Abstract
Purpose
Hybrid aortic arch repair in patients with chronic residual aortic dissection (RAD) is a less invasive alternative to conventional surgical treatment. The aim of this study was to describe the short-term and long-term results of hybrid treatment for RAD after type A repair.
Methods
In this retrospective single-center cohort study, all patients treated for chronic RAD with hybrid aortic arch repair were included. Indications for treatment were rapid aortic growth, aortic diameter > 55 mm, or aortic rupture.
Results
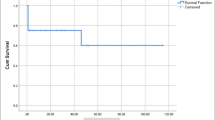
Between 2009 and 2020, we performed 29 hybrid treatments for chronic RAD. Twenty-four patients were treated for complete supra-aortic debranching in zones 0 and 5 with left subclavian artery debranching alone in zone 2. There was 1 perioperative death (3.4%): The patient was treated for an aortic rupture. There was no spinal cord ischemia and 1 minor stroke (3.4%). After a median follow-up of 25.4 months (range 3-97 months), the long-term mortality was 10.3% (3/29) with no late aortic-related deaths. Twenty-seven patients (93.1%) developed FL thrombosis of the descending thoracic aorta; the rate of aneurysmal progression on thoraco-abdominal aorta was 41.4% (12/29), and the rate of aortic reintervention was 34.5% (10/29).
Conclusion
In a high-volume aortic center, hybrid repair of RAD is associated with good anatomical results and a low risk of perioperative morbidity and mortality, including that of patients treated in zone 0. A redo replacement of the ascending aortic segment is sometimes necessary to provide a safer proximal landing zone and reduce the risk of type 1 endoleak after TEVAR.




Similar content being viewed by others
Availability of Data and Material
All the patients included in this study were clearly informed about the use of their data for clinical research, and the institutional review board approved the project (approval number 2019-48).
Code Availability
Not applicable.
Abbreviations
- RAD:
-
Residual aortic dissection after type A repair
- HR:
-
Hybrid repair
- TEVAR:
-
Thoracic endovascular aortic repair
- SA:
-
Supra-aortic
- IA:
-
Innominate artery
- LCCA:
-
Left common carotid artery
- LSA:
-
Left subclavian artery
- CPB:
-
Cardiopulmonary bypass
- CA:
-
Circulatory arrest
- ACP:
-
Antegrade cerebral protection
- CT:
-
Computed tomography
- CSFD:
-
Cerebrospinal fluid drainage
- STABILISE:
-
Stent-assisted balloon-induced intimal disruption and relamination in aortic dissection repair
- FL:
-
False lumen
- NIRS:
-
Near-infrared spectroscopy
- SCI:
-
Spinal cord ischemia
- CI:
-
Confidence interval
- FET:
-
Frozen elephant trunk
References
Concistre G, Casali G, Santaniello E, et al. Reoperation after surgical correction of acute type A aortic dissection: risk factor analysis. Ann Thorac Surg. 2012;93:450–5.
Zierer A, Voeller RK, Hill KE, Kouchoukos NT, Damiano RJ Jr, Moon MR. Aortic enlargement and late reoperation after repair of acute type A aortic dissection. Ann Thorac Surg. 2007;84:479–86. discussion 486-7.
Tamura K, Chikazawa G, Hiraoka A, Totsugawa T, Sakaguchi T, Yoshitaka H. The prognostic impact of distal anastomotic new entry after acute type I aortic dissection repair. Eur J Cardiothorac Surg. 2017;52:867–73.
Fattouch K, Sampognaro R, Navarra E, Caruso M, Pisano C, Coppola G, et al. Long-term results after repair of type A acute aortic dissection according to false lumen patency. Ann Thorac Surg. 2009;88:1244–50.
Kimura N, Itoh S, Yuri K, Adachi K, Matsumoto H, Yamaguchi A, et al. Reoperation for enlargement of the distal aorta after initial surgery for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2015;149:S91–8. e1.
Nakamura K, Onitsuka T, Yano M, Yano Y, Matsuyama M, Furukawa K. Risk factor analysis for ascending aorta and aortic arch repair using selective cerebral perfusion with open technique: role of open-stent graft placement. J Cardiovasc Surg. 2006;47:659–65.
Kazui T, Yamashita K, Washiyama N, et al. Aortic arch replacement using selective cerebral perfusion. Ann Thorac Surg. 2007;83:S796–8. discussion S824-31.
Haulon S, Greenberg RK, Spear R, Eagleton M, Abraham C, Lioupis C, et al. Global experience with an inner branched arch endograft. J Thorac Cardiovasc Surg. 2014;148:1709–16.
Koullias GJ, Wheatley GH 3rd. State-of-the-art of hybrid procedures for the aortic arch: a meta-analysis. Ann Thorac Surg. 2010;90:689–97.
Cao P, De Rango P, Czerny M, et al. Systematic review of clinical outcomes in hybrid procedures for aortic arch dissections and other arch diseases. J Thorac Cardiovasc Surg. 2012;144:1286–300. 1300 e1-2.
Faure EM, El Batti S, Sutter W, et al. Stent-assisted balloon-induced intimal disruption and relamination of distal remaining aortic dissection after acute DeBakey type I repair. J Thorac Cardiovasc Surg. 2019;157:2159–65.
Faure EM, El Batti S, Sutter W, et al. Stent-assisted balloon dilatation of chronic aortic dissection. J Thorac Cardiovasc Surg. 2020;S0022–5223(20)30430–X. Online ahead of print.
Czerny M, Kreibich M, Morlock J, Kondov S, Scheumann J, Schröfel H, et al. Chronic type B “residual” after type A: what I would do? J Vis Surg. 2018;4:14.
Dell’Aquila AM, Pollari F, Fattouch K, Santarpino G, Hillebrand J, Schneider S, et al. Early outcomes in re-do operation after acute type A aortic dissection: results from the multicenter REAAD database. Heart Vessel. 2017;32:566–73.
Malvindi PG, van Putte BP, Sonker U, Heijmen RH, Schepens MA, Morshuis WJ. Reoperation after acute type A aortic dissection repair: a series of 104 patients. Ann Thorac Surg. 2013;95:922–7.
Quintana E, Bajona P, Schaff HV, Dearani JA, Daly RC, Greason KL, et al. Open aortic arch reconstruction after previous cardiac surgery: outcomes of 168 consecutive operations. J Thorac Cardiovasc Surg. 2014;148:2944–50.
Di Bartolomeo R, Berretta P, Pantaleo A, et al. Long-term outcomes of open arch repair after a prior aortic operation: our experience in 154 patients. Ann Thorac Surg. 2017;103:1406–12.
Verscheure D, Haulon S, Tsilimparis N, Resch T, Wanhainen A, Mani K, et al. Endovascular treatment of post type A chronic aortic arch dissection with a branched endograft: early results from a retrospective international multicenter study. Ann Surg. 2019; Online ahead of print.
Papakonstantinou NA, Antonopoulos CN, Baikoussis NG, Kakisis I, Geroulakos G. Aortic arch reconstruction: are hybrid debranching procedures a good choice? Heart Lung Circ. 2018;27:1335–49.
Shirakawa Y, Kuratani T, Shimamura K, Torikai K, Sakamoto T, Shijo T, et al. The efficacy and short-term results of hybrid thoracic endovascular repair into the ascending aorta for aortic arch pathologies. Eur J Cardiothorac Surg. 2014;45:298–304. discussion 304.
Antoniou GA, El Sakka K, Hamady M, Wolfe JH. Hybrid treatment of complex aortic arch disease with supra-aortic debranching and endovascular stent graft repair. Eur J Vasc Endovasc Surg. 2010;39:683–90.
Canaud L, Gandet T, Ozdemir BA, Albat B, Marty-Ane C, Alric P. Hybrid aortic repair of dissecting aortic arch aneurysm after surgical treatment of acute type A dissection. Ann Vasc Surg. 2016;30:175–80.
Antoniou GA, Mireskandari M, Bicknell CD, Cheshire NJW, Gibbs RG, Hamady M, et al. Hybrid repair of the aortic arch in patients with extensive aortic disease. Eur J Vasc Endovasc Surg. 2010;40:715–21.
Vallejo N, Rodriguez-Lopez JA, Heidari P, Wheatley G, Caparrelli D, Ramaiah V, et al. Hybrid repair of thoracic aortic lesions for zone 0 and 1 in high-risk patients. J Vasc Surg. 2012;55:318–25.
Conzelmann LO, Hoffmann I, Blettner M, Kallenbach K, Karck M, Dapunt O, et al. Analysis of risk factors for neurological dysfunction in patients with acute aortic dissection type A: data from the German Registry for Acute Aortic Dissection type A (GERAADA). Eur J Cardiothorac Surg. 2012;42:557–65.
Faure EM, El Batti S, Abou Rjeili M, Julia P, Alsac JM. Mid-term outcomes of stent assisted balloon induced intimal disruption and relamination in aortic dissection repair (STABILISE) in acute type B aortic dissection. Eur J Vasc Endovasc Surg. 2018;56:209–15.
Sayer D, Bratby M, Brooks M, Loftus I, Morgan R, Thompson M. Aortic morphology following endovascular repair of acute and chronic type B aortic dissection: implications for management. Eur J Vasc Endovasc Surg. 2008;36(5):522–9.
Canaud L, Gandet T, Sfeir J, Ozdemir BA, Solovei L, Alric P. Risk factors for distal stent graft-induced new entry tear after endovascular repair of thoracic aortic dissection. J Vasc Surg. 2019;69(5):1610–4.
Acknowledgements
We would like to thank Professor Michel S. Makaroun (Pittsburgh, PA) for his careful reading and comments.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Alizée Porto, Arnaud Blanchard, Jean Victor Chazot, Laurence Bal, Mariangela De Masi, Pierre-Antoine Barral, Alexis Jacquier, Vlad Gariboldi, Frederic Collart, Valerie Deplano, and Marine Gaudry. The first draft of the manuscript was written by Marine Gaudry, Philippe Piquet, and Alizee Porto. Axel Bartoli made all figure revisions needed to improve the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting presentation: European Society of Vascular Surgery (ESVS), Hamburg, September 2019
Supplementary Information
ESM 1
(XLSX 112 kb)
Rights and permissions
About this article
Cite this article
Gaudry, M., Porto, A., Blanchard, A. et al. A 10-Year Aortic Center Experience with Hybrid Repair of Chronic “Residual” Aortic Dissection After Type A Repair. Cardiovasc Drugs Ther 36, 285–294 (2022). https://doi.org/10.1007/s10557-021-07150-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07150-w