Abstract
Objectives
When bone filling materials are applied onto the periodontal tissues in vivo, they interact with the injured periodontal ligament (PDL) tissue and modulate its activity. This may lead to mesenchymal stem cells (MSCs) recruitment from bone marrow and initiate bone regeneration. Our hypothesis is that the filling materials affect PDL cells and MSCs functional activities by modulating PDL C5a secretion and subsequent MSCs proliferation and recruitment.
Materials and methods
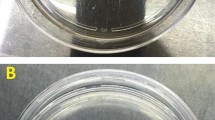
Materials’ extracts were prepared from 3 bone-grafting materials: Gen-Os® of equine and porcine origins and bovine Bio-Oss®. Expression and secretion of C5a protein by injured PDL cells were investigated by RT-PCR and ELISA. MSCs proliferation was analyzed by MTT assay. C5a binding to MSCs C5aR and its phosphorylation was studied by ELISA. C5a implication in MSCs recruitment toward injured PDL cells was investigated using Boyden chambers.
Results
MSCs proliferation significantly increased with Gen-Os® materials but significantly decreased with Bio-Oss®. C5a secretion slightly increased with Bio-Oss® while its level doubled with Gen-Os® materials. C5a fixation on MSCs C5aR and its phosphorylation significantly increased with Gen-Os® materials but not with Bio-Oss®. MSCs recruitment toward injured PDL cells increased with the three materials but was significantly higher with Gen-Os® materials than with Bio-Oss®. Adding C5a antagonist inhibited MSCs recruitment demonstrating a C5a-mediated migration.
Conclusions
Injured PDL cells secrete C5a leading MSCs proliferation and recruitment to the PDL injured cells. Gen-Os® materials enhanced both C5a secretion by injured PDL cells and MSCs recruitment. Bio-Oss® inhibited MSCs and was less efficient than Gen-Os® materials in inducing MSCs recruitment.
Clinical relevance
Within the limits of this study in vitro, Gen-Os® filling materials have a higher potential than Bio-Oss® on MSCs proliferation and C5a-dependent recruitment to the PDL injury site and the subsequent bone regeneration.





Similar content being viewed by others
References
Tan WL, Wong TLT, Wong MCM, Lang NP (2012) A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 23:1–21. https://doi.org/10.1111/j.1600-0501.2011.02375.x
Jamjoom A, Cohen RE (2015) Grafts for ridge preservation. J Funct Biomater 6:833–848. https://doi.org/10.3390/jfb6030833
Bassir S, Alhareky M, Wangsrimongkol B, Jia Y, Karimbux N (2018) Systematic review and meta-analysis of hard tissue outcomes of alveolar ridge preservation. Int J Oral Maxillofac Implants 33:979–994. https://doi.org/10.11607/jomi.6399
Barone A, Aldini NN, Fini M, Giardino R, Calvo Guirado JL, Covani U (2008) Xenograft versus extraction alone for ridge preservation after tooth removal: a clinical and histomorphometric study. J Periodontol 79:1370–1377. https://doi.org/10.1902/jop.2008.070628
Cortellini P (2000) Tonetti MS (2015) Clinical concepts for regenerative therapy in intrabony defects. Periodontol 68:282–307. https://doi.org/10.1111/prd.12048
Giuliani A, Iezzi G, Mazzoni S, Piattelli A, Perrotti V, Barone A (2018) Regenerative properties of collagenated porcine bone grafts in human maxilla: demonstrative study of the kinetics by synchrotron radiation microtomography and light microscopy. Clin Oral Investig 22:505–513. https://doi.org/10.1007/s00784-017-2139-6
Alfonsi F, Borgia V, Iezzi G et al (2017) Molecular, cellular and pharmaceutical aspects of filling biomaterials during the management of extraction sockets. Curr Pharm Biotechnol 18:64–75. https://doi.org/10.2174/1389201018666161223152607
Lin W, Xu L, Zwingenberger S, Gibon E, Goodman SB, Li G (2017) Mesenchymal stem cells homing to improve bone healing. J Orthop Transl 9:19–27. https://doi.org/10.1016/j.jot.2017.03.002
Wang L, Li Y, Chen J et al (2002) Ischemic cerebral tissue and MCP-1 enhance rat bone marrow stromal cell migration in interface culture. Exp Hematol 30:831–836. https://doi.org/10.1016/S0301-472X(02)00829-9
Puré E, Cuff CA (2001) A crucial role for CD44 in inflammation. Trends Mol Med 7:213–221. https://doi.org/10.22203/eCM.v026a09
Hemeda H, Jakob M, Ludwig A-K et al (2010) Interferon-gamma and tumor necrosis factor-alpha differentially affect cytokine expression and migration properties of mesenchymal stem cells. Stem Cells Dev 19:693–706. https://doi.org/10.1089/scd.2009.0365
Liu J, Kerns DG (2014) Mechanisms of guided bone regeneration: a review. Open Dent J 8:56–65. https://doi.org/10.2174/1874210601408010056
Mijiritsky E, Ferroni L, Gardin C et al (2017) Porcine bone scaffolds adsorb growth factors secreted by MSCs and improve bone tissue repair. Materials 10:1054. https://doi.org/10.3390/ma10091054
Murphy CM, O’Brien FJ, Little DG, Schindeler A (2013) Cell-scaffold interactions in the bone tissue engineering triad. Eur Cell Mater 26:120–132. https://doi.org/10.22203/eCM.v026a09
Ignatius A, Ehrnthaller C, Brenner RE et al (2011) The anaphylatoxin receptor C5aR is present during fracture healing in rats and mediates osteoblast migration in vitro: The Journal of Trauma: Injury. Infect Crit Care 71:952–960. https://doi.org/10.1097/TA.0b013e3181f8aa2d
Ricklin D, Hajishengallis G, Yang K, Lambris JD (2010) Complement: a key system for immune surveillance and homeostasis. Nat Immunol 11:785–797. https://doi.org/10.1038/ni.1923
Giannini E, Boulay F (1995) Phosphorylation, dephosphorylation, and recycling of the C5a receptor in differentiated HL60 cells. J Immunol 154:4055–4064
Schraufstatter IU, Discipio RG, Zhao M, Khaldoyanidi SK (2009) C3a and C5a are chemotactic factors for human mesenchymal stem cells, which cause prolonged ERK1/2 phosphorylation. J Immunol 182:3827–3836. https://doi.org/10.4049/jimmunol.0803055
Chmilewsky F, Jeanneau C, Laurent P, Kirschfink M, About I (2013) Pulp progenitor cell recruitment is selectively guided by a C5a gradient. J Dent Res 92:532–539. https://doi.org/10.1177/0022034513487377
Chmilewsky F, Jeanneau C, Laurent P, About I (2014) Pulp fibroblasts synthesize functional complement proteins involved in initiating dentin-pulp regeneration. Am J Pathol 184:1991–2000. https://doi.org/10.1016/j.ajpath.2014.04.003
Li K, Sacks SH, Zhou W (2007) The relative importance of local and systemic complement production in ischaemia, transplantation and other pathologies. Mol Immunol 44:3866–3874. https://doi.org/10.1016/j.molimm.2007.06.006
Jeanneau C, Rufas P, Rombouts C et al (2015) Can pulp fibroblasts kill cariogenic bacteria? Role of complement activation. J Dent Res 94:1765–1772. https://doi.org/10.1177/0022034515611074
Rombouts C, Jeanneau C, Camilleri J, Laurent P, About I (2016) Characterization and angiogenic potential of xenogeneic bone grafting materials: role of periodontal ligament cells. Dent Mater J 35:900–907. https://doi.org/10.4012/dmj.2016-005
Mathieu S, Jeanneau C, Sheibat-Othman N et al (2013) Usefulness of controlled release of growth factors in investigating the early events of dentin-pulp regeneration. J Endod 39:228–235. https://doi.org/10.1016/j.joen.2012.11.007
Jia M, Shi Z, Yan X et al (2018) Insulin and heparin-binding epidermal growth factor-like growth factor synergistically promote astrocyte survival and proliferation in serum-free medium. J Neurosci Methods. https://doi.org/10.1016/j.jneumeth.2018.06.002
Morris KM, Aden DP, Knowles BB, Colten HR (1982) Complement biosynthesis by the human hepatoma-derived cell line HepG2. J Clin Invest 70:906–913. https://doi.org/10.1172/JCI110687
Lubbers R, van Essen MF, van Kooten C, Trouw LA (2017) Production of complement components by cells of the immune system: production of complement components. Clin Exp Immunol 188:183–194. https://doi.org/10.1111/cei.12952
Peng Q, Li K, Sacks SH, Zhou W (2009) The role of anaphylatoxins C3a and C5a in regulating innate and adaptive immune responses. Inflamm Allergy Drug Targets 8:236–246. https://doi.org/10.2174/187152809788681038
Giraud T, Rufas P, Chmilewsky F et al (2017) Complement activation by pulp capping materials plays a significant role in both inflammatory and pulp stem cells’ recruitment. J Endod 43:1104–1110. https://doi.org/10.1016/j.joen.2017.02.016
Zimmermann CE, Gierloff M, Hedderich J, Açil Y, Wiltfang J, Terheyden H (2011) Biocompatibility of bone graft substitutes: effects on survival and proliferation of porcine multilineage stem cells in vitro. Folia Morphol (Warsz) 70:154–160
Adams BR, Mostafa A, Schwartz Z, Boyan BD (2014) Osteoblast response to nanocrystalline calcium hydroxyapatite depends on carbonate content: osteoblasts and Carbonated Hydroxyapatite. J Biomed Mater Res 102:3237–3242. https://doi.org/10.1002/jbm.a.34994
Figueiredo M, Henriques J, Martins G et al (2010) Physicochemical characterization of biomaterials commonly used in dentistry as bone substitutes-comparison with human bone: biomaterials in dentistry as bone substitutes. J Biomed Mater Res 92B:409–419. https://doi.org/10.1002/jbm.b.31529
Barone A, Nannmark U (2014) Bone, biomaterials & beyond. Edra Masson. p 200
Andersson J, Ekdahl KN, Larsson R et al (2002) C3 Adsorbed to a polymer surface can form an initiating alternative pathway convertase. J Immunol 168:5786–5791. https://doi.org/10.4049/jimmunol.168.11.5786
Nilsson B, Korsgren O, Lambris JD, Ekdahl KN (2010) Can cells and biomaterials in therapeutic medicine be shielded from innate immune recognition? Trends Immunol 31:32–38. https://doi.org/10.1016/j.it.2009.09.005
Ignatius A, Schoengraf P, Kreja L, Liedert A, Recknagel S, Kandert S, Brenner RE, Schneider M, Lambris JD, Huber-Lang M (2011) Complement C3a and C5a modulate osteoclast formation and inflammatory response of osteoblasts in synergism with IL-1β. J Cell Biochem 112:2594–2605. https://doi.org/10.1002/jcb.23186
Schraufstatter IU (2015) Complement activation in the context of stem cells and tissue repair. World J Stem Cells 7:1090. https://doi.org/10.4252/wjsc.v7.i8.1090
Hutmacher DW (2000) Scaffolds in tissue engineering bone and cartilage. Biomaterials 21:2529–2543. https://doi.org/10.1016/S0142-9612(00)00121-6
Acknowledgments
The authors thank Dr. Jean-Charles GARDON for providing the teeth.
Funding
The work was supported by Aix-Marseille University and CNRS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jeanneau, C., Le Fournis, C. & About, I. Xenogeneic bone filling materials modulate mesenchymal stem cell recruitment: role of the Complement C5a. Clin Oral Invest 24, 2321–2329 (2020). https://doi.org/10.1007/s00784-019-03087-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03087-5