Abstract
Background
Gastroparesis is a heterogeneous disorder. Patient characteristics and treatment responsiveness may differ based on the extent of delay in gastric emptying.
Aims
Characterize gastroparesis patients based on the degree of delay in gastric emptying, and assess the relationship of patient demographics, symptoms and response to therapy based on the extent of delay.
Methods
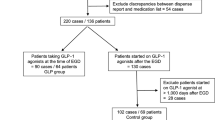
1333 solid-phase 4-h scintigraphic gastric emptying scans were reviewed. Delayed emptying was categorized on percent retention at 4 h: mild (10–19%), moderate (20–29%), and severe (≥ 30%). Analyses were performed with regard to demographics, symptoms, esophagogastroduodenoscopy findings, medication use, and emergency department (ED) visits/hospitalizations.
Results
284 patients had delayed gastric emptying: mild (42.6%), moderate (19.3%), and severe (37.3%). 79.5% were women, the mean age was 45 years (± 15), and mean symptom duration was 4.6 years (± 6.5). The main categories of gastroparesis were idiopathic and diabetes mellitus. The most commonly prescribed medications were metoclopramide, domperidone and erythromycin. Opiate use (n = 69) was associated with an increased degree of delayed gastric emptying (p = 0.03) with 50% of opiate users having very delayed gastric emptying. One-way analysis revealed that severely delayed gastric emptying correlated with both increased hospitalizations and ED visits.
Conclusions
Severe delay in gastric emptying is a risk factor for increased hospitalizations and ED visits. Opiate use correlates with increased severity of gastric emptying. Identifying at-risk patients, stopping opioids, and instituting a programmatic care plan for patients with severely delayed gastric emptying may reduce ED visits, hospitalizations, and healthcare costs.


Similar content being viewed by others
References
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. Clinical guideline: management of gastroparesis. Am JGastro. 2013;108:18–37.
Parkman HP, Hasler WL, Fisher RS, et al. for the American Gastroenterological Association. American Gastroenterological Association medical position statement: diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127:1589–1591.
Soykan I, Sivri B, Sarosiek I, et al. Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci. 1998;43:2398–2404. https://doi.org/10.1023/A:1026665728213.
Hoogerwerf WA, Pasricha PJ, Kalloo AN, et al. Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol. 1999;94:1029–1033.
Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462.
Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying Scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24–29. https://doi.org/10.1023/A:1005697422454.
Ziessman HA, Bonta DV, Goetze S, Ravich WJ. Experience with a simplified, standardized 4-hour gastric emptying protocol. J Nucl Med. 2007;48:568–572.
Keshavarzian A, Iber FL, Vaeth J. Gastric emptying in patients with insulin-requiring diabetic mellitus. Am J Gastroenterol. 1987;82:29–35.
Horowitz M, Maddox AF, Wishart JM, et al. Relationships between oesophageal transit and solid and liquid gastric empting in diabetes mellitus. Eur J Nucl Med. 1991;18:229–234.
Jones KL, Russo A, Stevens JE, et al. Predictors of delayed gastric emptying in diabetes. Diabetes Care. 2001;24:1264–1269.
Pande H, Lacy BE, Crowell MD. Inflammatory causes of gastroparesis: report of 5 cases. Dig Dis Sci. 2002;47:2664–2668. https://doi.org/10.1023/a:1021036601462.
Horowitz M, Harding PE, Maddox AF, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin dependent) diabetes mellitus. Diabetologia. 1989;32:151–159.
Jung HK, Choung RS, Locke GR, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136:1225–1233.
Lacy BE, Crowell MD, Mathis C, Bauer D, Heinberg LJ. Gastroparesis: quality of life and health care utilization. J Clin Gastroenterol. 2018;52:20–24.
Navas CM, Patel NK, Lacy BE. Gastroparesis: medical and therapeutic advances. Dig Dis Sci. 2017;62:2231–2240. https://doi.org/10.1007/s10620-017-4679-7.
Navas CM, Crowell MD, Lacy BE. The willingness of patients with gastroparesis to take risks with medications. Aliment Pharmacol Therap. 2019;49:429–436.
Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008;36:44–54.
Jaffe JK, Paladugu S, Gaughan JP, Parkman HP. Characteristics of nausea and its effects on quality of life in diabetic and idiopathic gastroparesis. J Clin Gastroenterol. 2011;45:317–321.
Almario CV, Ballal ML, Chey WD, Nordstrom C, Khanna D, Spiegel BM. Burden of gastrointestinal symptoms in the United States: results of a nationally representative survey of over 71,000 Americans. Am J Gastroenterol. 2018;113:1701.
Desai A, O’Connor M, Neja B, et al. Reproducibility of gastric emptying assessed with scintigraphy in patients with upper GI symptoms. Neurogastroenterol Motil. 2018;30:e13365.
Karamanolis G, Caenepeel P, Arts J, Tack J. Determinants of symptom pattern in idiopathic severely delayed gastric emptying: gastric emptying rate or proximal stomach dysfunction? Gut. 2007;56:29–36.
Horowitz M, Harding PE, Maddox A, et al. Gastric and oesophageal emptying in insulin-dependent diabetes mellitus. J Gastroenterol Hepatol. 1986;1:97–113.
Dibaise J, Patel N, Noelting J, et al. The relationship among gastroparetic symptoms, quality of life, and gastric emptying in patients referred for gastric emptying testing. Neurogastroenterol Motil. 2016;28:234–242.
Janssen P, Harris MS, Jones M, et al. The relation between symptom improvement and gastric emptying in the treatment of diabetic and idiopathic gastroparesis. Am J Gastroenterol. 2013;108:1382–1391.
Vijayvargiya P, Jameie-Oskooei S, Camilleri M, Chedid V, Erwin PJ, Murad MH. Association between delayed gastric emptying and upper gastrointestinal symptoms: a systematic review and meta-analysis. Gut. 2019;68:804–813.
Parkman HP, Yates KP, Maurer A, et al. Gastric emptying and symptoms of gastroparesis: specific symptoms correlating to severity of gastric retention. Gastroenterology. 2017;152:S933.
Parkman HP, Yates K, Hasler WL, et al. Clinical features of idiopathic gastroparesis vary with sex, body mass, symptom onset, delay in gastric emptying, and gastroparesis severity. Gastroenterology. 2011;140:101–115.
Hasler WL, Parkman HP, Wilson LA, et al. Psychological dysfunction is associated with symptom severity but not disease etiology or degree of gastric retention in patients with gastroparesis. Am J Gastroenterol. 2010;105:2357–2367.
Wadhwa V, Mehta D, Jobanputra Y, Lopez R, Thota PN, Sanaka MR. Healthcare utilization and costs associated with gastroparesis. World J Gastroenterol. 2017;23:4428–4436.
Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995–2004. Am J Gastroenterol. 2008;103:313–322.
Hyett B, Martinez FJ, Gill BM, et al. Delayed radionucleotide gastric emptying studies predict morbidity in diabetics with symptoms of gastroparesis. Gastroenterology. 2009;137:445–452.
Hirsch W, Nee J, Ballou S, et al. Emergency department burden of gastroparesis in the United States, 2006 to 2013. J Clin Gastroenterol. 2019;53:109–113.
Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–684.
Chenoweth D, Martin N, Pankowski J, Raymond LW. Nurse practitioner services: three-year impact on health care costs. J Occup Environ Med. 2008;50:1293–1298.
Jackson GL, Lee SY, Edelman D, Weinberger M, Yano EM. Employment of mid-level providers in primary care and control of diabetes. Prim Care Diabetes. 2011;5:25–31.
Qayed E, Muftah M. Frequency of hospital readmission and care fragmentation in gastroparesis: a nationwide analysis. World J Gastrointest Endosc. 2018;10:200–209.
Yu D, Ramsey FV, Norton WF, et al. The burdens, concerns, and quality of life of patients with gastroparesis. Dig Dis Sci. 2017;62:879–893. https://doi.org/10.1007/s10620-017-4456-7.
Highlights of prescribing information—Reglan. www.fda.gov. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/017854s062lbl.pdf. Accessed 27.4.19.
Alibibi R, McCallum RW. Metoclopramide: pharmacology and clinical application. Ann Intern Med. 1983;98:86–95.
Lacy BE, Weiser K. Gastric motility, gastroparesis, and gastric stimulation. Surg Clin. 2005;85:967–987.
Jeong ID, Camilleri M, Shin A, et al. A randomised, placebo-controlled trial comparing the effects of tapentadol and oxycodone on gastrointestinal and colonic transit in healthy humans. Aliment Pharmacol Ther. 2012;35:1088–1096.
Mittal RK, Frank EB, Lange RC, McCallum RW. Effects of morphine and naloxone on esophageal motility and gastric emptying in man. Dig Dis Sci. 1986;31:936–942. https://doi.org/10.1007/BF01303214.
Jehangir A, Parkman HP. Chronic opioids in gastroparesis: relationship withgastrointestinal symptoms, healthcare utilization and employment. World J Gastroenterol. 2017;23:7310–7320.
Florence C, Luo F, Xu L, Zhou C. The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Med Care. 2016;54:901–906.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
The study was designed and implemented by Navas, Wadas, Lacy, and Crowell. Chart review, data collection, and data input were performed by Navas, Wadas, and Zbib. Statistical analysis was performed by Crowell. The manuscript was written by Navas, Wadas, Lacy, and Crowell. All authors contributed to the final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest to disclose with regard to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navas, C.M., Wadas, E.D., Zbib, N.H. et al. Gastroparesis and Severity of Delayed Gastric Emptying: Comparison of Patient Characteristics, Treatments and Medication Adverse Events. Dig Dis Sci 66, 526–534 (2021). https://doi.org/10.1007/s10620-020-06258-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06258-7