (MD, PhD)3,7; Roberto Gallego-Pinazo (MD, PhD)3,8; Estanislao Gutiérrez (MD, PhD)3,9; Andrea Oléñik (MD, PhD)3; Salvador Pastor (MD, PhD)3,10; Jorge Ruiz-Medrano (MD, PhD, FEBO)3,7; Cecilia Salinas(MD)3,5; Maximino Abraldes (MD, PhD)3,11
Affiliations
1Optretina. Barcelona (Spain)
2Hospital Vall Hebron. Barcelona (Spain)
3Retinal specialist, retina readers. Barcelona (Spain)
4AMEDICS, Barcelona (Spain)
5IMO, Instituto de Microcirugía Ocular, Barcelona (Spain)
6Hospital de Cruces, Bilbao (Vizcaya, Spain)
7Hospital Puerta de Hierro, Madrid (Spain)
8Oftalvist, Valencia (Spain)
9Hospital Universitario Virgen Macarena, Sevilla (Spain)
10Hospital Clínico Universitario, Valladolid (Spain)
11Complexo Hospitalario Universitario de Santiago de Compostela (A Coruña, Spain)
Funding
Support for this assistance was funded by Allergan S.A.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Statement of ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Hospital Vall d’Hebron (Barcelona, Spain).
Consent to participate
Patients were fully informed about the study objectives and its limitations, and written informed consent was obtained before any test were carried out.
Competing interests
Dr. Miguel A Zapata has received a Grant from Allergan during the conduct of the study for medical writing and editorial assistant services. All other authors declare that they have no conflict of interest in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Figure S1.
Prevalence of age-related macular degeneration (AMD) (any eye and any severity) in the different Spanish provinces. (PNG 98 kb)
Table S1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Zapata, M.A., Burés, A., Gallego-Pinazo, R. et al. Prevalence of age-related macular degeneration among optometric telemedicine users in Spain: a retrospective nationwide population-based study. Graefes Arch Clin Exp Ophthalmol 259, 1993–2003 (2021). https://doi.org/10.1007/s00417-021-05093-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05093-4