Abstract
Purpose
To assess the association between children’s sleep quality and life satisfaction; and to evaluate the underlying mechanisms of this relationship.
Methods
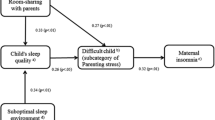
Three pediatric cohorts in the National Institutes of Health (NIH) Environmental influences on Child Health (ECHO) Research Program administered Patient-Reported Outcome Measurement Information System (PROMIS®) parent-proxy measures to caregivers (n = 1111) who reported on their 5- to 9-year-old children’s (n = 1251) sleep quality, psychological stress, general health, and life satisfaction; extant sociodemographic data were harmonized across cohorts. Bootstrapped path modeling of individual patient data meta-analysis was used to determine whether and to what extent stress and general health mediate the relationship between children’s sleep quality and life satisfaction.
Results
Nonparametric bootstrapped path analyses with 1000 replications suggested children’s sleep quality was associated with lower levels of stress and better general health, which, in turn, predicted higher levels of life satisfaction. Family environmental factors (i.e., income and maternal mental health) moderated these relationships.
Conclusion
Children who sleep well have happier lives than those with more disturbed sleep. Given the modifiable nature of children’s sleep quality, this study offers evidence to inform future interventional studies on specific mechanisms to improve children’s well-being.

Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- CFI:
-
Comparative fit index
- CI:
-
Confidence interval
- ECHO:
-
Environmental influences on Child Health Outcomes
- HRQoL:
-
Health-Related Quality of Life
- LRT:
-
Likelihood ratio test
- NIH:
-
National Institutes of Health
- PROMIS:
-
Patient-Reported Outcomes Measurement Information System
- RMSEA:
-
Root Mean Square Error of Approximation
- SD:
-
Standard deviation
- SRMR:
-
Standardized root mean squared residual
- TLI:
-
Tucker–Lewis Index
References
Buysse, D. J. (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9–17.
Ohayon, M., et al. (2017). National Sleep Foundation's sleep quality recommendations: First report. Sleep Health, 3(1), 6–19.
US Department of Health and Human Services. (2014). 2020 Topics & objectives: Sleep health. Washington, DC: US Department of Health and Human Services.
US Department of Health and Human Services. Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030. (2019). Report #7: Assessment and Recommendations for Proposed Objectives for Healthy People 2030. Washington, DC.
Hawkins, S. S., & Takeuchi, D. T. (2016). Social determinants of inadequate sleep in US children and adolescents. Public Health, 138, 119–126.
Hatzinger, M., et al. (2008). Electroencephalographic sleep profiles and hypothalamic-pituitary-adrenocortical (HPA)-activity in kindergarten children: Early indication of poor sleep quality associated with increased cortisol secretion. Journal of Psychiatric Research, 42(7), 532–543.
Javaheri, S., et al. (2008). Sleep quality and elevated blood pressure in adolescents. Circulation, 118(10), 1034–1040.
Van Cauter, E., & Knutson, K. L. (2008). Sleep and the epidemic of obesity in children and adults. European Journal of Endocrinology, 159(Suppl 1), S59–66.
Gregory, A. M., & Sadeh, A. (2012). Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews, 16(2), 129–136.
Beebe, D. W. (2011). Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatric Clinics of North America, 58(3), 649–665.
Matricciani, L., et al. (2019). Children’s sleep and health: A meta-review. Sleep Medicine Reviews, 46, 136–150.
Wong, M. M., et al. (2004). Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism: Clinical & Experimental Research, 28(4), 578–587.
Reidy, B. L., et al. (2016). Prospective associations between chronic youth sleep problems and young adult health. Sleep Health, 2(1), 69–74.
Richards, M., & Huppert, F. A. (2011). Do positive children become positive adults? Evidence from a longitudinal birth cohort study. The Journal of Positive Psychology, 6(1), 75–87.
Steptoe, A., et al. (2008). Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research, 64(4), 409–415.
Strine, T. W., & Chapman, D. P. J. S. M. (2005). Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Medicine, 6(1), 23–27.
Perkinson-Gloor, N., Lemola, S., & Grob, A. (2013). Sleep duration, positive attitude toward life, and academic achievement: The role of daytime tiredness, behavioral persistence, and school start times. Journal of Adolescent, 36(2), 311–318.
Roberts, R. E., Roberts, C. R., & Duong, H. T. (2009). Sleepless in adolescence: Prospective data on sleep deprivation, health and functioning. Journal of Adolescent, 32(5), 1045–1057.
Magee, C. A., Robinson, L., & Keane, C. (2017). Sleep quality subtypes predict health-related quality of life in children. Sleep Medicine, 35, 67–73.
Huebner, E. S. (1991). Initial development of the student’s life satisfaction scale. School Psychology International, 12, 231–240.
Huebner, E. S. (1994). Preliminary development and validation of a multidimensional life satisfaction scale for children. Psychological Assessment, 6(2), 149–158.
Bevans, K. B., Riley, A. W., & Forrest, C. B. (2010). Development of the healthy pathways child-report scales. Quality of Life Research, 19(8), 1195–1214.
Bevans, K. B., Riley, A. W., & Forrest, C. B. (2012). Development of the healthy pathways parent-report scales. Quality of Life Research, 21(10), 1755–1770.
Proctor, C. L., Linley, P. A., & Maltby, J. (2009). Youth life satisfaction: A review of the literature. Journal of Happiness Studies, 10, 583–630.
Huebner, E. S., et al. (2004). Life satisfaction in children and youth: Empirical foundations and implications for school psychologists. Psychology in the Schools, 41(1), 81–93.
Gilman, R., & Huebner, S. (2003). A review of life satisfaction research with children and adolescents. Sch Psych Q, 18, 192–205.
Forrest, C. B., et al. (2018). Development and psychometric evaluation of the PROMIS® Pediatric Life Satisfaction item banks, child-report, and parent-proxy editions. Quality of Life Research, 27(1), 217–234.
Forrest, C. B., et al. (2014). Development of the PROMIS® pediatric global health (PGH-7) measure. Quality of Life Research, 23(4), 1221–1231.
Bevans, K. B., et al. (2018). Psychometric evaluation of the PROMIS® pediatric psychological and physical stress experiences measures. Journal of Pediatric Psychology, 43(6), 678–692.
Suldo, S. M., & Huebner, E. S. (2004). Does life satisfaction moderate the effects of stressful life events on psychopathological behavior during adolescence? School Psychology Quarterly, 19(2), 93–105.
Benham, G. (2010). Sleep: An important factor in stress-health models. Stress and Health, 26(3), 204–214.
Forrest, C. B., et al. (2018). Development and validation of the PROMIS® Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep, 41(6), zsy54.
Blackwell, C. K., et al. (2019). For the ECHO Consortium. General health and life satisfaction in children with chronic illness. Pediatrics, 143(6), e20182988.
Gillman, M. W., & Blaisdell, C. J. (2018). Environmental influences on child health outcomes, a research program of the National Institutes of Health. Current Opinion in Pediatrics, 30(2), 260–262.
Forrest, C. B., et al. (2012). Commentary: The patient-reported outcome measurement information system (PROMIS®) for children and youth: Application to pediatric psychology. Journal of Pediatric Psychology, 37(6), 614–621.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). New York: Guilford Publications.
Yung, Y. F., & Bentler, P. M. (1996). Bootstrapping techniques in analysis of mean and covariance structures. In G. A. Marcoulides & R. E. Schumacker (Eds.), Advanced structural equation modeling: Issues and techniques (pp. 195–226). New York: Lawrence Erlbaum Associates Inc.
Fan, X. (2003). Using commonly available software for bootstrapping in both substantive and measurement analyses. Educational and Psychological Measurement, 63(1), 24–50.
Gitterman, B. A., et al. (2016). Poverty and child health in the United States. Pediatrics, 137(4), e20160339.
Bannink, R., Pearce, A., & Hope, S. (2016). Family income and young adolescents’ perceived social position: Associations with self-esteem and life satisfaction in the UK Millennium Cohort Study. Archives Disease Childhood, 101(10), 917–921.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55.
McEwen, B. S. (2006). Sleep deprivation as a neurobiologic and physiologic stressor: Allostasis and allostatic load. Metabolism, 55, S20–S23.
Barber, L. K., & Munz, D. C. (2011). Consistent-sufficient sleep predicts improvements in self-regulatory performance and psychological strain. Stress and Health, 27(4), 314–324.
C.S. Mott Children’s Hospital National Poll on Children’s Health. (2017).
Hale, L., et al. (2018). Youth screen media habits and sleep: Sleep-friendly screen behavior recommendations for clinicians, Educators, and Parents. Child and Adolescent Psychiatric Clinics, 27(2), 229–245.
Mindell, J. A., Meltzer, L., Carskadon, M. A., & Chervin, R. D. (2009). Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine, 10(7), 771–779.
Wartella, E. A., et al. (2013). Parenting in the age of digital technology: A national survey. Evanston, IL: Center on Media and Human Development, School of Communication, Northwestern University.
Taylor, B., et al. (2011). Prevention of overweight in infancy (POI. nz) study: A randomised controlled trial of sleep, food and activity interventions for preventing overweight from birth. BMC Public Health, 11(1), 942.
Garrison, M., & Christakis, D. (2012). The impact of a healthy media use intervention on sleep in preschool children. Pediatrics, 130(2), 492–499.
Bowers, J., & Moyer, A. (2017). Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: A meta-analysis. Sleep Health, 3(6), 423–431.
Keller, P., et al. (2017). Earlier school start times are associated with higher rates of behavioral problems in elementary schools. Sleep Health, 3(2), 113–118.
Bin, Y. S. (2016). Is sleep quality more important than sleep duration for public health? Sleep, 39(9), 1629–1630.
Upton, P., Lawford, J., & Eiser, C. J. Q. O. L. R. (2008). Parent–child agreement across child health-related quality of life instruments: A review of the literature. Quality of Life Research, 17(6), 895.
McGreavey, J., et al. (2005). The Tayside children's sleep questionnaire: A simple tool to evaluate sleep problems in young children. Child: Care, Health and Development, 31(5), 539–544.
Bruni, O., et al. (1996). The Sleep Disturbance Scale for Children (SDSC) Construct ion and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. Journal of Sleep Research, 5(4), 251–261.
Acknowledgements
The authors wish to thank our ECHO colleagues, the medical, nursing and program staff, as well as the children and families participating in the ECHO cohorts.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023319 with co-funding from the Office of Behavioral and Social Sciences Research (OBSSR; Person Reported Outcomes Core, Blackwell & Forrest), UG3/UH3OD023313 (LeBourgeois & Hartstein); UG3/UH3OD023279 (Elliott), UG3/UH3OD023389 (Ganiban), UG3OD023316 (Hunt), and UG3/UH3OD023253 (Camargo). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
We also acknowledge the contributions of the following ECHO program collaborators: Duke Clinical Research Institute (Coordinating Center), Durham, NC: DKB, PBS, KLN, HB. Medical University of South Carolina, Charleston, SC: JEV, RW. National Institutes of Health (ECHO Program Office), Bethesda, MD: CB. Northwestern University (Person Reported Outcomes (PRO) Core), Evanston, IL: RG, DC. University of Oregon, Eugene, OR: LDL.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Blackwell, C.K., Hartstein, L.E., Elliott, A.J. et al. Better sleep, better life? How sleep quality influences children’s life satisfaction. Qual Life Res 29, 2465–2474 (2020). https://doi.org/10.1007/s11136-020-02491-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02491-9