Abstracts
Objectives
Diabetes nephropathy (DN) is one of the complications of diabetes mellitus (DM) marked by gradual progressive loss of renal function. SOCS/JAK/STAT and PI3K/Akt/PTEN signalling pathways are among the chain of interactions implicated in the onset, progression and pathology of DN. Momordica charantia (bitter melon) is often used in folk medicine as therapy for DM due to its hypoglycemic properties. This study was designed to evaluate M. charantia silver nanoparticles’ therapeutic effect on DN-induced by streptozotocin (STZ) in Wistar rats.
Methods
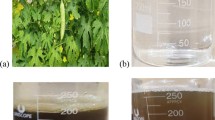
The M. charantia nanoparticles used was synthesized using the filtrate from the plant methanolic extract added to 1 mM concentration of aqueous silver nitrate. DM was induced in Wistar rats by intraperitoneal injection of STZ (65 mg/kg). The animals’ treatment groups were divided into; Diabetic control (65 mg/kg STZ), Control, and groups treated with silver nitrate (10 mg/kg), M. charantia nanoparticles (50 mg/kg), metformin (100 mg/kg), and plant extract (100 mg/kg). Treatment was terminated after 11 days. RT-PCR determined renal mRNA expression of Akt, PI3k, PTEN, TGF-β, JAK2, STAT3, STAT5, SOCS3, SOCS4 and glucokinase (GCK). Consequently, characterized compounds from M. charantia identified from literatures were docked with PI3K, JAK2 and TGF-β and STAT3 to retrieve potential hits.
Results
Oral administration of M. charantia nanoparticles (50 mg/kg) to STZ-induced diabetic untreated rats significantly ((p < 0.05) down-regulated the mRNA expression of Akt, PI3k, TGF-β, JAK2, STAT3 and upregulated the mRNA expression of PTEN, SOCS3 and SOCS4, thus establishing the role of M. charantia nanoparticles in alleviating DN in diabetic rats. Additionally, there was a significant up-regulation of glucose metabolizing gene (glucokinase) upon administering M. charantia nanoparticles. Molecular docking results showed 12 compounds from bitter melon with docking score ranging from −6.114 kcal/mol to −8.221 kcal/mol that are likely to exert anti-diabetic properties.
Conclusion
Observation drawn from this study suggests that M. charantia nanoparticles ameliorate DN through regulation of SOCS/JAK/STAT and PI3K/Akt/PTEN signalling pathways.

















Similar content being viewed by others
References
Hendrick AM, Gibson MV, Kulshreshtha A. Diabetic retinopathy. Primary Care. 2015;42:451–64.
Elekofehinti OO, Ejelonu OC, Kamdem JP, Akinlosotu OB, Famuti A, Adebowale DD, et al. Discovery of potential visfatin activators using in silico docking and ADME predictions as therapy for type 2 diabetes. Beni-Suef University J Basic Appl Sci. 2018;7:241–9.
Karger Publishers [Internet].Centers for disease control and prevention: national diabetes Statistics Report, 2017 [cited Feb 24, 2018]. Available from: https://www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed 15 July 2020.
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98.
Ritz E, Orth SR. Nephropathy in patients with type 2 diabetes mellitus. N Engl J Med. 1999;341:1127–33.
Niewczas MA, Pavkov ME, Skupien J, Smiles A, Md Dom ZI, Wilson JM, et al. A signature of circulating inflammatory proteins and development of end-stage renal disease in diabetes. Nat Med. 2019;25:805–13.
Wang X, Yao B, Wang Y, Fan X, Wang S, Niu A, et al. Macrophage cyclooxygenase-2 protects against development of diabetic nephropathy. Diabetes. 2017;66:494–504.
Goldszmid RS, Trinchieri G. The price of immunity. Nat Immunol. 2012;13:932–8.
Dai T, Natarajan R, Nast CC, LaPage J, Chuang P, Sim J, et al. Glucose and diabetes: effects on podocyte and glomerular p38MAPK, heat shock protein 25, and actin cytoskeleton. Kidney Int. 2006;69:806–14.
Lin S, Teng J, Li J, Sun F, Yuan D, Chang J. Association of chemerin and vascular endothelial growth factor (VEGF) with diabetic nephropathy. Med Sci Monitor: Int Med J Exper Clin Res. 2016;22:3209–14.
Akchurin OM, Kaskel F. Update on inflammation in chronic kidney disease. Blood Purif. 2015;39:84–92.
Pal PB, Sinha K, Sil PC. Mangiferin attenuates diabetic nephropathy by inhibiting oxidative stress mediated signaling cascade, TNFα related and mitochondrial dependent apoptotic pathways instreptozotocin-induced diabetic rats. PLoS. 2014;9:e107220. https://doi.org/10.1371/journal.pone.0107220.
Bell CG, Teschendorff AE, Rakyan VK, Maxwell AP, Beck S, Savage DA. Genome-wide DNA methylation analysis for diabetic nephropathy in type 1 diabetes mellitus. BMC Med Genet. 2010;3:33.
Sapienza C, Lee J, Powell J, Erinle O, Yafai F, Reichert J, et al. DNA methylation profiling identifies epigenetic differences between diabetes patients with ESRD and diabetes patients without nephropathy. Epigenetics. 2011;6:20–8.
Patel RK, Mohan C. PI3K/AKT signaling and systemic autoimmunity. Immunol Res. 2005;31:47–55.
Zhu J, Sun N, Aoudjit L, Li H, Kawachi H, Lemay S, et al. Nephrin mediates actin reorganization via phosphoinositide 3-kinase in podocytes. Kidney Int. 2008;73:556–66.
Ribback S, Cigliano A, Kroeger N, Pilo MG, Terracciano L, Burchardt M, et al. PI3K/AKT/mTOR pathway plays amajor pathogenetic role in glycogen accumulation and tumor development in renal distal tubules of rats and men. Oncotarget. 2015;6:13036–48.
Kato M, Yuan H, Xu Z, et al. Role of the Akt/FoxO3a pathway in TGF-훽1-mediated mesangial cell dysfunction: a novel mechanism related to diabetic kidney disease. J American Soc Neph. 2006;17:3325–35.
Wang K, Wu YG, Su J, et al. Total glucosides of paeony regulates JAK2/STAT3 activation and macrophage proliferation in diabetic rat kidneys. Am J Chinese Med. 2012;3:521.
Mao T, Chen H, Hong L, et al. Pigment epithelium-derived factor inhibits high glucose-induced JAK/STAT signalling pathway activation in human glomerular mesangial cells. Saudi Med J. 2013;8:793.
Koike K, Ueda S, Yamagishi S, Yasukawa H, Kaida Y, Yokoro M, et al. Protective role of JAK/STAT signaling against renal fibrosis in mice with unilateral ureteral obstruction. Clin Immunol. 2014;150:78–87.
Puhr M, Santer FR, Neuwirt H, et al. SOCS-3 antagonises the proliferative and migratory effects of fibroblast growth factor-2 in prostate cancer by inhibition of p44/p42 MAPK signalling. Endocr Relatcancer. 2010;17:525–38.
Shi J, Wei L. Regulation of JAK/STAT signalling by SOCS in the myocardium. Cardiovasc Res. 2016;110:456.
Li D, Lu Z, Xu Z, et al. Spironolactone promotes autophagy via inhibiting PI3K/AKT/mTOR signalling pathway and reduce adhesive capacity damage in podocytes under mechanical stress. Biosci Rep. 2016;36:4.
Zeng R, Xiong Y, Zhu F, Ma Z, Liao W, He Y, et al. Fenofibrate attenuated glucose induced mesangial cells proliferation and extracellular matrix synthesis via PI3K/AKT and ERK1/2. PLoS One. 2013;8:e76836.
Zhang X, Liang D, Chi ZH, et al. Effect of zinc on high glucose-induced epithelial-to-mesenchymal transition in renal tubular epithelial cells. Int J Mol Med. 2015;35:1747–54.
Nahar MK, Zarina-Zakaria U, Fazlul-Bari MD. Green synthesis of silver nanoparticles using Momordica charantia fruit extracts. Adv Mat Res. 2015;1109:35–9.
Abdelwahed W, Degobert G, Stainmesse S, Fessi H. Freeze-drying of nanoparticles: formulation, process and storage considerations. Adv Drug Deliv Rev. 2006;58:1688–713.
Elekofehinti OO, Onunkun AT, Olaleye TM. Cymbopogon citratus (DC.) Stapf mitigates ER-stress induced by streptozotocin in rats via down-regulation of GRP78 and up-regulation of Nrf2 signaling. J Ethnopharmacol. 2020;262:113130.
Iwaloye O, Elekofehinti OO, Babatomiwa K, Fadipe TM, Akinjiyan MO, Ariyo EO, et al. Discovery of TCM derived compounds as wild type and mutant plasmodium falciparum dihydrofolate reductase inhibitors: induced fit docking and ADME studies. Current Drug Discovery Technol. 2020. https://doi.org/10.2174/1570163817999200729122753.
Iwaloye O, Elekofehinti OO, Oluwarotimi EA, Babatomiwa K, Momoh IA. In silico molecular studies of natural compounds as possible anti-Alzheimer’s agents: ligand-based design. Network Model Analys Health Informatics Bioinformatics. 2020;9:54.
Ahamad J, Amin S, Showkat RM. Momordica charantia Linn. (Cucurbitaceae): review on Phytochemistry and pharmacology. Res J Phytochem. 2017;11:53–65.
Iwaloye O, Elekofehinti OO, Oluwarotimi EA, Kikiowo B, Fadipe TM. Insight into glycogen synthase kinase-3β inhibitory activity of phyto-constituents from Melissa officinalis: in silico studies. In Silico Pharmacol. 2020;8:2.
Nasri H, Rafieian-Kopaei M. Diabetes mellitus and renal failure: prevention and management. J Res Med Sci. 2015;20:1112–20.
Nasri H. The awareness of chronic kidney disease and aging; the focus of world kidney day in 2014. J Nephropharmacol. 2014;3:1–2.
Junaid Nazar CM, Kindratt TB, Ahmad SM, Ahmed M, Anderson J. Barriers to the successful practice of chronic kidney diseases at the primary health care level; a systematic review. J Renal Inj Prev. 2014;3:61–7.
Tabatabaeimalazy O, Larijani B, Abdollahi M. Targeting metabolic disorders by natural products. J diabetes Metabol Disorder. 2015:14–57.
Kumar D, Trivedi N, Dixit RK. Herbal medicines used in the traditional indian medicinal system as a therapeutic treatment option for diabetes management: a review. World J Pharm Pharmaceutic Sci. 2015;4:11–29.
Hasan I, Khatoon S. Effect of Momordica charantia (bitter gourd) tablets in diabetes mellitus: type 1 and type 2. Prime Res Med. 2012;2:72–4.
Sărăndan H, Botău D, Ianculov I, Radu F, Rada O, Morar D, et al. The hypoglycemic effect of Momordica charantia Linn in normal and alloxan induced diabetic rabbits. Scientif Papers: Animal Sci Biotechnol. 2010;43:516–8.
Abdal Dayem A, Hossain M, Lee S, et al. The role of reactive oxygen species (ROS) in the biological activities of metallic nanoparticles. Int J Mol Sci. 2017;18:1–20.
Veiseh O, Tang BC, Whitehead KA, Anderson DG, Langer R. Managing diabetes with nanomedicine: challenges and opportunities. Nat Rev Drug Discov. 2015;14:45–57.
Arya AK, Kumar L, Pokharia D, Tripathi K. Applications of nanotechnology in diabetes. Dig J Nanomater Biostruct. 2008;3:221–5.
Leibiger B, Moede T, Uhles S, Barker CJ, Creveaux M, Domin J, et al. Insulin feedback via pi3k-c2a activated pkba/akt1 is required for glucose-stimulated insulin secretion. FASEB J. 2010;24:1824–37.
Vareda PMP, Saldanha LL, Camaforte NA, Violato NM, Dokkedal AL, Bosqueiro JR. Myrcia bella leaf extract prevents hypoglycemic activity via pi3k/Akt insulin pathway. Evid Based Complement Alternat Med. 2014;2014:1–11. https://doi.org/10.1155/2014/543606.
Bosqueiro JR. Myrcia bella leaf extract prevents hypoglycemic activity via pi3k/Akt insulin pathway. Evid Based Complement Alternat Med. 2014;2014:1–11. https://doi.org/10.1155/2014/543606.
Müller C, Dünschede F, Koch E, et al. Alpha-lipoic acid preconditioning reduces ischemia-reperfusion injury of the rat liver via the PI3-kinase/ Akt pathway. Am J Physiol Gastrointest Liver Physiol. 2003;285:769–78.
Okumura H, Nagaya N, Itoh T, Okano I, Hino J, Mori K, et al. Adrenomedullin infusion attenuates myocardial ischemia/reperfusion injury through the phosphatidylinositol 3-kinase/Akt-dependent pathway. Circulation. 2004;109:242–8.
Downward J. PI 3-kinase, Akt and cell survival. Sem Cell Devel Bio. 2004;15:177–82.
Zhang D, Shao S, Shuai H, Ding Y, Shi W, Wang D, et al. SDF-1훼 reduces fibronectin expression in rat mesangial cells induced by TGF-훽1 and high glucose through PI3K/Akt pathway. Exp Cell Res. 2013;319:1796–803.
Wan-Xin T, Tian-Lei C, Ben W, Wei-Hua W, Ping F. Effect of mitofusin 2 overexpression on the proliferation and apoptosis of high-glucose induced rat glomerular mesangial cells. J Nephrol. 2012;25:1023–30.
Wang XM, Yao Liu MSX, Hao J, Liu QJ, Gao F. Interplay between the notch and PI3K/Akt pathways in high glucose-induced podocyte apoptosis. Am J Physiol-Renal Physiol. 2014;306:205–21.
Zhao S, Zhu L, Duan H, Liu S, Liu Q, Liu W, et al. PI3K/Akt pathway mediates high glucose-induced lipid accumulation in human renal proximal tubular cells via spliced XBP-1. J Cell Biochem. 2012;113:3288–98.
Hao J, Zhu L, Li F, Liu Q, Zhao X, Liu S, et al. Phospho-mTOR: a novel target in regulation of renal lipid metabolism abnormality of diabetes. Exp Cell Res. 2013;319:2296–306.
Huang C, Lin MZ, Cheng D, Braet F, Pollock CA, Chen XM. KCa3.1 mediates dysfunction of tubular autophagy in diabetic kidneys via PI3k/Akt/mTOR signaling pathways. Scientific Reports. 2016; 6.
Chung CH, Fan J, Lee EY, Kang JS, Lee SJ, Pyagay PE, et al. Effects of tumor necrosis factor-훼 on podocyte expression of monocyte chemoattractant protein-1 and in diabetic nephropathy. Nephron Extra. 2015;5:1–18.
Qin D, Zhang G, Xu X, Wang L. The PI3K/Akt signaling pathway mediates the high glucose-induced expression of extracellular matrix molecules in human retinal pigment epithelial cells. J Diabetes Res. 2015;2015:1–11. https://doi.org/10.1155/2015/920280.
Qin D, Zheng XX, Jiang YR. Apelin-13 induces proliferation, migration, and collagen I mRNA expression in human RPE cells via PI3K/Akt and MEK/Erk signaling pathways. Mol Vis. 2013;19:2227–36.
Zhou M, Li P, Kang Q. Shen-Yuan-Dan capsule inhibiting inflammatory reaction by regulating insulin receptor substrate 1/PI3K/Akt/NF-kappaB signaling pathway in Apoliprotein E knockout mice fed with a high-fat diet. Acta Cardiol Sin. 2014;33:285–91.
Hong JN, Li WW, Wang LL. Jiangtang decoction ameliorate diabetic nephropathy through the regulation of PI3K/Akt-mediated NF-kappaB pathways in KK-Ay mice. Chin Med. 2012;12:13.
Wang J, Zhou J, Wang Y, et al. Qiliqiangxin protects against anoxic injury in cardiac microvascular endothelial cells via NRG-1/ErbB-PI3K/Akt/mTOR pathway. J Cell Mol Med. 2017.
Deng Z, Yuan C, Yang J, Peng Y, Wang W, Wang Y, et al. behavioral defects induced by chronic social defeat stress are protected by M. charantia polysaccharides via attenuation of JNK3/PI3K/AKT neuroinflammatory pathway. Annals Trans Med. 2019;7:1.
Molinari F, Frattini M. Functions and regulation of the PTEN gene in colorectal cancer. Front Oncol. 2013;3:326.
Wang YY, Liu RX, Guo B, Xiao Y, Shi MJ, Pi MJ, et al. Down-regulation of PTEN expression in kidney and its role in development of diabetic nephropathy in rats. Sheng Li Xue Bao. 2011;63:325–32.
Lee EY, Chung CH, Khoury CC. The monocyte chemoattractant protein-1/CCR2 loop, inducible by TGF-훽, increases podocyte motility and albumin permeability. Am J Physiol—Renal Physiol. 2009;297:85–94.
Waasdorp M, Duitman J, Florquin S, Spek CA. Protease-activated receptor-1 deficiency protects against streptozotocin-induced diabetic nephropathy in mice. Sci Rep. 2016;6.
Sutariya B, Jhonsa D, Saraf NM. TGF-훽: the connecting link between nephropathy and fibrosis. Immunopharmacol Immunotoxicol. 2016;38:39–49.
Wang K, Wu YG, Su J, et al. Total glucosides of paeony regulates JAK2/STAT3 activation and macrophage proliferation in diabetic rat kidneys. Am J Chin Med. 2011;40:521.
Mao T, Chen H, Hong L, et al. Pigment epithelium-derived factor inhibits high glucose-induced JAK/STAT signalling pathway activation in human glomerular mesangial cells. Saudi Med J. 2013;34:793.
Tamiya T, Kashiwagi I, Takahashi R, Yasukawa H, Yoshimura A. Suppressors of cytokine signaling (SOCS) proteins and JAK/STAT pathways: regulation of T-cell inflammation by SOCS1 and SOCS3. Arterioscler Thromb Vasc Biol. 2011;31:980–5.
Yoshimura A, Naka T, Kubo M. SOCS proteins, cytokine signalling and immune regulation. Nat Rev Immunol. 2007;7:454–65.
Ortizmuñoz G, Lopezparra V, Lopezfranco O, et al. Suppressors of cytokine signaling abrogates diabetic nephropathy. J Am Soc Nephrol. 2010;21:763–72.
Lu TC, Wang ZH, Feng X, Chuang PY, Fang W, Shen Y, et al. Knockdown of Stat3 activity in vivo prevents diabetic glomerulopathy. Kidney Int. 2009;76:63–71.
Banes AK, Shaw S, Jenkins J, et al. Angiotensin II blocrade prevents hyperglycemia—induced activation of JAK and STAK proteins in diabetic rat kidney glomemli. Am J Phys Renal Phys. 2004;286:653–9.
Fang Y, Sai-cong S, Hai-ying W. Intervention effects of compound Houttuyniae Herba to diabetic renal damage based on SOCS-JAK/STAT negative feedback regulation. Chinese Herbal Med. 2018;10:424–30. https://doi.org/10.1016/j.chmed.2018.08.005.
Yang L, Xue J, Meng X, Wang Y, Wu L, Cuiyan L, et al. Effects of total flavonoids from Oxytropis falcata Bunge on the SOCS/JAK/STAT inflammatory signaling pathway in the kidneys of diabetic nephropathy model mice. Eur J Inflammation. 2019;17:1–12.
Ortiz-Muñoz G, Lopez-Parra V, Lopez-Franco O, Fernandez-Vizarra P, Mallavia B, Flores C, et al. Suppressors of cytokine signaling abrogate diabetic nephropathy. J Am Soc Nephrol. 2010;21:763–72.
Barzilai N, Rossetti L. Role of glucokinase and glucose-6-phosphatase in the acute and chronic regulation of hepatic glucose fluxes by insulin. J Biol Chem. 1993;268:25019–25.
McCarthy MI, Hattersley AT. Molecular diagnostics in monogenic and multifactorial forms of type 2 diabetes. Expert Rev Mol Diagn. 2001;1:403–12.
Basu A, Basu R, Shah P, Vella A, Johnson CM, Nair KS, et al. Effects of type 2 diabetes on the ability of insulin and glucose to regulate splanchnic and muscle glucose metabolism: evidence for a defect in hepatic glucokinase activity. Diabetes. 2000;49:272–83.
Ferris SA. Hepatic glucokinase activity in human diabetics and nondiabetics. Metabolism. 1964;13:1478–81.
Zhang X, Liang W, Mao Y, Li H, Yang Y, Tan H. Hepatic glucokinase activity is the primary defect in alloxan-induced diabetes of mice. Biomed Pharmacother. 2009;63(1):80–6.
Kolawole OT, Akanji MA. Effects of extract of leaves of Newbouldia laevis on the activities of some enzymes of hepatic glucose metabolism in diabetic rats. African J Biotech. 2014;13:2273–81.
Acknowledgements
This research received no grants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All institutional and national guidelines for the care and use of laboratory animals were followed.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elekofehinti, O.O., Oyedokun, V.O., Iwaloye, O. et al. Momordica charantia silver nanoparticles modulate SOCS/JAK/STAT and P13K/Akt/PTEN signalling pathways in the kidney of streptozotocin-induced diabetic rats. J Diabetes Metab Disord 20, 245–260 (2021). https://doi.org/10.1007/s40200-021-00739-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00739-w