Abstract
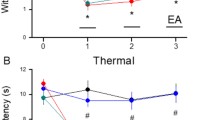
The pro-resolving mechanism is a recently described endogenous process that controls inflammation. The present study evaluated components of this mechanism, including annexin 1 (ANXA1) and the formyl peptide receptor 2/ALX (FPR2/ALX) receptor, in the antihyperalgesic effect induced by electroacupuncture (EA) in an animal model of persistent peripheral inflammation. Male Swiss mice underwent intraplantar (i.pl.) injection with complete Freund’s adjuvant (CFA). Mechanical hyperalgesia was assessed with von Frey monofilaments. Animals were treated with EA (2–10 Hz, ST36-SP6) or subcutaneous BML-111 injection (FPR2/ALX agonist) for 5 consecutive days. In a separate set of experiments, on the first and fifth days after CFA injection, animals received i.pl. WRW4 (FPR2/ALX antagonist) or naloxone (non-selective opioid receptor antagonist) before EA or BML-111 injection. Paw protein levels of FPR2/ALX and ANXA1 were evaluated on the second day after CFA injection by western blotting technique. EA and BML-111 reduced mechanical hyperalgesia. I.pl. naloxone or WRW4 prevented the antihyperalgesic effect induced by either EA or BML-111. EA increased ANXA1 but did not alter FPR2/ALX receptor levels in the paw. Furthermore, i.pl. pretreatment with WRW4 prevented the increase of ANXA1 levels induced by EA. This work demonstrates that the EA antihyperalgesic effect on inflammatory pain involves the ANXA1/FPR2/ALX pro-resolution pathway. This effect appears to be triggered by the activation of FPR2/ALX receptors and crosstalk communication with the opioid system.






Similar content being viewed by others
References
Ali U, Apryani E, Ahsan MZ, Shoaib RM, Ahmad KA, Wang YX (2019) Acupuncture/electroacupunture as an alternative in current opioid crisis. Chin J Integ Med 26:1–5. https://doi.org/10.1007/s11655-019-3175-7
Almeida RT, Galdino G, Perez AC, Silva G, Romero TR, Duarte ID (2017) ST36 electroacupuncture actives nNOS, iNOS and ATP-sensitive potassium channels to promote orofacial antinociception in rats. J Physiol Pharmacol 68:27–33
Ayoub SS, Yazid S, Flor RJ (2008) Increased susceptibility of annexin-A1 null mice to nociceptive pain is indicative of a spinal antinociceptive action of annexin-A1. Br J Pharmacol 154:1135–1142. https://doi.org/10.1038/bjp.2008.166
Berrueta L, Muskaj I, Olenich S, Butler T, Texugo GJ, Colas RA (2016) Stretching impacts inflammation resolution in connective tissue. J Cell Physiol 231:1621–1627. https://doi.org/10.1002/jcp.25263
Brack A, Rittner HL, Machelska H, Leder K, Mousa SA, Schäfer M (2004) Control of inflammatory pain by chemokine-mediated recruitment of opioid-containing polymorphonuclear cells. Pain 112:229–238. https://doi.org/10.1016/j.pain.2004.08.029
Ceccherelli F, Gagliardi G, Visentin R, Sandona F, Casale R, Giron G (1999) The effects of parachlorophenylalanine and naloxone on acupuncture and electroacupuncture modulation of capsaicin-induced neurogenic edema in the rat hind paw. A controlled blind study. Clin Exp Rheumatol 17:655–662
Chen WH, Hsieh CL, Huang CP, Lin TJ, Tzen JT, Ho TY, Lin YW (2013) Acid-sensing ion channel 3 mediates peripheral antihyperalgesia effects of acupuncture in miceinflammatory pain. J Biomed Sci 18:82. https://doi.org/10.1186/1423-0127-18-82
Chen L, Lv F, Pei L (2014) Annexin 1: a glucocorticoid-inducible protein that modulates inflammatory pain. Eur J Pain 18:338–347. https://doi.org/10.1002/j.1532-2149.2013.00373
Chiang N, Fierro IM, Gronert K, Serhan CN (2000) Activation of lipoxin A (4) receptors by aspirin-triggered lipoxins and select peptides evokes ligand-specific responses in inflammation. J Exp Med 191:1197–1208. https://doi.org/10.1084/jem.191.7.1197
Chiang N, Serhan CN, Dahlen SE, Drazen JM, Hay DW, Rovati GE, Shimizu T, Yokomizo T, Brink C (2006) The lipoxin receptor ALX: potent ligand-specific and stereoselective actions in vivo. Pharmacol Rev 58:463–487. https://doi.org/10.1124/pr.58.3.4
Chou R, Qaseem A, Snow V, Casey D, Cruz JTJR, Shekelle P, Owens DK (2007) Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 147:478–491. https://doi.org/10.7326/0003-4819-147-7-200710020-00006
Corder G, Tawfik VL, Wang D, Sypek EI, Low SA, Dickinson JR (2017) Loss of μ opioid receptor signaling in nociceptors, but not microglia, abrogates morphine tolerance without disrupting analgesia. Nat Med 23:164–173. https://doi.org/10.1038/nm.4262
Cui YH, Le Y, Gong W, Proost P, Van Damme J, Murphy WJ (2002) Bacterial lipopolysaccharide selectively up-regulates the function of the chemotactic peptide receptor formyl peptide receptor 2 in murine microglial cells. J Immunol 168:434–442. https://doi.org/10.4049/jimmunol.168.1.434
Da Silva MD, Bobinski F, Sato KL, Kolker SJ, Sluka KA, Santos AR (2015) IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol Neurobiol 51:19–31. https://doi.org/10.1007/s12035-014-8790-x
Dalpiaz A, Spisani S, Biondi C, Fabbri E, Nalli M, Ferretti ME (2003) Studies on human neutrophil biological functions by means of formyl-peptide receptor agonists and antagonists. Curr Drug Targets Immune Endocr Metabol Disord 3:33–42. https://doi.org/10.2174/1568008033340333
Dufton N, Hannon R, Brancaleone V, Dalli J, Patel HB, Gray M (2010) Anti-inflammatory role of the murine formyl-peptide receptor 2: ligand-specific effects on leukocyte responses and experimental inflammation. J Immunol 184:2611–2619. https://doi.org/10.4049/jimmunol.0903526
El Kebir D, Jozsef L, Khreiss T, Pan W, Petasis NA, Serhan CN, Filep JG (2007) Aspirin-triggered lipoxins override the apopto- sis-delaying action of serum amyloid A in human neutrophils: a novel mechanism for resolution of inflammation. J Immunol 179:616–622. https://doi.org/10.4049/jimmunol.179.1.616
Eskinazi DP, Jobst KA (1996) National Institutes of Health Office of Alternative Medicine-Food and Drug Administration Workshop on Acupuncture. J Altern Complement Med 2:3–6. https://doi.org/10.1089/acm.1996.2.3
Ferreira SH, Cunha FQ, Lorenzetti BB, Michelin MA, Perretti H, Flower RJ, Poole S (1997) Role of lipocortin-1 in the anti-hyperalgesic actions of dexamethasone. Br J Pharmacol 121:883–888. https://doi.org/10.1038/sj.bjp.0701211
Fierro IM, Colgan SP, Bernasconi G, Petasis NA, Clish CB, Arita M, Serhan CN (2003) Lipoxin A4 and aspirin-triggered 15-epi- lipoxin A4 inhibit human neutrophil migration: comparisons between synthetic 15 epimers in chemotaxis and transmigration with microvessel endothelial cells and epithelial cells. J Immunol 170:2688–2694. https://doi.org/10.4049/jimmunol.170.5.2688
Flower RJ (1988) Eleventh Gaddum memorial lecture. Lipocortin and the mechanism of action of the glucocorticoids. Br J Pharmacol 94:987–1015. https://doi.org/10.1111/j.1476-5381.1988.tb11614.x
Headland SE, Norling LV (2015) The resolution of inflammation: principles and challenges. Semin Immunol 27:149–160. https://doi.org/10.1016/j.smim.2015.03.014
Ho CF, Ismail NB, Koh JK, Gunaseelan S, Low YH, Ng YK (2018) Localisation of formyl-peptide receptor 2 in the rat central nervous system and its role in axonal and dendritic outgrowth. Neurochem Res 43:1587–1598. https://doi.org/10.1007/s11064-018-2573-0
Huang C, Huang ZQ, Hu ZP, Jiang SZ, Li HT, Han JS, Wan Y (2008) Electroacupuncture effects in a rat model of complete Freund’s adjuvant-induced inflammatory pain: antinociceptive effects enhanced and tolerance development accelerated. Neurochem Res 33:2107–2111. https://doi.org/10.1007/s11064-008-9721-x
Huang CP, Chen HN, Su HL, Hsieh CL, Chen WH, Lin YW (2013) Electroacupuncture reduces carrageenan- and CFA-induced inflammatory pain accompanied by changing the expression of Nav1.7 and Nav1.8, rather than Nav1.9, in mice dorsal root ganglia. Evid Based Complement Alternat Med 1:8. https://doi.org/10.1155/2013/312184
Ji RR, Chamessian A, Zhang YQ (2016) Pain regulation by non-neuronal cells and inflammation. Science 354:572–577. https://doi.org/10.1126/science.aaf8924
Kong J, Spaeth R, Cook A, Kirsch I, Claggett B, Vangel M, Gollub RL, Smoller JW, Kaptchuk TJ (2013) Are all placebo effects equal? Placebo pills, sham acupuncture, cue conditioning and their association. PLoS One 8:1–9. https://doi.org/10.1371/journal.pone.0067485
Lao L, Zhang RX, Zhang G, Wang X, Berman BM, Ren K (2004) A parametric study of electroacupuncture on persistent hyperalgesia and Fos protein expression in rats. Brain Res 1020:18–29. https://doi.org/10.1016/j.brainres.2004.01.092
Liao HY, Hsieh CL, Huang C, Lin YW (2017) Electroacupuncture attenuates CFA-induced inflammatory pain by suppressing Nav1.8 through S100B, TRPV1, opioid, and adenosine pathways in mice. Sci Rep 7:42531. https://doi.org/10.1038/srep42531
Liu XJ, Gingrich JR, Vargas-Caballero M, Dong YN, Sengar A, Beggs S (2008) Treatment of inflammatory and neuropathic pain by uncoupling Src from the NMDA receptor complex. Nat Med 14:1325–1332. https://doi.org/10.1038/nm.1883
Liu F, Fang JQ, Shao XM (2009) Influence of electroacupuncture on the expression of cyclooxygenase mRNA and protein in rats with air-pouch plus recombinant human IL-1beta induced inflammation at the back. Zhen Ci Yan Jiu 34:159–162
Maderna P, Cottell DC, Toivonen T (2010) FPR2/ALX receptor expression and internalization are critical for lipoxin A4 and annexin-derived peptide-stimulated phagocytosis. FASEB J 24:4240–4249. https://doi.org/10.1096/fj.10-159913
Mambretti EM, Kistner K, Mayer S, Massotte D, Kieffer BL, Hoffmann C (2016) Functional and structural characterization of axonal opioid receptors as targets for analgesia. Mol Pain 12:1–17. https://doi.org/10.1177/1744806916628734
Martins DF, Brito RN, Stramosk J, Batisti AP, Madeira F, Turnes BL (2015) Peripheral neurobiologic mechanisms of antiallodynic effect of warm water immersion therapy on persistent inflammatory pain. J Neurosci Res 93:157–166. https://doi.org/10.1002/jnr.23461
Mazzardo-Martins L, Salm DC, Winkelmann-Duarte EC, Ferreira JK, Lüdtke DD, Frech KP, Belmonte LAO, Horewicz VV, Piovezan AP, Cidral-Filho FJ, Moré AOO, Martins DF (2018) Electroacupuncture induces antihyperalgesic effect through endothelin-B receptor in the chronic phase of a mouse model of complex regional pain syndrome type I. Pflugers Arch 470:1829–1827. https://doi.org/10.1007/s00424-018-2192-2
Meotti FC, Missau FC, Ferreira J, Pizzolatti MG, Mizuzaki C, Nogueira CW (2006) Anti-allodynic property of flavonoid myricitrin in models of persistent inflammatory and neuropathic pain in mice. Biochem Pharmacol 72:1707–1713. https://doi.org/10.1007/s00424-018-2192-2
Migeotte I, Communi D, Parmentier M (2006) Formyl peptide receptors: a promiscuous subfamily of G protein-coupled receptors controlling immune immune responses. Cytokine Growth Factor Rev 17:501–519. https://doi.org/10.1016/j.cytogfr.2006.09.009
Mou H, Li Z, Kong Y, Deng B, Qian L, Wang JM, Le Y (2002) Proinflammatory stimulants promote the expression of a promiscuous G protein-coupled receptor, mFPR2, in microvascular endothelial cells. Inflammation 35:656–664. https://doi.org/10.1007/s10753-011-9358-9
Naciff JM, Kaetzel MA, Behbehani MM, Dedman JR (1996) Differential expression of annexins I-VI in the rat dorsal root ganglia and spinal cord. J Comp Neurol 368:356–370. https://doi.org/10.1002/(SICI)1096-9861(19960506)368:3<356::AID-CNE3>3.0.CO;2-4
Oehler B, Mohammadi M, Perpina Viciano C, Hackel D, Hoffmann C, Brack A (2017) Peripheral interaction of resolvin D1 and E1 with opioid receptor antagonists for antinociception in inflammatory pain in rats. Front Mol Neurosci 10:242. https://doi.org/10.3389/fnmol.2017.00242
Ouyang BS, Che JL, Gao J, Zhang Y, Li J, Yang HZ (2010) Effects of electroacupuncture and simple acupuncture on changes of IL-1, IL-4, IL-6 and IL-10 in peripheral blood and joint fluid in patients with rheumatoid arthritis. Zhongguo Zhen Jiu 30:840–844
Pei L, Zhang J, Zhao F, Su T, Wei H, Tian J, Li M, Shi J (2011) Annexin 1 exerts anti-nociceptive effects after peripheral inflammatory pain through formyl-peptide-receptor-like 1 in rat dorsal root ganglion. Br J Anaesth 107:948–958. https://doi.org/10.1093/bja/aer299
Perretti S, Di Giannuario A, De Felice M, Perretti M, Cirino G (2004) Stimulus-dependent specificity for annexin 1 inhibition of the inflammatory nociceptive response: the involvement of the receptor for formylated peptides. Pain 109:52–63. https://doi.org/10.1016/j.pain.2004.01.009
Piovezan AP, Batisti AP, Benevides MLACS, Turnes BL, Martins DF, Kanis L (2017) Hydroalcoholic crude extract of Casearia sylvestris Sw. reduces chronic post-ischemic pain by activation of pro-resolving pathways. J Ethnopharmacol 204:179–188. https://doi.org/10.1016/j.jep.2017.03.059
Rittner HL, Brack A, Machelska H, Mousa SA, Bauer M, Schäfer M, Stein C (2001) Opioid peptide-expressing leukocytes: identification, recruitment, and simultaneously increasing inhibition of inflammatory pain. Anesthesiology 95:500–508. https://doi.org/10.1097/00000542-200108000-00036
Rittner HL, Hackel D, Voigt P, Mousa S, Stolz A, Labuz D (2009) Mycobacteria attenuate nociceptive responses by formyl peptide receptor triggered opioid peptide release from neutrophils. PLoS Pathog 5:1–14. https://doi.org/10.1371/journal.ppat.1000362
Rodrigues AS (2009) The influence of Zusanli (E36) and Sanyinjiao (BP 6) acupuncture points on the development of thioacetamide-induced liver lesions in wistar rats. Doctoral dissertation at the Faculty of São Paulo. Faculty of Veterinary Medicine and Animal Science. Department of Surgery. https://doi.org/10.11606/T.10.2009.tde-30092010-154903
Sehhatie-Shafaie F, Kazemzadeh R, Amani F, Heshmat R (2013) The effect of acupressure on Sanyinjiao and Hugo points on labor pain in nulliparous women: a randomized clinical trial. J Caring Sci 2:123–129. https://doi.org/10.5681/jcs.2013.015
Sekido R, Ishimaru K, Sakita M (2003) Differences of electroacupuncture-induced analgesic: effect in normal and inflammatory conditions in rats. Am J Chin Med 31:955–965. https://doi.org/10.1142/S0192415X03001491
Serhan CN (2014) Pro-resolving lipid mediators are leads for resolution physiology. Nature 510:92–101. https://doi.org/10.1038/nature13479
Serhan CN, Levy BD (2018) Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. J Clin Invest 128:2657–2669. https://doi.org/10.1172/JCI97943
Serhan CN, Petasis NA (2011) Resolvins and protectins in inflammation resolution. Chem Rev 111:5922–5432. https://doi.org/10.1021/cr100396c
Silvério-Lopes SM (2008) Induced analgesic for eletroacupuncture: a retrospective boarding na frequency stimulation. FIEP Bulletin 2:308–393
Spahn V, Del Vecchio G, Labuz D, Rodriguez-Gaztelumendi A, Massaly N, Temp J (2017) A nontoxic pain killer designed by modeling of pathological receptor conformations. Science 355:966–969. https://doi.org/10.1126/science.aai8636
Spurr L, Nadkarni S, Pederzoli-Ribeil M, Goulding NJ, Perretti M, D’Acquisto F (2011) Comparative analysis of annexin A1-formyl peptide receptor 2/ALX expression in human leukocyte subsets. Int Immunopharmacol 11:55–66. https://doi.org/10.1016/j.intimp.2010.10.006
Stein C, Clark JD, Oh U (2009) Peripheral mechanisms of pain and analgesia. Brain Res Rev 60:90–113. https://doi.org/10.1016/j.brainresrev.2008.12.017
Sugimoto MA, Souza LP, Pinho V, Perretti M, Teixeira MM (2016) Resolution of inflammation: what controls its onset? Front Immunol 7:160. https://doi.org/10.3389/fimmu.2016.00160
Svensson CI, Zattoni M, Serhan CN (2007) Lipoxins and aspirin-triggered lipoxin inhibit inflammatory pain processing. J Exp Med 204:245–252. https://doi.org/10.1084/jem.20061826
Torres-Rosas R, Yehia G, Peña G, Mishra P, Del Rocio T-BM, Moreno-Eutimio MA, Arriaga-Pizano LA, Isibasi A, Ulloa L (2014) Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med 20:291–295. https://doi.org/10.1038/nm.3479
Wang Y, Gehringer R, Mousa SA, Hackel D, Brack A, Rittner HL (2014) CXCL10 controls inflammatory pain via opioid peptide-containing macrophages in electroacupuncture. PLoS One 9:1–12
Xiang XH, Chen YM, Zhang JM, Tian JH, Han JS, Cui CL (2014) Low- and high-frequency transcutaneous electrical acupoint stimulation induces different effects on cerebral μ-opioid receptor availability in rhesus monkeys. J Neurosci Res 92:555–563. https://doi.org/10.1371/journal.pone.0094696
Zhang R, Lao L, Ren K, Berman BM (2014) Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology 120:482–503. https://doi.org/10.1097/ALN.0000000000000101
Zhang J, Pan R, Zhou M, Tan F, Huang Z, Dong J (2018) Electroacupuncture as an adjunctive therapy for motor dysfunction in acute stroke survivors: a systematic review and meta-analyses. BMJ Open 8:1–11. https://doi.org/10.1136/bmjopen-2017-017153
Funding
This work was supported by grants from the National Council for Scientific and Technological Development (CNPq; grant number 430556/2018-7) and Foundation of Support for Research and Innovation of the State of Santa Catarina (FAPESC; grant number 2019TR73) and by the Coordination for the Higher Education (CAPES) and Unisul Scientific Initiation Program (PUIC), Brazil. DFM is supported by research fellowships from CNPq (309407/2017-6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vieira, C., Salm, D.C., Horewicz, V.V. et al. Electroacupuncture decreases inflammatory pain through a pro-resolving mechanism involving the peripheral annexin A1-formyl peptide receptor 2/ALX-opioid receptor pathway. Pflugers Arch - Eur J Physiol 473, 683–695 (2021). https://doi.org/10.1007/s00424-020-02502-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-020-02502-1