Abstract
Purpose
To elucidate the electrophysiological predictors of the intramural origins of left ventricular outflow tract-ventricular tachyarrhythmias (LVOT-VAs), and to clarify the involvement of anatomical factors.
Methods
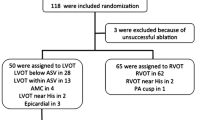
Twenty-nine successfully ablated LVOT-VAs patients with origins in the aortomitral continuity (AMC) (n = 8), aortic sinus of valsalva (ASV) (n = 9), great cardiac vein (GCV) (n = 5), and intramural myocardium (n = 7) were enrolled. Intramural origins were defined as when effective ablation from AMC and epicardium (ASV and/or GCV) was needed. The local activation time difference (LATD) was calculated as follows: (earliest AMC activation) − (earliest epicardial activation), and was presented as an absolute value. Electrophysiological parameters and anatomical factors predisposing the intramural origins were investigated.
Results
LATD of intramural origins was significantly shorter than that of AMC and GCV (4.5 ± 2.6 vs. 12.1 ± 7.4 vs. 17.4 ± 4.7, P < 0.05), respectively. In multivariate logistic regression analysis, LATD was associated with intramural origins (odds ratio: 0.711, confidence interval: 0.514−0.985, P = 0.040). ROC analysis revealed LATD of 7 ms as cut-off value. In computed tomography analysis, some patients who had thick fat tissue below the GCV, and an unusual GCV running pattern might be misdiagnosed as intramural origins.
Conclusion
LATD ≤ 7 ms was associated with intramural origins, but with some anatomical limitations.




Similar content being viewed by others
Data availability
The deidentified participant data will be shared on a request basis. Please directly contact the corresponding author to request data sharing.
Code availability
Not applicable.
References
Yamada T, McElderry HT, Doppalapudi H, Okada T, Murakami Y, Yoshida Y, et al. Idiopathic ventricular arrhythmias originating from the left ventricular summit: anatomic concepts relevant to ablation. Circ Arrhythm Electrophysiol. 2010;3:616–623.2.
Yamada T, Doppalapudi H, Maddox WR, McElderry HT, Plumb VJ, Kay GN. Prevalence and electrocardiographic and electrophysiological characteristics of idiopathic ventricular arrhythmias originating from intramural foci in the left ventricular outflow tract. Circ Arrhythm Electrophysiol. 2016;9:e004079.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7(2):79–108. https://doi.org/10.1016/j.euje.2005.12.014.
Tsang W, Salgo IS, Medvedofsky D, Takeuchi M, Prater D, Weinert L, et al. Transthoracic 3D echocardiographic left heart chamber quantification using an automated adaptive analytics algorithm. JACC Cardiovasc Imaging. 2016;9:769–82.
de Knegt MC, Fuchs A, Weeke P, Mogelvang R, Hassager C, Kofoed KF. Optimisation of coronary vascular territorial 3D echocardiographic strain imaging using computed tomography: a feasibility study using image fusion. Int J Card Imaging. 2016;32:1715–23.
Kamioka M, Hijioka N, Matsumoto Y, Nodera M, Kaneshiro T, Suzuki H, et al. Uncontrolled blood pressure affects atrial remodeling and adverse clinical outcome in paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2018;41:402–10.
Daniels DV, Lu YY, Morton JB, Santucci PA, Akar JG, Green A, et al. Idiopathic epicardial left ventricular tachycardia originating remote from the sinus of Valsalva: electrophysiological characteristics, catheter ablation, and identification from the 12-lead electrocardiogram. Circulation. 2006;113:1659–66.
Hachiya H, Hirao K, Sasaki T, Higuchi K, Hayashi T, Tanaka Y, et al. Novel ECG predictor of difficult cases of outflow tract ventricular tachycardia: peak deflection index on an inferior lead. Circ J. 2010;74:256–61.
Kamioka M, Mathew S, Lin T, Metzner A, Rillig A, Deiss S, et al. Electrophysiological and electrocardiographic predictors of ventricular arrhythmias originating from the left ventricular outflow tract within and below the coronary sinus cusps. Clin Res Cardiol. 2015;104:544–54.
Ouyang F, Mathew S, Wu S, Kamioka M, Metzner A, Xue Y, et al. Ventricular arrhythmias arising from the left ventricular outflow tract below the aortic sinus cusps: mapping and catheter ablation via transseptal approach and electrocardiographic characteristics. Cir Arrythmia Electrophysiol. 2014;7:445–55.
Yamada T, Litovsky SH, Kay GN. The left ventricular ostium: an anatomic concept relevant to idiopathic ventricular arrhythmias. Circ Arrhythm Electrophysiol. 2008;1:396–404.
Yamada S, Chung FP, Lin YJ, Chang SL, Lo LW, Hu YF, et al. Electrocardiographic features of failed and recurrent right ventricular outflow tract catheter ablation of idiopathic ventricular arrhythmias. J Cardiovasc Electrophysiol. 2018;29:127–37.
Heeger CH, Hayashi K, Kuck KH, Ouyang F. Catheter ablation of idiopathic ventricular arrhythmias arising from the cardiac outflow tracts- recent insights and techniques for the successful treatment of common and challenging cases. Circ J. 2016;80:1073–86.
Cheung JW, Anderson RH, Markowitz SM, Lerman BB. Catheter ablation of arrhythmias originating from the left ventricular outflow tract. JACC Clin Electrophysiol. 2019;5:1–12.
Chung FP, Lin CY, Shirai Y, Futyma P, Santangeli P, Lin YJ, et al. Outcomes of catheter ablation of ventricular arrhythmia originating from the left ventricular summit: a multicenter study. Heart Rhythm. 2020;17:1077–83.
Ouyang F, Fotuhi P, Ho SY, Hebe J, Volkmer M, Goya M, et al. Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation. J Am Coll Cardiol. 2002;39:500–8.
Zipse MM, Edward JA, Zheng L, Tzou WS, Borne RT, Sauer WH, et al. Impact of epicardial adipose tissue and catheter ablation strategy on biophysical parameters and ablation lesion characteristics. J Cardiovasc Electrophysiol. 2020;31:1114–24.
Shirai Y, Santangeli P, Liang JJ, Garcia FC, Supple GE, Frankel DS, et al. Anatomical proximity dictates successful ablation from adjacent sites for outflow tract ventricular arrhythmias linked to the coronary venous system. Europace. 2019;21:484–91.
Yamada T, Maddox WR, McElderry HT, Doppalapudi H, Plumb VJ, Kay GN. Radiofrequency catheter ablation of idiopathic ventricular arrhythmias originating from intramural foci in the left ventricular outflow tract: efficacy of sequential versus simultaneous unipolar catheter ablation. Circ Arrhythm Electrophysiol. 2015;8:344–52.
Teh AW, Reddy VY, Koruth JS, Miller MA, Choudry S, D'Avila A, et al. Bipolar radiofrequency catheter ablation for refractory ventricular outflow tract arrhythmias. J Cardiovasc Electrophysiol. 2014;25:1093–9.
Chung FP, Vicera JJB, Lin YJ, Chang SL, Lo LW, Hu YF, et al. Clinical efficacy of open-irrigated electrode cooled with half-normal saline for initially failed radiofrequency ablation of idiopathic outflow tract ventricular arrhythmias. J Cardiovasc Electrophysiol. 2019;30:1508–16.
Kreidieh B, Rodriguez-Manero M, Schurmann P, Ibarra-Cortez SH, Dave AS, Valderrabano M. Retrograde coronary venous ethanol infusion for ablation of refractory ventricular tachycardia. Circ Arrhythm Electrophysiol. 2016;9:e004352.
Benhayon D, Cogan J, Young M. Left atrial appendage as a vantage point for mapping and ablating premature ventricular contractions originating in the epicardial left ventricular summit. Clin Case Rep. 2018;6:1124–7.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Naoko Hijioka, Minoru Nodera, Shinya Yamada, Takashi Kaneshiro, and Yasuchika Takeishi. The first draft of the manuscript was written by Masashi Kamioka, and all authors commented on previous versions of the manuscript.
Corresponding author
Ethics declarations
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the ethical committee of Fukushima Medical University (No. 1808).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Competing interests
Takashi Kaneshiro belongs to department of arrhythmia and cardiac pacing supported by Abbott and Biotronik Co, Ltd. These companies are not associated with contents of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 30665 kb)
Rights and permissions
About this article
Cite this article
Kamioka, M., Hijioka, N., Nodera, M. et al. Electrophysiological properties and involvement of anatomical factors for the prediction of intramural origin in patients with ventricular tachyarrhythmia arising from the left ventricular outflow tract. J Interv Card Electrophysiol 63, 115–123 (2022). https://doi.org/10.1007/s10840-021-00959-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00959-3