Abstract
Background
Difficulty scores (DSs) have been proposed to rate laparoscopic liver resection (LLR) technical difficulty increasing surgical safety. The aim of the study was to validate three DSs (Hasegawa, Halls and Kawaguchi) and compare their ability to predict technical difficulty and postoperative outcomes.
Materials and methods
All patients who underwent LLR from January 2006 to January 2019 were analyzed. Exclusion criteria were cyst fenestrations, thermal ablation, missing data for the computation of the DS and a follow-up < 90 days.
Results
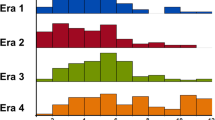
The population comprised 300 patients. The DS distribution in the study population was: Halls low 55 (18.3%), moderate 82 (27.3%), high 111 (37%) and extremely high 52 (17.3%); Hasegawa low 130 (43.3%), medium 105 (35%) and high 65 (21.7%); Kawaguchi Grade I 194 (64.7%), Grade II 47 (15.7%) and Grade III 59 (19.7%). Hasegawa and Kawaguchi showed the strongest correlation (r = 0.798, p < 0.001). Technical complexity, evaluated using the Pringle maneuver, Pringle time, blood loss and operative time, increased significantly with Hasegawa and Kawaguchi score classes (p < 0.001 for all comparisons). None of the scores properly stratified postoperative complications. The highest Kawaguchi (23.7% grade III vs. 13.7% grades I and II, p = 0.057) and Hasegawa (24.6% high vs. 13.2% low/medium, p = 0.025) classes had a higher overall morbidity rate than medium–low ones.
Conclusions
Kawaguchi and Hasegawa scores predicted LLR’s technical difficulty. None of the scores discriminated the postoperative complication risk of low classes compared with medium ones.



Similar content being viewed by others
References
Schostek S, Zimmermann M, Schurr MO, Prosst RL (2015) Design and performance of a low-cost telemetric laparoscopic tactile grasper. Surg Innov 23(3):291–297. https://doi.org/10.1177/1553350615615440
Coelho FF, Kruger JA, Fonseca GM, Araújo RL, Jeismann VB, Perini MV, Lupinacci RM, Cecconello I, Herman P (2016) Laparoscopic liver resection: experience based guidelines. World J Gastrointest Surg 8(1):5. https://doi.org/10.4240/wjgs.v8.i1.5
Wong-Lun-Hing EM, van Dam RM, van Breukelen GJ, Tanis PJ, Ratti F, van Hillegersberg R, Slooter GD, de Wilt JH, Liem MS, de Boer MT, Klaase JM, Neumann UP, Aldrighetti LA, Dejong CH, ORANGE II Collaborative Group (2017) Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study). Br J Surg 104(5):525–535. https://doi.org/10.1002/bjs.10438
Fretland ÅA, Kazaryan AM, Bjørnbeth BA, Flatmark K, Andersen MH, Tønnessen TI, Bjørnelv GM, Fagerland MW, Kristiansen R, Øyri K, Edwin B (2015) Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet study): study protocol for a randomized controlled trial. Trials 16:73. https://doi.org/10.1186/s13063-015-0577-5
Hallet J, Pessaux P, Beyfuss KA, Jayaraman S, Serrano PE, Martel G, Coburn NG, Piardi T, Mahar AL (2019) Critical appraisal of predictive tools to assess the difficulty of laparoscopic liver resection: a systematic review. Surg Endosc 33(2):366–376. https://doi.org/10.1007/s00464-018-6479-3
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, OʼRourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection a report from the second international consensus conference held in morioka. Ann Surg 261(4):619–629. https://doi.org/10.1097/SLA.0000000000001184
Tong Y, Li Z, Ji L, Wang Y, Wang W, Ying J, Cai X (2018) A novel scoring system for conversion and complication in laparoscopic liver resection. Hepatobiliary Surg Nutr 7(6):454–465. https://doi.org/10.21037/hbsn.2018.10.09
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21(10):745–753. https://doi.org/10.1002/jhbp.166
Troisi RI, Montalti R, Van Limmen JG, Cavaniglia D, Reyntjens K, Rogiers X, De Hemptinne B (2014) Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford). 16(1):75–82. https://doi.org/10.1111/hpb.12077
Lee SY, Goh BKP, Sepideh G, Allen JC, Merkow RP, Teo JY, Chandra D, Koh YX, Tan EK, Kam JH, Cheow PC, Chow PKH, Ooi LLPJ, Chung AYF, D'Angelica MI, Jarnagin WR, Peter Kingham T, Chan CY (2019) Laparoscopic liver resection difficulty score-a validation study. J Gastrointest Surg 23(3):545–555. https://doi.org/10.1007/s11605-018-4036-y
Im C, Cho JY, Han HS, Yoon YS, Choi Y, Jang JY, Choi H, Jang JS, Kwon SU (2017) Validation of difficulty scoring system for laparoscopic liver resection in patients who underwent laparoscopic left lateral sectionectomy. Surg Endosc 31(1):430–436. https://doi.org/10.1007/s00464-016-4994-7
Periyasamy M, Cho JY, Ahn S, Han HS, Yoon YS, Choi Y, Jang JS, Kwon SU, Kim S, Choi JK, Guro H (2017) Prediction of surgical outcomes of laparoscopic liver resections for hepatocellular carcinoma by defining surgical difficulty. Surg Endosc 31(12):5209–5218. https://doi.org/10.1007/s00464-017-5589-7
Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagiri H, Umemura A, Makabe K, Sasaki A (2017) A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 31(12):5356–5363. https://doi.org/10.1007/s00464-017-5616-8
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267(1):13–17. https://doi.org/10.1097/SLA.0000000000002176
Halls MC, Berardi G, Cipriani F, Barkhatov L, Lainas P, Harris S, D'Hondt M, Rotellar F, Dagher I, Aldrighetti L, Troisi RI, Edwin B, Abu Hilal M (2018) Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br J Surg. 105(9):1182–1191. https://doi.org/10.1002/bjs.10821
Ferrero A, Lo Tesoriere R, Russolillo N (2019) Ultrasound liver map technique for laparoscopic liver resections. World J Surg 43(10):2607–2611. https://doi.org/10.1007/s00268-019-05046-3
Ferrero A, Russolillo N, Langella S, Forchino F, Stasi M, Fazio F, Lo Tesoriere R (2019) Ultrasound liver map technique for laparoscopic liver resections: perioperative outcomes are not impaired by technical complexity. Updates Surg 71(1):49–56. https://doi.org/10.1007/s13304-019-00646-z
Russolillo N, D'Eletto M, Langella S, Perotti S, Lo Tesoriere R, Forchino F, Ferrero A (2016) Role of laparoscopic ultrasound during diagnostic laparoscopy for proximal biliary cancers: a single series of 100 patients. Surg Endosc 30(3):1212–1218. https://doi.org/10.1007/s00464-015-4333-4
Ferrero A, Lo Tesoriere R, Russolillo N, Viganò L, Forchino F, Capussotti L (2015) Ultrasound-guided laparoscopic liver resections. Surg Endosc 29(4):1002–1005. https://doi.org/10.1007/s00464-014-3762-9
Viganò L, Jaffary SA, Ferrero A, Russolillo N, Langella S, Capussotti L (2011) Liver resection without pedicle clamping: feasibility and need for “ salvage clamping ”. Looking for the right clamping policy. Analysis of 512 consecutive resections. J Gastrointest Surg 15(10):1820–1828. https://doi.org/10.1007/s11605-011-1625-4
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Büchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149(5):713–724. https://doi.org/10.1016/j.surg.2010.10.001
Strasberg SM, Belghiti J, Clavien P-A, Gadzijev E, Garden JO, Lau W-Y, Makuuchi M, Strong RW, Terminology Commitee of the International Hepato-Pancreato-Biliary Association (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford) 2(3):333–339. https://doi.org/10.1016/S1365-182X(17)30755-4
Farges O, Jagot P, Kirstetter P, Marty J, Belghiti J (2002) Prospective assessment of the safety and benefit of laparoscopic liver resections. J Hepatobiliary Pancreat Surg 9(2):242–248. https://doi.org/10.1007/s005340200026
Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP (2011) Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 13(5):295–308. https://doi.org/10.1111/j.1477-2574.2011.00295.x
Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G (2010) Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 102(1):82–86. https://doi.org/10.1002/jso.21541
Xie SM, Xiong JJ, Liu XT, Chen HY, Iglesia-García D, Altaf K, Bharucha S, Huang W, Nunes QM, Szatmary P, Liu XB (2017) Laparoscopic versus open liver resection for colorectal liver metastases: a comprehensive systematic review and meta-analysis. Sci Rep 7(1):1012. https://doi.org/10.1038/s41598-017-00978-z
Robles-Campos R, Lopez-Lopez V, Brusadin R, Lopez-Conesa A, Gil-Vazquez PJ, Navarro-Barrios Á, Parrilla P (2019) Open versus minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc. https://doi.org/10.1007/s00464-019-06679-0
Halls MC, Alseidi A, Berardi G, Cipriani F, Van der Poel M, Davila D, Ciria R, Besselink M, D'Hondt M, Dagher I, Alrdrighetti L, Troisi RI, Abu Hilal M (2019) A Comparison of the learning curves of laparoscopic liver surgeons in differing stages of the IDEAL paradigm of surgical innovation: standing on the shoulders of pioneers. Ann Surg 269(2):221–228. https://doi.org/10.1097/SLA.0000000000002996
McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, Nicholl J, Collaboration B, Aronson JK, Barkun JS, Blazeby JM, Boutron IC, Campbell WB, Clavien PA, Cook JA, Ergina PL, Feldman LS, Flum DR, Maddern GJ, Nicholl J, Reeves BC, Seiler CM, Strasberg SM, Meakins JL, Ashby D, Black N, Bunker J, Burton M, Campbell M, Chalkidou K, Chalmers I, de Leval M, Deeks J, Ergina PL, Grant A, Gray M, Greenhalgh R, Jenicek M, Kehoe S, Lilford R, Littlejohns P, Loke Y, Madhock R, McPherson K, Meakins J, Rothwell P, Summerskill B, Taggart D, Tekkis P, Thompson M, Treasure T, Trohler U, Vandenbroucke J (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374(9695):1105–1112. https://doi.org/10.1016/S0140-6736(09)61116-8
Geersing GJ, Bouwmeester W, Zuithoff P, Spijker R, Leeflang M, Moons KG (2012) Search filters for finding prognostic and diagnostic prediction studies in Medline to enhance systematic reviews. PLoS ONE 7(2):e32844. https://doi.org/10.1371/journal.pone.0032844
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Nadia Russolillo, Cecilia Maina, Francesco Fleres, Serena Langella, Roberto Lo Tesoriere, and Alessandro Ferrero have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Russolillo, N., Maina, C., Fleres, F. et al. Comparison and validation of three difficulty scoring systems in laparoscopic liver surgery: a retrospective analysis on 300 cases. Surg Endosc 34, 5484–5494 (2020). https://doi.org/10.1007/s00464-019-07345-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07345-1