Abstract
Background
The purpose of this study was to evaluate the effect of 3D visualization applied to laparoscopic appendectomy (LA) performed by young surgeons (YS). We considered both operative features and clinical outcomes, aiming to highlight the benefits that this technology could bring to novice surgeons and their laparoscopic training.
Methods
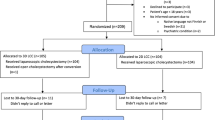
All the surgical procedures were performed by residents who had performed less than 20 appendectomies prior to the beginning of the study under the supervision of an expert surgeon. At the time of enrolment patients were randomized into two arms: Experimental arm (EA): laparoscopic appendectomy performed with laparoscopic 3D vision technology. Control arm (CA): laparoscopic appendectomy performed with the "standard" 2D technology. The primary endpoint was to find any statistically significant difference in operative time between the two arms. Differences in conversion rate, intra-operative complications, post-operative complications and surgeons’ operative comfort were considered as secondary endpoints.
Results
We randomized 135 patients into the two study arms. The two groups were homogeneous for demographic characteristics, BMI and ASA scores. The characteristics of clinical presentation and anatomical position showed no significant difference. The operative time was longer in the CA (57.5 vs. 49.6 min, p = 0.048, 95% CI). In the subgroup of complicated appendicitis, this trend toward inferior operative time was confirmed without reaching statistical significance (2D = 60 min, 3D = 49.5 min, p = 0.082 95% CI).
No intra-operative complications were observed in either group. The conversion rate was 5.6% (4 patients) in the 2D group and 4.6% (3 patients) in 3D group.
Conclusion
The utilization of 3D laparoscopy was associated with reduction in operative time without influencing other parameters, in particular without altering the safety profile of the procedure.



Similar content being viewed by others
References
Di Saverio S, Birindelli A, Kelly MD et al (2016) WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 11:34
Addiss DG, Shaffer N, Fowler BS et al (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132(5):910–925
Jones DB, Jerome D, Brewer RN et al (1996) The influence of three-dimensional video system on laparoscopic task performance. Surg Laparosc Endosc 6(3):191–197
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study of influence of two-dimensional versus threedimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251
Mashiach R, Mezhybovsky V, Nevler A et al (2014) Three-dimensional imaging improves surgical skill performance in a laparoscopic test model for both experienced and novice laparoscopic surgeons. Surg Endosc 28:3489–3493
Cicione A, Autorino R, Laguna MP et al (2015) Three-dimensional technology facilitates surgical performance of novice laparoscopy surgeons: a quantitative assessment on a porcine kidney model. Urology 85:1252–1256
Chiu CJ, Prabhu KL, Tan-Tam CC et al (2015) Using three-dimensional laparoscopy as a novel training tool for novice trainees compared with two-dimensional laparoscopy. Am J Surg 209:824–827
Wagner OJ, Hagen M, Kurmann A et al (2012) Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 26(10):2961–2968
Bilgen K, Ustun M, Karakahya M et al (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23(2):180–183
Sahu D, Mathew MJ, Reddy PK (2014) Laparoscopy-help or hype; initial experience of a tertiary health centre. J Clin Diagn Res 8(7):NC01–NC03
Currò G, La Malfa G, Caizzone A et al (2015) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery A single-surgeon prospective randomized comparative study. Obes Surg 25(11):2120–2124
Currò G, La Malfa G, Lazzara L et al (2015) Three-dimensional versus two-dimensional laparoscopic cholecystectomy: is surgeon experience relevant? J Laparoendosc Adv Surg Tech 25(7):566–570
Agrusa A, Di Buono G, Chianetta D et al (2016) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: a case–control study. Int J Surg 28(suppl1):114–117
Velayutham V, Fucks D, Nomi T et al (2016) 3D visualization reduces operating time when compared to highdefinition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc 30:147–153
Medeiros LR, Stein AT, Fachel J et al (2008) Laparoscopy versus laparotomy for benign ovarian tumor: a systematic review and meta-analysis. Int J Gynecol Cancer 18(3):387–399
Sørensen SMD, Savran MM, Konge L et al (2016) Three-dimensional versus two-dimensional vision in laparoscopy: a systematic review. Surg Endosc 30:11–23
Özsoy M, Kallidonis P, Kyriazis I (2015) Novice surgeons: do they benefit from 3D laparoscopy? Lasers Med Sci 30:1325–1333
Cicione A, Autorino R, Breda A et al (2013) Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82(6):1444–1450
Storz P, Buess GF, Kunert W et al (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc Other Interv Tech 26(5):1454–1460
Ashraf A, Collins D, Whelan M et al (2015) Three-dimensional (3D) simulation versus two-dimensional (2D) enhances surgical skills acquisition in standardised laparoscopic tasks: a before and after study. Int J Surg 14:12–16
Leite M, Carvalho AF (2016) Costa P et al Assessment of laparoscopic skills performance: 2D versus 3D vision and classic instrument versus new hand-held robotic device for laparoscopy. Surg Innov 23(1):52–61
Axt S (2016) Influence of the endoscope’s stereoscopic base on performance in standardized laparoscopic tasks: a prospective randomized controlled trial. Surg Endosc Other Interv Tech 30:S74
Buia A, Stockhausen F, Filmann N et al (2017) 3D vs 2D imaging in laparoscopic surgery—an advantage? Results of standardised black box training in laparoscopic surgery. Langenbeck’s Arch Surg 402(1):167–171
Poudel S, Kurashima Y, Watanabe Y et al (2017) Impact of 3D in the training of basic laparoscopic skills and its transferability to 2D environment: a prospective randomized controlled trial. Surg Endosc Other Interv Tech 31(3):1111–1118
Sakata S, Grove PM, Hill A et al (2017) Impact of simulated three-dimensional perception on precision of depth judgements, technical performance and perceived workload in laparoscopy. Br J Surg 104(8):1097–1106
Honeck P, Wendt-Nordahl G, Rassweiler J et al (2012) Three-dimensional laparoscopic imaging improves surgical performance on standardized ex-vivo laparoscopic tasks. J Endourol 26(8):1085–1088
Yalcin S, Kibar Y, Ozgok IY (2014) Which system is better for beginners’ laparoscopy training? glasses based full-hd 3D monitor systems or standard (full-hd 2D) monitor systems. J Endourol 28:A271
Gomes CA, Nunes TA, Fonseca Chebli JM et al (2012) Laparoscopy grading system of acute appendicitis: new insight for future trials. Surg Laparosc Endosc Percutan Tech 22(5):463–466
Likert R (1932) A technique for the measurement of attitudes. Arch Psychol 140:55
Becker H, Melzer A, Schurr MO, Buess G (1993) 3-D video techniques in endoscopic surgery. Endosc Surg Allied Technol 1(1):40–46
Fergo C, Burcharth J, Pommergaard HC et al (2017) Three-dimensional laparoscopy vs. 2-dimensional laparoscopy with high-definition technology for abdominal surgery: a systematic review. Am J Surg 213:159–170
Vettoretto N, Foglia E, Ferrario L et al (2018) Why laparoscopists may opt for three-dimensional view: a summary of the full HTA report on 3D versus 2D laparoscopy by S.I.C.E. (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie). Surg Endosc 32:2986–2993
Arezzo A, Vettoretto N, Francis NK et al (2019) The use of 3D laparoscopic imaging systems in surgery: EAES consensus development conference 2018. Surg Endosc 10:3251–3274
Schwab K, Smith R, Brown V et al (2017) Evolution of stereoscopic imaging in surgery and recent advances. World J Gastrointest Endosc 9(8):368–377
NCT03143426 Does 3D Visualisation Improve Performance of Laparoscopic Cholecystectomy by Junior Surgeons?
Alaraimi BS, Sarker SJ, Elbakbak WS, Makkiyah S, Al-Marzouq A, Goriparthi RG et al (2013) Laparoscopic skills performance with stereoscopic vision as compared to the standard laparoscopic vision: a randomised control study. Int J Surg 11(8):593–594
Bohr I, Read JC (2013) Stereoacuity with Frisby and revised FD2 stereo tests. PLoS ONE ONE 8(12):e82999
Bosten JM, Goodbourn PT, Lawrance-Owen AJ, Bargary G, Hogg RE, Mollon JD (2015) A population study of binocular function. Vision Res 110(Pt A):34–50
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs Emanule Botteri, Monica Ortenzi, Giovanni Alemanno, Alessio Giordano, Elisabetta Travaglio, Cecilia Turolo, Simone Castiglioni, Elio Treppiedi, Edoardo Rosso, Andrea Gattolin, Valerio Caracino, Paolo Prosperi, Andrea Valeri, Mario Guerrieri and Nereo Vettoretto have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Botteri, E., Ortenzi, M., Alemanno, G. et al. Laparoscopic Appendectomy Performed by junior SUrgeonS: impact of 3D visualization on surgical outcome. Randomized multicentre clinical trial. (LAPSUS TRIAL). Surg Endosc 35, 710–717 (2021). https://doi.org/10.1007/s00464-020-07436-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07436-4