Abstract
Background
Endoscopic submucosal dissection (ESD) is a prominent minimally invasive operative technique for treating early gastrointestinal tumors but can result in postoperative bleeding. We conducted a randomized controlled trial to determine whether increasing blood pressure under hemostasis during gastric ESD to identify potential bleeding spots reduces the risk of post-ESD bleeding.
Methods
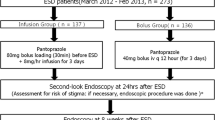
In this randomized, controlled, single-blinded clinical trial, 309 patients with early gastric cancer who were admitted to a hospital to undergo ESD were recruited from March 2017 to February 2018 and were randomized into intervention and control groups. In the control group, patients underwent normal ESD. In the intervention group, we increased patients’ blood pressure to 150 mmHg for 5 min using a norepinephrine pump (0.05 μg/kg/min initial dose) after the specimen was extracted during the ESD operation to identify and coagulate potential bleeding spots with hot biopsy forceps. Our primary outcome was the incidence of postoperative bleeding over 60-day follow-up.
Results
The incidence of post-ESD bleeding was lower in the intervention group (1.3%, 2/151) than in the control group (10.1%, 16/158, p = 0.01). Deeper tumor invasion was associated with a higher risk of post-ESD bleeding (5.3% in mucosal/submucosal layer 1 group vs. 12.5% in submucosal layer 2/muscularis propria group, p < 0.001). Multi-factor but not univariate analysis showed that proton pump inhibitor administration three times per day may be a better choice than twice per day.
Conclusion
Increasing blood pressure under hemostasis during ESD to identify and coagulate potential bleeding spots could reduce the risk of delayed bleeding after gastric ESD.



Similar content being viewed by others
References
Tanabe S, Ishido K, Higuchi K et al (2014) Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a retrospective comparison with conventional endoscopic resection in a single center. Gastric Cancer 17:130–136
Fujiya M, Tanaka K, Dokoshi T et al (2015) Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 81:583–595
Park YM, Cho E, Kang HY et al (2011) The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc 25:2666–2677
Lim JH, Kim SG, Kim JW et al (2012) Do antiplatelets increase the risk of bleeding after endoscopic submucosal dissection of gastric neoplasms? Gastrointest Endosc 75:719–727
Isomoto H, Shikuwa S, Yamaguchi N et al (2009) Endoscopic submucosal dissection for early gastric cancer: a largescale feasibility study. Gut 58:331–336
Goto O, Fujishiro M, Oda I et al (2012) A multicenter survey of the management after gastric endoscopic submucosal dissection related to postoperative bleeding. Dig Dis Sci 57:435–439
Koh R, Hirasawa K, Yahara S, Oka H et al (2013) Antithrombotic drugs are risk factors for delayed postoperative bleeding after endoscopic submucosal dissection for gastric neoplasms. Gastrointest Endosc 78:476–483
Okada K, Yamamoto Y, Kasuga A et al (2011) Risk factors for delayed bleeding after endoscopic submucosal dissection for gastric neoplasm. Surg Endosc 25:98–107
Toyokawa T, Inaba T, Omote S et al (2012) Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: analysis of 1123 lesions. J Gastroenterol Hepatol 27(5):907–912
Ebi M, Shimura T, Nishiwaki H et al (2014) Management of systolic blood pressure after endoscopic submucosal dissection is crucial for prevention of post-ESD gastric bleeding. Eur J Gastroenterol Hepatol 26(5):504–509
Oka S, Tanaka S, Kaneko I et al (2006) Advantage of endoscopic submucosal dissection compared with EMR for early gastric cancer. Gastrointest Endosc 64:877–883
Kataoka Y, Tsuji Y, Hirasawa K et al (2019) Endoscopic tissue shielding to prevent bleeding after endoscopic submucosal dissection: a prospective multicenter randomized controlled trial. Endoscopy 51(7):619–627
Takizawa K, Oda I, Gotoda T et al (2008) Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection: an analysis of risk factors. Endoscopy 40:179–183
Goto O, Fujishiro M, Kodashima S et al (2010) A second-look endoscopy after endoscopic submucosal dissection for gastric epithelial neoplasm may be unnecessary: a retrospective analysis of postendoscopic submucosal dissection bleeding. Gastrointest Endosc 71:241–248
Chung IK, Lee JH, Lee SH et al (2009) Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc 69:1228–1235
Nakamura M, Nishikawa J, Hamabe K et al (2012) Risk factors for delayed bleeding from endoscopic submucosal dissection of gastric neoplasms. Scand J Gastroenterol 47:1108–1114
Yoon JH, Kim YJ, Lee KN et al (2019) Effect on bleeding prevention of an intravenous proton pump inhibitor during the fasting period after endoscopic submucosal dissection: a prospective, randomized, double-blind, placebo-controlled trial. J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04466-9
Dumoulin FL, Hildenbrand R (2019) Endoscopic resection techniques for colorectal neoplasia: current developments. World J Gastroenterol 25(3):300–307
Higashiyama M, Oka S, Tanaka S et al (2011) Risk factors for bleeding after endoscopic submucosal dissection of gastric epithelial neoplasm. Dig Endosc 23:290–295
Suzuki S, Chino A, Kishihara T et al (2014) Risk factors for bleeding after endoscopic submucosal dissection of colorectal neoplasms. World J Gastroenterol 20:1839–1845
Matsumura T, Arai M, Maruoka D et al (2014) Risk factors for early and delayed post-operative bleeding after endoscopic submucosal dissection of gastric neoplasms, including patients with continued use of antithrombotic agents. BMC Gastroenterol 14:172
Kataoka Y, Tsuji Y, Sakaguchi Y et al (2016) Bleeding after endoscopic submucosal dissection: risk factors and preventive methods. World J Gastroenterol 22(26):5927–5935
Kawano S, Okada H, Kawahara Y et al (2011) Proton pump inhibitor dose-related healing rate of artificial ulcers after endoscopic submucosal dissection: a prospective randomized controlled trial. Digestion 84(1):46–53
Ko J, Kim SJ, Kang DH et al (2019) Dose-related healing of artificial ulcers after endoscopic submucosal dissection using esomeprazole: a randomized controlled study. Medicine (Baltimore) 98(20):e15701
Lee JY, Kim CG, Cho S-J et al (2017) Is the reinitiation of antiplatelet agents safe at 1 week after gastric endoscopic submucosal dissection? Assessment of bleeding risk using the Forrest classification. Gut Liver 11(4):489–96
Arai M, Matsumura T, Okimoto K et al (2014) Two-week treatment with proton pump inhibitor is sufficient for healing post endoscopic submucosal dissection ulcers. World J Gastroenterol 20(43):16318–16322
Tsuji Y, Ohata K, Ito T et al (2010) Risk factors for bleeding after endoscopic submucosal dissection for gastric lesions. World J Gastroenterol 16:2913–2917
Funding
This study was supported by the grants from the Natural Science Foundation of Shanghai (Grant No. 18441901100) and the National Natural Science Foundation of China (Grant No. 82000623).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Drs. Sheng-Li Lin, Ping-Ting Gao, Wen-Kai Ni, Quan-Lin Li, Wei-Feng Chen, Yi-Qun Zhang, Jian-Wei Hu, Wen-Zheng Qin, Ming-Yan Cai, Zhong Ren, Yun-Shi Zhong, Li-Qing Yao, Shi-Yao Chen, Mei-Dong Xu, Li-Li Ma, and Ping-Hong Zhou have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, SL., Gao, PT., Ni, WK. et al. Controlled hypertension under hemostasis prevents post-gastric endoscopic submucosal dissection bleeding: a prospective randomized controlled trial. Surg Endosc 35, 5675–5685 (2021). https://doi.org/10.1007/s00464-020-08256-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08256-2