Abstract
We analysed the familial aggregation (familiality) of cognitive dimensions and explored their role as liability markers for early-onset bipolar disorder (EOBD). The sample comprised 99 subjects from 26 families, each with an offspring diagnosed with EOBD. Four cognitive dimensions were assessed: reasoning skills; attention and working memory; memory; and executive functions. Their familiality was investigated in the total sample and in a subset of healthy relatives. The intra-family resemblance score (IRS), a family-based index of the similarity of cognitive performance among family members, was calculated. Familiality was detected for the attention and working memory (AW) dimension in the total sample (ICC = 0.37, p = 0.0004) and in the subsample of healthy relatives (ICC = 0.37, p = 0.016). The IRS reflected that there are families with similar AW mean scores (either high or low) and families with heterogeneous scores. Families with the most common background for the AW dimension (IRS > 0) were selected and dichotomized in two groups according to the mean family AW score. This allowed differentiating families whose members had similar high scores than those with similar low scores: both patients (t = − 4.82, p = 0.0005) and relatives (t = − 5.04, p < 0.0001) of the two groups differed in their AW scores. AW dimension showed familial aggregation, suggesting its putative role as a familial vulnerability marker for EOBD. The IRS estimation allowed the identification of families with homogeneous scores for this dimension. This represents a first step towards the investigation of the underlying mechanisms of AW dimension and the identification of etiological subgroups.

Similar content being viewed by others
References
Merikangas KR, Jin R, He J-P et al (2011) Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatr 68:241–251. https://doi.org/10.1001/archgenpsychiatry.2011.12
Goodwin FK, Jamison KR (1990) Manic-depressive illness. New York
Kurtz MM, Gerraty RT (2009) A meta-analytic investigation of neurocognitive deficits in bipolar illness: profile and effects of clinical state. Neuropsychology 23:551–562. https://doi.org/10.1037/a0016277
Szmulewicz AG, Samamé C, Martino DJ et al (2015) An updated review on the neuropsychological profile of subjects with bipolar disorder. Arch Clin Psychiatr (São Paulo) 42:139–146. https://doi.org/10.1590/0101-60830000000064
Bourne C, Aydemir Ö, Balanzá-Martínez V et al (2013) Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis. Acta Psychiatr Scand 128:149–162. https://doi.org/10.1111/acps.12133
Song J, Bergen SE, Kuja-Halkola R et al (2015) Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord 17:184–193. https://doi.org/10.1111/bdi.12242
Kieseppä T, Partonen T, Haukka J et al (2004) High concordance of bipolar I disorder in a nationwide sample of twins. Am J Psychiatr 161:1814–1821. https://doi.org/10.1176/ajp.161.10.1814
Nurnberger JI, Koller DL, Jung J et al (2014) Identification of pathways for bipolar disorder: a meta-analysis. JAMA psychiatr 71:657–664. https://doi.org/10.1001/jamapsychiatry.2014.176
Faraone SV, Glatt SJ, Tsuang MT (2003) The genetics of pediatric-onset bipolar disorder. Biol Psychiatr 53:970–977
Pavuluri MN, Birmaher B, Naylor MW (2005) Pediatric bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatr 44:846–871. https://doi.org/10.1097/01.chi.0000170554.23422.c1
Schürhoff F, Bellivier F, Jouvent R et al (2000) Early and late onset bipolar disorders: two different forms of manic-depressive illness? J Affect Disord 58:215–221
Grigoroiu-Serbanescu M, Rietschel M, Hauser J et al (2014) Commingling analysis of age-of-onset in bipolar I disorder and the morbid risk for major psychoses in first degree relatives of bipolar I probands. J Affect Disord 168:197–204. https://doi.org/10.1016/j.jad.2014.06.054
Tozzi F, Manchia M, Galwey NW et al (2011) Admixture analysis of age at onset in bipolar disorder. Psychiatr Res 185:27–32. https://doi.org/10.1016/j.psychres.2009.11.025
Ortiz A, Bradler K, Slaney C et al (2011) An admixture analysis of the age at index episodes in bipolar disorder. Psychiatr Res 188:34–39. https://doi.org/10.1016/j.psychres.2010.10.033
Post RM, Altshuler LL, Kupka R et al (2016) Age of onset of bipolar disorder: combined effect of childhood adversity and familial loading of psychiatric disorders. J Psychiatr Res 81:63–70. https://doi.org/10.1016/j.jpsychires.2016.06.008
Post RM, Altshuler LL, Kupka R et al (2016) Age at onset of bipolar disorder related to parental and grandparental illness burden. J Clin Psychiatr 77:e1309–e1315. https://doi.org/10.4088/JCP.15m09811
Preisig M, Strippoli MPF, Castelao E et al (2016) The specificity of the familial aggregation of early-onset bipolar disorder: A controlled 10-year follow-up study of offspring of parents with mood disorders. J Affect Disord 190:26–33. https://doi.org/10.1016/j.jad.2015.10.005
Preisig M, Strippoli M-PF, Castelao E et al (2016) The specificity of the familial aggregation of early-onset bipolar disorder : a controlled 10-year follow-up study of offspring of parents with mood disorders. J Affect Disord 190:26–33. https://doi.org/10.1016/j.jad.2015.10.005
Lázaro L, Castro-Fornieles J, de la Fuente JE et al (2007) Differences between prepubertal- versus adolescent- onset bipolar disorder in a Spanish clinical sample. Eur Child Adolesc Psychiatr 16:510–516. https://doi.org/10.1007/s00787-007-0629-9
Connor DF, Ford JD, Pearson GS, et al (2017) Early-onset bipolar disorder: characteristics and outcomes in the clinic. J Child Adolesc Psychopharmacol cap.2017.0058. 10.1089/cap.2017.0058
Joslyn C, Hawes DJ, Hunt C, Mitchell PB (2016) Is age of onset associated with severity, prognosis, and clinical features in bipolar disorder? A meta-analytic review. Bipolar Disord 18:389–403. https://doi.org/10.1111/bdi.12419
Baldessarini RJ, Tondo L, Vazquez GH et al (2012) Age at onset versus family history and clinical outcomes in 1,665 international bipolar-I disorder patients. World Psychiatr 11:40–46
Doyle AE, Wilens TE, Kwon A et al (2005) Neuropsychological functioning in youth with bipolar disorder. Biol Psychiatr 58:540–548. https://doi.org/10.1016/j.biopsych.2005.07.019
Joseph MF, Frazier TW, Youngstrom EA, Soares JC (2008) A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. J Child Adolesc Psychopharmacol 18:595–605. https://doi.org/10.1089/cap.2008.064
Lera-Miguel S, Andrés-Perpiñá S, Calvo R et al (2011) Early-onset bipolar disorder: how about visual-spatial skills and executive functions? Eur Arch Psychiatr Clin Neurosci 261:195–203. https://doi.org/10.1007/s00406-010-0169-z
Frías Á, Palma C, Farriols N (2014) Neurocognitive impairments among youth with pediatric bipolar disorder: a systematic review of neuropsychological research. J Affect Disord 166:297–306. https://doi.org/10.1016/j.jad.2014.05.025
Dickstein DP, Axelson D, Weissman AB et al (2016) Cognitive flexibility and performance in children and adolescents with threshold and sub-threshold bipolar disorder. Eur Child Adolesc Psychiatr 25:625–638. https://doi.org/10.1007/s00787-015-0769-2
McCarthy J, McGlashan A, Kraseski K et al (2004) Sustained attention and visual processing speed in children and adolescents with bipolar disorder and other psychiatric disorders. Psychol Rep 95:39–47. https://doi.org/10.2466/pr0.95.1.39-47
Elias LR, Miskowiak KW, Vale AMO et al (2017) Cognitive impairment in euthymic pediatric bipolar disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatr 56:286–296. https://doi.org/10.1016/j.jaac.2017.01.008
Iverson GL, Brooks BL, Langenecker SA, Young AH (2011) Identifying a cognitive impairment subgroup in adults with mood disorders. J Affect Disord 132:360–367. https://doi.org/10.1016/j.jad.2011.03.001
Martino DJ, Strejilevich SA, Scápola M et al (2008) Heterogeneity in cognitive functioning among patients with bipolar disorder. J Affect Disord 109:149–156. https://doi.org/10.1016/j.jad.2007.12.232
Martino DJ, Strejilevich SA, Marengo E et al (2014) Toward the identification of neurocognitive subtypes in euthymic patients with bipolar disorder. J Affect Disord 167:118–124. https://doi.org/10.1016/j.jad.2014.05.059
Burdick KE, Russo M, Frangou S et al (2014) Empirical evidence for discrete neurocognitive subgroups in bipolar disorder: clinical implications. Psychol Med 44:3083–3096. https://doi.org/10.1017/S0033291714000439
Lewandowski KE, Sperry SH, Cohen BM, Öngür D (2014) Cognitive variability in psychotic disorders: a cross-diagnostic cluster analysis. Psychol Med 44:3239–3248. https://doi.org/10.1017/S0033291714000774
Bora E, Hıdıroğlu C, Özerdem A et al (2016) Executive dysfunction and cognitive subgroups in a large sample of euthymic patients with bipolar disorder. Eur Neuropsychopharmacol 26:1338–1347. https://doi.org/10.1016/j.euroneuro.2016.04.002
Aminoff SR, Hellvin T, Lagerberg TV et al (2013) Neurocognitive features in subgroups of bipolar disorder. Bipolar Disord 15:272–283. https://doi.org/10.1111/bdi.12061
Volkert J, Kopf J, Kazmaier J et al (2015) Evidence for cognitive subgroups in bipolar disorder and the influence of subclinical depression and sleep disturbances. Eur Neuropsychopharmacol 25:192–202. https://doi.org/10.1016/j.euroneuro.2014.07.017
Bora E, Yucel M, Pantelis C (2009) Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord 113:1–20. https://doi.org/10.1016/j.jad.2008.06.009
Hıdıroğlu C, Torres IJ, Er A et al (2015) Response inhibition and interference control in patients with bipolar I disorder and first-degree relatives. Bipolar Disord 17:781–794. https://doi.org/10.1111/bdi.12335
Papmeyer M, Sussmann JE, Hall J et al (2015) Neurocognition in individuals at high familial risk of mood disorders with or without subsequent onset of depression. Psychol Med 45:3317–3327. https://doi.org/10.1017/S0033291715001324
Jabben N, Arts B, van Os J, Krabbendam L (2010) Neurocognitive functioning as intermediary phenotype and predictor of psychosocial functioning across the psychosis continuum: studies in schizophrenia and bipolar disorder. J Clin Psychiatr 71:764–774. https://doi.org/10.4088/JCP.08m04837yel
Lin K, Lu R, Chen K et al (2017) Differences in cognitive deficits in individuals with subthreshold syndromes with and without family history of bipolar disorder. J Psychiatr Res 91:177–183. https://doi.org/10.1016/j.jpsychires.2017.05.005
Arts B, Jabben N, Krabbendam L, van Os J (2008) Meta-analyses of cognitive functioning in euthymic bipolar patients and their first-degree relatives. Psychol Med 38:771–785. https://doi.org/10.1017/S0033291707001675
Calafiore D, Rossell SL, Van Rheenen TE (2018) Cognitive abilities in first-degree relatives of individuals with bipolar disorder. J Affect Disord 225:147–152. https://doi.org/10.1016/j.jad.2017.08.029
McCormack C, Green MJ, Rowland JE et al (2016) Neuropsychological and social cognitive function in young people at genetic risk of bipolar disorder. Psychol Med 46:745–758. https://doi.org/10.1017/S0033291715002147
Miskowiak KW, Kjærstad HL, Meluken I et al (2017) The search for neuroimaging and cognitive endophenotypes: a critical systematic review of studies involving unaffected first-degree relatives of individuals with bipolar disorder. Neurosci Biobehav Rev 73:1–22
Bora E, Özerdem A (2017) A meta-analysis of neurocognition in youth with familial high risk for bipolar disorder. Eur Psychiatr 44:17–23
Bora E (2017) A comparative meta-analysis of neurocognition in first-degree relatives of patients with schizophrenia and bipolar disorder. Eur Psychiatr 45:121–128. https://doi.org/10.1016/j.eurpsy.2017.06.003
Olvet DM, Stearns WH, McLaughlin D et al (2010) Comparing clinical and neurocognitive features of the schizophrenia prodrome to the bipolar prodrome. Schizophr Res 123:59–63. https://doi.org/10.1016/j.schres.2010.07.005
Ratheesh A, Lin A, Nelson B et al (2013) Neurocognitive functioning in the prodrome of mania—an exploratory study. J Affect Disord 147:441–445. https://doi.org/10.1016/j.jad.2012.09.017
Soler J, Ferentinos P, Prats C et al (2017) Familial aggregation of schizotypy in schizophrenia-spectrum disorders and its relation to clinical and neurodevelopmental characteristics. J Psychiatr Res 84:214–220. https://doi.org/10.1016/j.jpsychires.2016.09.026
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatr 36:980–988. https://doi.org/10.1097/00004583-199707000-00021
McClellan J, Kowatch R, Findling RL (2007) Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatr 46:107–125. https://doi.org/10.1097/01.chi.0000242240.69678.c4
Soler J, Ferentinos P, Prats C et al (2016) Familial aggregation of schizotypy in schizophrenia-spectrum disorders and its relation to clinical and neurodevelopmental characteristics. J Psychiatr Res 84:214–220. https://doi.org/10.1016/j.jpsychires.2016.09.026
Suarez BK, Van Eerdewegh P (1984) A comparison of three affected-sib-pair scoring methods to detect HLA-linked disease susceptibility genes. Am J Med Genet 18:135–146. https://doi.org/10.1002/ajmg.1320180117
Knowles EEM, Mathias SR, McKay DR et al (2014) Genome-wide analyses of working-memory ability: a review. Curr Behav Neurosci reports 1:224–233. https://doi.org/10.1007/s40473-014-0028-8
Cornblatt BA, Risch NJ, Faris G et al (1988) The continuous performance test, identical pairs version (CPT-IP): I. new findings about sustained attention in normal families. Psychiatr Res 26:223–238
Myles-Worsley M, Coon H (1997) Genetic and developmental factors in spontaneous selective attention: a study of normal twins. Psychiatr Res 71:163–174
Blokland GAM, Mesholam-Gately RI, Toulopoulou T et al (2017) Heritability of neuropsychological measures in schizophrenia and nonpsychiatric populations: a systematic review and meta-analysis. Schizophr Bull 43:788–800. https://doi.org/10.1093/schbul/sbw146
Xu C, Sun J, Duan H et al (2015) Gene, environment and cognitive function: a Chinese twin ageing study. Age Ageing 44:452–457. https://doi.org/10.1093/ageing/afv015
Kim D, Kim J, Koo T et al (2015) Shared and distinct neurocognitive endophenotypes of schizophrenia and psychotic bipolar disorder. Clin Psychopharmacol Neurosci 13:94–102. https://doi.org/10.9758/cpn.2015.13.1.94
Tirapu-Ustarroz J, Cordero-Andres P, Luna-Lario P, Hernaez-Goni P (2017) Proposed model of executive functions based on factorial analyses. Rev Neurol 64:75–84
Robertson IH, Ward T, Ridgeway V, Nimmo-Smith I (1996) The structure of normal human attention: the test of everyday attention. J Int Neuropsychol Soc 2:525–534
Boone KB, Pontón MO, Gorsuch RL et al (1998) Factor analysis of four measures of prefrontal lobe functioning. Arch Clin Neuropsychol 13:585–595
Ríos M, Periáñez JA, Muñoz-Céspedes JM (2004) Attentional control and slowness of information processing after severe traumatic brain injury. Brain Inj 18:257–272. https://doi.org/10.1080/02699050310001617442
Vlad M, Raucher-Chéné D, Henry A, Kaladjian A (2018) Functional outcome and social cognition in bipolar disorder: Is there a connection? Eur Psychiatr 52:116–125. https://doi.org/10.1016/J.EURPSY.2018.05.002
Miskowiak KW, Seeberg I, Kjaerstad HL, et al (2019) Affective cognition in bipolar disorder: a systematic review by the ISBD targeting cognition task force. Bipolar Disord bdi.12834. 10.1111/bdi.12834
Bora E, Bartholomeusz C, Pantelis C (2016) Meta-analysis of theory of mind (ToM) impairment in bipolar disorder. Psychol Med 46:253–264. https://doi.org/10.1017/S0033291715001993
Ospina LH, Nitzburg GC, Shanahan M et al (2018) Social cognition moderates the relationship between neurocognition and community functioning in bipolar disorder. J Affect Disord 235:7–14. https://doi.org/10.1016/j.jad.2018.03.013
Miskowiak K, Burdick K, Martinez-Aran A et al (2018) Assessing and addressing cognitive impairment in bipolar disorder: the International Society for Bipolar Disorders Targeting Cognition Task Force recommendations for clinicians. Bipolar Disord 20:184–194. https://doi.org/10.1111/bdi.12595
Sepede G, De Berardis D, Campanella D et al (2012) Impaired sustained attention in euthymic bipolar disorder patients and non-affected relatives: an fMRI study. Bipolar Disord 14:764–779. https://doi.org/10.1111/bdi.12007
Klimes-Dougan B, Ronsaville D, Wiggs EA, Martinez PE (2006) Neuropsychological functioning in adolescent children of mothers with a history of bipolar or major depressive disorders. Biol Psychiatr 60:957–965. https://doi.org/10.1016/j.biopsych.2006.03.031
Volkert J, Haubner J, Kazmaier J et al (2016) Cognitive deficits in first-degree relatives of bipolar patients: the use of homogeneous subgroups in the search of cognitive endophenotypes. J Neural Transm 123:1001–1011. https://doi.org/10.1007/s00702-016-1581-y
Lera-Miguel S, Andrés-Perpiñá S, Fatjó-Vilas M et al (2015) Two-year follow-up of treated adolescents with early-onset bipolar disorder: Changes in neurocognition. J Affect Disord 172:48–54. https://doi.org/10.1016/j.jad.2014.09.041
Ferentinos P, Koukounari A, Power R et al (2015) Familiality and SNP heritability of age at onset and episodicity in major depressive disorder. Psychol Med 45:2215–2225. https://doi.org/10.1017/S0033291715000215
Peralta V, Fañanás L, Martín-Reyes M, Cuesta MJ (2017) Dissecting the catatonia phenotype in psychotic and mood disorders on the basis of familial-genetic factors. Schizophr Res. https://doi.org/10.1016/j.schres.2017.09.013
Mucci A, Galderisi S, Green MF et al (2018) Familial aggregation of MATRICS consensus cognitive battery scores in a large sample of outpatients with schizophrenia and their unaffected relatives. Psychol Med 48:1359–1366. https://doi.org/10.1017/S0033291717002902
Stahl E, Breen G, Forstner A, et al (2018) Genomewide association study identifies 30 loci associated with bipolar disorder. bioRxiv 173062. 10.1101/173062
Hou L, Bergen SE, Akula N et al (2016) Genome-wide association study of 40,000 individuals identifies two novel loci associated with bipolar disorder. Hum Mol Genet 25:3383–3394. https://doi.org/10.1093/hmg/ddw181
Chen DT, Jiang X, Akula N et al (2013) Genome-wide association study meta-analysis of European and Asian-ancestry samples identifies three novel loci associated with bipolar disorder. Mol Psychiatr 18:195–205. https://doi.org/10.1038/mp.2011.157
Charney AW, Ruderfer DM, Stahl EA et al (2017) Evidence for genetic heterogeneity between clinical subtypes of bipolar disorder. Transl Psychiatr 7:e993–e993. https://doi.org/10.1038/tp.2016.242
Psychiatric GWAS Consortium Bipolar Disorder Working Group (2011) Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nat Genet 43:977–983. https://doi.org/10.1038/ng.943
Croarkin PE, Luby JL, Cercy K, et al (2017) Genetic risk score analysis in early-onset bipolar disorder. J Clin Psychiatr. 10.4088/JCP.15m10314
Kennedy KP, Cullen KR, DeYoung CG, Klimes-Dougan B (2015) The genetics of early-onset bipolar disorder: A systematic review. J Affect Disord 184:1–12. https://doi.org/10.1016/j.jad.2015.05.017
Davies G, Marioni RE, Liewald DC et al (2016) Genome-wide association study of cognitive functions and educational attainment in UK Biobank (N = 112 151). Mol Psychiatr 21:758–767. https://doi.org/10.1038/mp.2016.45
Ibrahim-Verbaas CA, Bressler J, Debette S et al (2016) GWAS for executive function and processing speed suggests involvement of the CADM2 gene. Mol Psychiatr 21:189–197. https://doi.org/10.1038/mp.2015.37
Trampush JW, Yang MLZ, Yu J et al (2017) GWAS meta-analysis reveals novel loci and genetic correlates for general cognitive function: a report from the COGENT consortium. Mol Psychiatr 22:336–345. https://doi.org/10.1038/mp.2016.244
Davies G, Lam M, Harris SE et al (2018) Study of 300,486 individuals identifies 148 independent genetic loci influencing general cognitive function. Nat Commun 9:2098. https://doi.org/10.1038/s41467-018-04362-x
Liebers DT, Pirooznia M, Seiffudin F et al (2016) Polygenic risk of schizophrenia and cognition in a population-based survey of older adults. Schizophr Bull 42:984–991. https://doi.org/10.1093/schbul/sbw001
Ranlund S, Calafato S, Thygesen JH et al (2018) A polygenic risk score analysis of psychosis endophenotypes across brain functional, structural, and cognitive domains. Am J Med Genet B Neuropsychiatr Genet 177:21–34. https://doi.org/10.1002/ajmg.b.32581
Smeland OB, Bahrami S, Frei O et al (2019) Genome-wide analysis reveals extensive genetic overlap between schizophrenia, bipolar disorder, and intelligence. Mol Psychiatr. https://doi.org/10.1038/s41380-018-0332-x
Hagenaars SP, Harris SE, Davies G et al (2016) Shared genetic aetiology between cognitive functions and physical and mental health in UK Biobank (N = 112 151) and 24 GWAS consortia. Mol Psychiatr 21:1624–1632. https://doi.org/10.1038/mp.2015.225
Savage JE, Jansen PR, Stringer S et al (2018) Genome-wide association meta-analysis in 269,867 individuals identifies new genetic and functional links to intelligence. Nat Genet 50:912–919. https://doi.org/10.1038/s41588-018-0152-6
Georgiades A, Rijsdijk F, Kane F et al (2016) New insights into the endophenotypic status of cognition in bipolar disorder: Genetic modelling study of twins and siblings. Br J Psychiatr 208:539–547. https://doi.org/10.1192/bjp.bp.115.167239
Fernandes CPD, Christoforou A, Giddaluru S et al (2013) A genetic deconstruction of neurocognitive traits in schizophrenia and bipolar disorder. PLoS ONE 8:e81052. https://doi.org/10.1371/journal.pone.0081052
Hill WD, Davies G, Liewald DC et al (2016) Age-dependent pleiotropy between general cognitive function and major psychiatric disorders. Biol Psychiatr 80:266–273. https://doi.org/10.1016/j.biopsych.2015.08.033
Bo Q, Mao Z, Li X et al (2017) Use of the MATRICS consensus cognitive battery (MCCB) to evaluate cognitive deficits in bipolar disorder: a systematic review and meta-analysis. PLoS ONE 12:e0176212. https://doi.org/10.1371/journal.pone.0176212
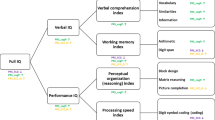
Wechsler D (2004) The Wechsler intelligence scale for children, 4th edn. Pearson Assessment, London
Wechsler D (1997) Wechsler Adult Intelligence Scale, 3rd edition (WAIS-III) Administration and scoring manual., Adaptación Española TEA ediciones, Madrid. Psychological Corporation, San Antonio.
Benton AL (1969) Development of a multilingual aphasia battery. Progress and problems J Neurol Sci 9:39–48. https://doi.org/10.1016/0022-510X(69)90057-4
Heaton RK (1981) Wisconsin card sorting test: computer version 2. Research Edition. (Psychological Assessment Resources, Inc., Odessa, F.L., 1981).
Cornblatt BA, Lenzenweger MF, Erlenmeyer-Kimling L (1989) The continuous performance test, identical pairs version: II. Contrasting attentional profiles in schizophrenic and depressed patients. Psychiatr Res 29:65–85
Wechsler D (1997) Wechsler memory scale-Third Edition San Antonio. The Psychological Corporation, TX
Delis, DC, Kramer JH, Kaplan, E, Ober BA (1987) CVLT, California Verbal Learning Test: Adult Version: Manual. Psychological Corporation
Acknowledgements
This study was funded by: (i) Fundación Alicia Koplowitz, (ii) the Instituto de Salud Carlos III through project PI15/01420 (co-funded by the European Regional Development Fund/European Social Fund “Investing in your future”), (iii) the Comissionat per a Universitats i Recerca del DIUE, of the Generalitat de Catalunya regional authorities (2017SGR1577, 2017SGR1271 and 2017SGR881), (iv) an Ajuts de Personal Investigador Predoctoral en Formació grant (APIF-Universitat de Barcelona) awarded to J. Soler, and (vi) a Sara Borrell postdoctoral contract awarded to M. Fatjó-Vilas (CD16/00264).
Funding
The funding sources played no role in the design of the study, the collection, analysis and interpretation of data, or the decision to submit this manuscript for publication. We are also deeply grateful to all participants, whose generosity made this work possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval was obtained from the local research ethics committees. All participants provided written consent after being informed of the study procedures and implications. All procedures were carried out in accordance with the Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Soler, J., Lera-Miguel, S., Lázaro, L. et al. Familial aggregation analysis of cognitive performance in early-onset bipolar disorder. Eur Child Adolesc Psychiatry 29, 1705–1716 (2020). https://doi.org/10.1007/s00787-020-01486-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01486-8