Abstract
Purpose
The impact of periodic limb movements during sleep (PLMS) on excessive daytime sleepiness (EDS) is controversial. We investigated the relationship between PLMS and EDS in men with obstructive sleep apnea (OSA).
Methods
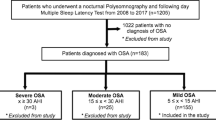
This was a cross-sectional study of men with OSA. PLMS parameters were a PLM index (PLMI) > 15 per hour of sleep and a PLM-arousal index (PLMAI) > 5 per hour of sleep. The Epworth Sleepiness Scale (ESS) and the Beck Depression Inventory were used. EDS was defined as an ESS score ≥ 11. Multivariate logistic regression analysis was performed with adjustments for several covariates.
Results
Of 1111 men with OSA, 14.0% (n = 156) had a PLMI > 15/h, and 3.7% (n = 41) had a PLMAI > 5/h. EDS was noted in 39.5% (n = 439) of men. Men with a PLMI > 15/h were less likely to have EDS (odd ratio [OR], 0.598; 95% confidence interval [CI], 0.414–0.864; p = 0.006). This association remained significant after controlling for age, body mass index, depressive symptoms, total sleep time, and severity of OSA (OR, 0.675; 95% CI, 0.456–0.999; p = 0.049). Men with a PLMAI > 5/h were less likely to have EDS, but this result did not reach statistical significance (OR, 0.550; 95% CI, 0.273–1.109; p = 0.095).
Conclusions
PLMS defined as PLMI > 15/h are significantly and inversely associated with EDS in men with OSA, even after controlling for several confounding variables.
Similar content being viewed by others
References
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Hornyak M, Feige B, Riemann D, Voderholzer U (2006) Periodic leg movements in sleep and periodic limb movement disorder: prevalence, clinical significance and treatment. Sleep Med Rev 10(3):169–177
Al-Alawi A, Mulgrew A, Tench E, Ryan CF (2006) Prevalence, risk factors and impact on daytime sleepiness and hypertension of periodic leg movements with arousals in patients with obstructive sleep apnea. J Clin Sleep Med 2(03):281–287
Chervin RD (2001) Periodic leg movements and sleepiness in patients evaluated for sleep-disordered breathing. Am J Respir Crit Care Med 164(8):1454–1458
Leary EB, Moore HE IV, Schneider LD, Finn LA, Peppard PE, Mignot E (2018) Periodic limb movements in sleep: prevalence and associated sleepiness in the Wisconsin Sleep Cohort. Clin Neurophysiol 129(11):2306–2314
Haba-Rubio J, Marti-Soler H, Tobback N, Andries D, Marques-Vidal P, Vollenweider P, Preisig M, Heinzer R (2018) Clinical significance of periodic limb movements during sleep: the HypnoLaus study. Sleep Med 41:45–50
Szentkirályi A, Stefani A, Hackner H, Czira M, Teismann IK, Völzke H, Stubbe B, Gläser S, Ewert R, Penzel T (2018) Prevalence and associated risk factors of periodic limb movement in sleep in two German population-based studies. Sleep 42(3):zsy237
Montplaisir J, Michaud M, Denesle R, Gosselin A (2000) Periodic leg movements are not more prevalent in insomnia or hypersomnia but are specifically associated with sleep disorders involving a dopaminergic impairment. Sleep Med 1(2):163–167
Sforza E, Nicolas A, Lavigne G, RPGST AG, Petit D, Montplaisir J (1999) EEG and cardiac activation during periodic leg movements in sleep support for a hierarchy of arousal responses. Neurology 52(4):786–791
Ferrillo F, Beelke M, Canovaro P, Watanabe T, Aricò D, Rizzo P, Garbarino S, Nobili L, De Carli F (2004) Changes in cerebral and autonomic activity heralding periodic limb movements in sleep. Sleep Med 5(4):407–412
Guilleminault C, Philip P (1996) Tiredness and somnolence despite initial treatment of obstructive sleep apnea syndrome (what to do when an OSAS patient stays hypersomnolent despite treatment). Sleep 19(suppl_9):S117–S122
Vernet C, Redolfi S, Attali V, Konofal E, Brion A, Frija-Orvoen E, Pottier M, Similowski T, Arnulf I (2011) Residual sleepiness in obstructive sleep apnoea: phenotype and related symptoms. Eur Respir J 38(1):98–105
Haba-Rubio J, Staner L, Krieger J, Macher JP (2005) Periodic limb movements and sleepiness in obstructive sleep apnea patients. Sleep Med 6(3):225–229
Scofield H, Roth T, Drake C (2008) Periodic limb movements during sleep: population prevalence, clinical correlates, and racial differences. Sleep 31(9):1221–1227
Mendelson WB (1996) Are periodic leg movements associated with clinical sleep disturbance? Sleep 19(3):219–223
Coleman RM (1982) Daytime sleepiness in patients with periodic movements in sleep. Sleep 5(suppl_2):S191-S202
Ren R, Huang G, Zhang J, Zhou J, Li Y, Sun Y, Zhou G, Li S, Lu L, Wing Y-K (2016) Age and severity matched comparison of gender differences in the prevalence of periodic limb movements during sleep in patients with obstructive sleep apnea. Sleep Breath 20(2):821–827
Karadeniz D, Ondze B, Besset A, Billiard M (2000) EEG arousals and awakenings in relation with periodic leg movements during sleep. J Sleep Res 9(3):273–277
Montplaisir J, Nicolas A, Godbout R, Walters A (2000) Restless legs syndrome and periodic limb movement disorder. In: Kryger MH, Roth T, Dement WC (eds) Principles and practice of sleep medicine. Saunders, Philadelphia
Bixler EO, Papaliaga MN, Vgontzas AN, LIN HM, Pejovic S, Karataraki M, VELA-BUENO A, Chrousos GP (2009) Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J Sleep Res 18(2):221–228
Theorell-Haglöw J, Miller CB, Bartlett DJ, Yee BJ, Openshaw HD, Grunstein RR (2018) Gender differences in obstructive sleep apnoea, insomnia and restless legs syndrome in adults–what do we know? A clinical update. Sleep Med Rev 38:28–38
Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P (1997) Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord 12(1):61–65
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB (2014) Restless legs syndrome/Willis–Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med 15(8):860–873
Iber C, Iber C (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, vol 1. American Academy of Sleep Medicine, Westchester
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus C, Vaughn BV (2012) The AASM manual for the scoring of sleep and associated events. Rules, terminology and technical specifications, vol 176. American Academy of sleep medicine, Darien
Zucconi M, Ferri R, Allen R, Baier PC, Bruni O, Chokroverty S, Ferini-Strambi L, Fulda S, Garcia-Borreguero D, Hening WA (2006) The official World Association of Sleep Medicine (WASM) standards for recording and scoring periodic leg movements in sleep (PLMS) and wakefulness (PLMW) developed in collaboration with a task force from the International Restless Legs Syndrome Study Group (IRLSSG). Sleep Med 7(2):175–183
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW (2011) The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15(3):377–384
Lee Y (1991) A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol 10:98–113
Shin D-S, Yang KI, Kim D-E, Hwangbo Y, Koo BB, Cho YW (2018) Periodic limb movements during sleep are not associated with hypertension in a clinical cohort of Korean adults. Am J Hypertens 31(11):1228–1233
Ferré S, García-Borreguero D, Allen RP, Earley CJ (2019) New insights into the neurobiology of restless legs syndrome. Neuroscientist 25(2):113–125
Allen RP, Stillman P, Myers AJ (2010) Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in Western Europe: prevalence and characteristics. Sleep Med 11(1):31–37
Ferri R, Rundo F, Zucconi M, Manconi M, Bruni O, Ferini-Strambi L, Fulda S (2015) An evidence-based analysis of the association between periodic leg movements during sleep and arousals in restless legs syndrome. Sleep 38(6):919–924
Gamaldo C, Benbrook AR, Allen RP, Oguntimein O, Earley CJ (2009) Evaluating daytime alertness in individuals with restless legs syndrome (RLS) compared to sleep restricted controls. Sleep Med 10(1):134–138
Trenkwalder C, Paulus W (2010) Restless legs syndrome: pathophysiology, clinical presentation and management. Nat Rev Neurol 6(6):337–346
Claman DM, Ewing SK, Redline S, Ancoli-Israel S, Cauley JA, Stone KL (2013) Periodic leg movements are associated with reduced sleep quality in older men: the MrOS sleep study. J Clin Sleep Med 9(11):1109–1117
Sweetman AM, Lack LC, Catcheside PG, Antic NA, Chai-Coetzer CL, Smith SS, Douglas JA, McEvoy RD (2017) Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev 33:28–38
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments, or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.J., Lee, SA. Periodic limb movements during sleep may reduce excessive daytime sleepiness in men with obstructive sleep apnea. Sleep Breath 24, 1523–1529 (2020). https://doi.org/10.1007/s11325-020-02024-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02024-1