Abstract
Background and Objective
Fetal circulation is unique and the parameters describing hemodynamic status during development are critical for constructing a fetal physiologically based pharmacokinetic model. To date, a comprehensive review of circulatory changes during fetal development, with a specific focus on developing these models, has not been reported. The objective of this work was to collate, analyze, and mathematically describe physiological information on fetal cardiac output and tissue blood flows during development.
Methods
A comprehensive literature search was carried out to collate and evaluate the changes to fetal cardiac output and fetal tissue blood flows during growth. The collated data were assessed, integrated, and analyzed to establish continuous mathematical functions describing the average parameter changes and variability during development.
Results
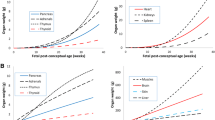
Data were available for fetal cardiac output (14 Doppler studies), blood flow through the fetal umbilical vein (15 studies), ductus venosus (6 studies), liver veins (5 studies), brain (4 studies), lungs (5 studies), and kidneys (2 studies). Fetal cardiac output is described as either an age- or weight-dependent function. The latter is preferred as it generates an individualized cardiac output that is correlated to the fetal body weight. Blood flow as a proportion of fetal cardiac output to the liver, placenta, brain, kidneys, and lungs was age varying, whilst for the adipose, bone, heart, muscle, and skin the blood flow proportions were fixed. The pattern of change (with respect to direction and pace) for each of these parameters was different.
Conclusions
Despite limitations in the availability of some values, the collected data provide a useful resource for fetal physiologically based pharmacokinetic modeling. Potential applications of these data include predicting xenobiotic exposure and risk assessment in the fetus following the administration of maternally dosed drugs or unintended exposure to environmental toxicants.








Similar content being viewed by others
References
Murphy PJ. The fetal circulation. CEACCP. 2005;5:107–12.
Kiserud T. Physiology of the fetal circulation. Semin Fetal Neonatal Med. 2005;10:493–503.
Vimpeli T, Huhtala H, Wilsgaard T, Acharya G. Fetal aortic isthmus blood flow and the fraction of cardiac output distributed to the upper body and brain at 11–20 weeks of gestation. Ultrasound Obstet Gynecol. 2009;33:538–44.
Finnemore A, Groves A. Physiology of the fetal and transitional circulation. Semin Fetal Neonatal Med. 2015;20:210–6.
Gaohua L, Abduljalil K, Jamei M, Johnson TN, Rostami-Hodjegan A. A pregnancy physiologically based pharmacokinetic (p-PBPK) model for disposition of drugs metabolized by CYP1A2, CYP2D6 and CYP3A4. Br J Clin Pharmacol. 2012;74:873–85.
Abduljalil K, Furness P, Johnson TN, Rostami-Hodjegan A, Soltani H. Anatomical, physiological and metabolic changes with gestational age during normal pregnancy: a database for parameters required in physiologically based pharmacokinetic modelling. Clin Pharmacokinet. 2012;51:365–96.
Zhang Z, Imperial MZ, Patilea-Vrana GI, Wedagedera J, Gaohua L, Unadkat JD. Development of a novel maternal-fetal physiologically based pharmacokinetic model I: insights into factors that determine fetal drug exposure through simulations and sensitivity analyses. Drug Metab Dispos. 2017;45:920–38.
Kapraun DF, Wambaugh JF, Setzer RW, Judson RS. Empirical models for anatomical and physiological changes in a human mother and fetus during pregnancy and gestation. PLoS ONE. 2019;14:e0215906.
Dallmann A, Ince I, Coboeken K, Eissing T, Hempel G. A physiologically based pharmacokinetic model for pregnant women to predict the pharmacokinetics of drugs metabolized via several enzymatic pathways. Clin Pharmacokinet. 2018;57:749–68.
Clewell HJ, Gearhart JM, Gentry PR, Covington TR, VanLandingham CB, Crump KS, et al. Evaluation of the uncertainty in an oral reference dose for methylmercury due to interindividual variability in pharmacokinetics. Risk Anal. 1999;19:547–58.
Abduljalil K, Johnson TN, Rostami-Hodjegan A. Fetal physiologically-based pharmacokinetic models: systems information on fetal biometry and gross composition. Clin Pharmacokinet. 2018;57:1149–71.
Abduljalil K, Jamei M, Johnson TN. Fetal physiologically based pharmacokinetic models: systems information on the growth and composition of fetal organs. Clin Pharmacokinet. 2019;58:23562.
Abduljalil K, Jamei M, Johnson TN. Fetal physiologically based pharmacokinetic models: systems information on fetal blood components and binding proteins. Clin Pharmacokinet. 2020;59:629–42.
Schoennagel BP, Yamamura J, Kording F, Fischer R, Bannas P, Adam G, et al. Fetal dynamic phase-contrast MR angiography using ultrasound gating and comparison with Doppler ultrasound measurements. Eur Radiol. 2019;29:4169–76.
Zheng M, Schaal M, Chen Y, Li X, Shentu W, Zhang P, et al. Real-time 3-dimensional echocardiographic assessment of ventricular volume, mass, and function in human fetuses. PLoS ONE. 2013;8:e58494.
Uittenbogaard LB, Haak MC, Spreeuwenberg MD, van Vugt JM. Fetal cardiac function assessed with four-dimensional ultrasound imaging using spatiotemporal image correlation. Ultrasound Obstet Gynecol. 2009;33:272–81.
Molina FS, Faro C, Sotiriadis A, Dagklis T, Nicolaides KH. Heart stroke volume and cardiac output by four-dimensional ultrasound in normal fetuses. Ultrasound Obstet Gynecol. 2008;32:181–7.
DeKoninck P, Steenhaut P, Van Mieghem T, Mhallem M, Richter J, Bernard P, et al. Comparison of Doppler-based and three-dimensional methods for fetal cardiac output measurement. Fetal Diagn Ther. 2012;32:72–8.
De Smedt MC, Visser GH, Meijboom EJ. Fetal cardiac output estimated by Doppler echocardiography during mid- and late gestation. Am J Cardiol. 1987;60:338–42.
Mielke G, Benda N. Cardiac output and central distribution of blood flow in the human fetus. Circulation. 2001;103:1662–8.
Rasanen J, Wood DC, Weiner S, Ludomirski A, Huhta JC. Role of the pulmonary circulation in the distribution of human fetal cardiac output during the second half of pregnancy. Circulation. 1996;94:1068–73.
Lisowski LA, Verheijen PM, De Smedt MM, Visser GH, Meijboom EJ. Altered fetal circulation in type-1 diabetic pregnancies. Ultrasound Obstet Gynecol. 2003;21:365–9.
Rudolph AM, Iwamoto HS, Teitel DF. Circulatory changes at birth. J Perinat Med. 1988;16(Suppl. 1):9–21.
Godfrey ME, Friedman KG, Drogosz M, Rudolph AM, Tworetzky W. Cardiac output and blood flow redistribution in fetuses with D-loop transposition of the great arteries and intact ventricular septum: insights into pathophysiology. Ultrasound Obstet Gynecol. 2017;50:612–7.
Hamill N, Yeo L, Romero R, Hassan SS, Myers SA, Mittal P, et al. Fetal cardiac ventricular volume, cardiac output, and ejection fraction determined with 4-dimensional ultrasound using spatiotemporal image correlation and virtual organ computer-aided analysis. Am J Obstet Gynecol. 2011;205(76):e1-10.
Vimpeli T, Huhtala H, Wilsgaard T, Acharya G. Fetal cardiac output and its distribution to the placenta at 11–20 weeks of gestation. Ultrasound Obstet Gynecol. 2009;33:265–71.
Veille J-C, Hanson RA, Tatum K, Kelley K. Quantitative assessment of human fetal renal blood flow. Am J Obstet Gynecol. 1993;169:1399–402.
Kiserud T, Ebbing C, Kessler J, Rasmussen S. Fetal cardiac output, distribution to the placenta and impact of placental compromise. Ultrasound Obstet Gynecol. 2006;28:126–36.
Sutton MS, Groves A, MacNeill A, Sharland G, Allan L. Assessment of changes in blood flow through the lungs and foramen ovale in the normal human fetus with gestational age: a prospective Doppler echocardiographic study. Br Heart J. 1994;71:232–7.
Prsa M, Sun L, van Amerom J, Yoo SJ, Grosse-Wortmann L, Jaeggi E, et al. Reference ranges of blood flow in the major vessels of the normal human fetal circulation at term by phase-contrast magnetic resonance imaging. Circ Cardiovasc Imaging. 2014;7:663–70.
Allan LD, Chita SK, Al-Ghazali W, Crawford DC, Tynan M. Doppler echocardiographic evaluation of the normal human fetal heart. Br Heart J. 1987;57:528–33.
Kenny JF, Plappert T, Doubilet P, Saltzman DH, Cartier M, Zollars L, et al. Changes in intracardiac blood flow velocities and right and left ventricular stroke volumes with gestational age in the normal human fetus: a prospective Doppler echocardiographic study. Circulation. 1986;74:1208–16.
Alsolai AA, Bligh LN, Greer RM, Kumar S. Relationship of prelabor fetal cardiac function with intrapartum fetal compromise and neonatal status at term. Ultrasound Obstet Gynecol. 2018;51:799–805.
Rizzo G, Arduini D, Valensise H, Romanini C. Effects of behavioural states on cardiac output in the healthy human fetus at 36–38 weeks of gestation. Early Hum Dev. 1990;23:109–15.
Ho DY, Josowitz R, Katcoff H, Griffis HM, Tian Z, Gaynor JW, et al. Mid-gestational fetal placental blood flow is diminished in the fetus with congenital heart disease. Prenat Diagn. 2020;40:1432–8.
Seed M, van Amerom JF, Yoo SJ, Al Nafisi B, Grosse-Wortmann L, Jaeggi E, et al. Feasibility of quantification of the distribution of blood flow in the normal human fetal circulation using CMR: a cross-sectional study. J Cardiovasc Magn Reson. 2012;14:79.
Simioni C, Araujo Junior E, Martins WP, Rolo LC, Rocha LA, Nardozza LM, et al. Fetal cardiac output and ejection fraction by spatio-temporal image correlation (STIC): comparison between male and female fetuses. Rev Bras Cir Cardiovasc. 2012;27:275–82.
Acharya G, Wilsgaard T, Berntsen GKR, Maltau JM, Kiserud T. Doppler-derived umbilical artery absolute velocities and their relationship to fetoplacental volume blood flow: a longitudinal study. Ultrasound Obstet Gynecol. 2005;25:444–53.
Boito S, Struijk PC, Ursem NT, Stijnen T, Wladimiroff JW. Umbilical venous volume flow in the normally developing and growth-restricted human fetus. Ultrasound Obstet Gynecol. 2002;19:344–9.
Flo K, Wilsgaard T, Acharya G. Longitudinal reference ranges for umbilical vein blood flow at a free loop of the umbilical cord. Ultrasound Obstet Gynecol. 2010;36:567–72.
Rizzo G, Capponi A, Pietrolucci ME, Arduini D. Umbilical vein blood flow at 11 + 0 to 13 + 6 weeks of gestation. J Matern Fetal Neonatal Med. 2010;23:315–9.
Rizzo G, Rizzo L, Aiello E, Allegra E, Arduini D. Modelling umbilical vein blood flow normograms at 14–40 weeks of gestation by quantile regression analysis. J Matern Fetal Neonatal Med. 2016;29:701–6.
Kessler J, Rasmussen S, Godfrey K, Hanson M, Kiserud T. Longitudinal study of umbilical and portal venous blood flow to the fetal liver: low pregnancy weight gain is associated with preferential supply to the fetal left liver lobe. Pediatr Res. 2008;63:315–20.
Nyberg MK, Johnsen SL, Rasmussen S, Kiserud T. Fetal breathing is associated with increased umbilical blood flow. Ultrasound Obstet Gynecol. 2010;36:718–23.
Lees C, Albaiges G, Deane C, Parra M, Nicolaides KH. Assessment of umbilical arterial and venous flow using color Doppler. Ultrasound Obstet Gynecol. 1999;14:250–5.
Bellotti M, Pennati G, De Gasperi C, Battaglia FC, Ferrazzi E. Role of ductus venosus in distribution of umbilical blood flow in human fetuses during second half of pregnancy. Am J Physiol Heart Circ Physiol. 2000;279:H1256–63.
Sutton MS, Theard MA, Bhatia SJ, Plappert T, Saltzman DH, Doubilet P. Changes in placental blood flow in the normal human fetus with gestational age. Pediatr Res. 1990;28:383–7.
Tchirikov M, Rybakowski C, Huneke B, Schroder HJ. Blood flow through the ductus venosus in singleton and multifetal pregnancies and in fetuses with intrauterine growth retardation. Am J Obstet Gynecol. 1998;178:943–9.
Opheim GL, Moe Holme A, Blomhoff Holm M, Melbye Michelsen T, Muneer Zahid S, Paasche Roland MC, et al. The impact of umbilical vein blood flow and glucose concentration on blood flow distribution to the fetal liver and systemic organs in healthy pregnancies. FASEB J. 2020;34:12481–91.
Opheim GL, Henriksen T, Haugen G. The effect of a maternal meal on fetal liver blood flow. PLoS ONE. 2019;14:e0216176.
Ferrazzi E, Rigano S, Bozzo M, Bellotti M, Giovannini N, Galan H, et al. Umbilical vein blood flow in growth-restricted fetuses. Ultrasound Obstet Gynecol. 2000;16:432–8.
Barbera A, Galan HL, Ferrazzi E, Rigano S, Jozwik M, Battaglia FC, et al. Relationship of umbilical vein blood flow to growth parameters in the human fetus. Am J Obstet Gynecol. 1999;181:174–9.
Gill RW, Kossoff G, Warren PS, Garrett WJ. Umbilical venous flow in normal and complicated pregnancy. Ultrasound Med Biol. 1984;10:349–63.
Battaglia FC. Clinical studies linking fetal velocimetry, blood flow and placental transport in pregnancies complicated by intrauterine growth retardation (IUGR). Trans Am Clin Climatol Assoc. 2003;114:305–13.
Singh Y, Tissot C. Echocardiographic evaluation of transitional circulation for the neonatologists. Front Pediatr. 2018;6:140.
Bellotti M, Pennati G, De Gasperi C, Bozzo M, Battaglia FC, Ferrazzi E. Simultaneous measurements of umbilical venous, fetal hepatic, and ductus venosus blood flow in growth-restricted human fetuses. Am J Obstet Gynecol. 2004;190:1347–58.
Haugen G, Kiserud T, Godfrey K, Crozier S, Hanson M. Portal and umbilical venous blood supply to the liver in the human fetus near term. Ultrasound Obstet Gynecol. 2004;24:599–605.
Kessler J, Rasmussen S, Kiserud T. The fetal portal vein: normal blood flow development during the second half of human pregnancy. Ultrasound Obstet Gynecol. 2007;30:52–60.
Kiserud T, Rasmussen S, Skulstad S. Blood flow and the degree of shunting through the ductus venosus in the human fetus. Am J Obstet Gynecol. 2000;182(1 Pt 1):147–53. https://doi.org/10.1016/s0002-9378(00)70504-7.
Zvanca M, Gielchinsky Y, Abdeljawad F, Bilardo CM, Nicolaides KH. Hepatic artery Doppler in trisomy 21 and euploid fetuses at 11–13 weeks. Prenat Diagn. 2011;31:22–7.
Ebbing C, Rasmussen S, Godfrey KM, Hanson MA, Kiserud T. Hepatic artery hemodynamics suggest operation of a buffer response in the human fetus. Reprod Sci. 2008;15:166–78.
Edelstone DI, Rudolph AM, Heymann MA. Liver and ductus venosus blood flows in fetal lambs in utero. Circ Res. 1978;42:426–33.
International Commission on Radiological Protection. Basic anatomical and physiological data for use in radiological protection reference values. Ann ICRP. 2002;32:1–277.
Rudolph AM, Heymann MA, Teramo KAW, Barrett CT, Räihä NCR. Studies on the circulation of the previable human fetus. Pediatr Res. 1971;5:452–65.
Veille J-C, Hanson R, Tatum K. Longitudinal quantitation of middle cerebral artery blood flow in normal human fetuses. Am J Obstet Gynecol. 1993;169:1393–8.
Konje JC, Abrams K, Bell SC, de Chazal RC, Taylor DJ. The application of color power angiography to the longitudinal quantification of blood flow volume in the fetal middle cerebral arteries, ascending aorta, descending aorta, and renal arteries during gestation. Am J Obstet Gynecol. 2000;182:393–400.
Avitan T, Sanders A, Brain U, Rurak D, Oberlander TF, Lim K. Variations from morning to afternoon of middle cerebral and umbilical artery blood flow, and fetal heart rate variability, and fetal characteristics in the normally developing fetus. J Clin Ultrasound. 2018;46(4):235–40. https://doi.org/10.1002/jcu.22569.
Vali P, Lakshminrusimha S. The fetus can teach us: oxygen and the pulmonary vasculature. Children (Basel). 2017;4:67.
Hislop A, Reid L. Intra-pulmonary arterial development during fetal life-branching pattern and structure. J Anat. 1972;113:35–48.
Andriani G, Persico A, Tursini S, Ballone E, Cirotti D, Lelli CP. The renal-resistive index from the last 3 months of pregnancy to 6 months old. BJU Int. 2001;87:562–4.
Ji EK, Kwon TH. P45.13: imaging of fetal coronary arteries and pulmonary veins with gray and color flow Doppler sonography. Ultrasound Obstet Gynecol. 2007;30:627.
Baschat AA, Gembruch U, Reiss I, Gortner L, Diedrich K. Demonstration of fetal coronary blood flow by Doppler ultrasound in relation to arterial and venous flow velocity waveforms and perinatal outcome: the ‘heart-sparing effect.’ Ultrasound Obstet Gynecol. 1997;9:162–72.
Baschat AA, Muench MV, Gembruch U. Coronary artery blood flow velocities in various fetal conditions. Ultrasound Obstet Gynecol. 2003;21:426–9.
Rudolph AM, Heymann MA. Circulatory changes during growth in the fetal lamb. Circ Res. 1970;26:289–99.
Ebbing C, Rasmussen S, Godfrey KM, Hanson MA, Kiserud T. Fetal superior mesenteric artery: longitudinal reference ranges and evidence of regulatory link to portal liver circulation. Early Hum Dev. 2009;85:207–13.
Matasova K, Dokus K, Zubor P, Danko J, Zibolen M. Physiological changes in blood flow velocities in the superior mesenteric and coeliac artery in healthy term fetuses and newborns during perinatal period. J Matern Fetal Neonatal Med. 2011;24:827–32.
Ebbing C, Rasmussen S, Godfrey KM, Hanson MA, Kiserud T. Fetal celiac and splenic artery flow velocity and pulsatility index: longitudinal reference ranges and evidence for vasodilation at a low portocaval pressure gradient. Ultrasound Obstet Gynecol. 2008;32:663–72.
Valentin J. Basic anatomical and physiological data for use in radiological protection: reference values: ICRP Publication 89. Ann ICRP. 2002;32:1–277.
Jensen A, Hohmann M, Kunzel W. Dynamic changes in organ blood flow and oxygen consumption during acute asphyxia in fetal sheep. J Dev Physiol. 1987;9:543–59.
Tan W, Riggs KW, Thies RL, Rurak DW. Use of an automated fluorescent microsphere method to measure regional blood flow in the fetal lamb. Can J Physiol Pharmacol. 1997;75:959–68.
Wu PY, Wong WH, Guerra G, Miranda R, Godoy RR, Preston B, et al. Peripheral blood flow in the neonate; 1. Changes in total, skin, and muscle blood flow with gestational and postnatal age. Pediatr Res. 1980;14:1374–8.
Sepulveda W, Bower S, Nicolaidis P, De Swiet M, Fisk NM. Discordant blood flow velocity waveforms in left and right brachial arteries in growth-retarded fetuses. Obstet Gynecol. 1995;86:734–8.
Rizzo G, Capponi A, Chaoui R, Taddei F, Arduini D, Romanini C. Blood flow velocity waveforms from peripheral pulmonary arteries in normally grown and growth-retarded fetuses. Ultrasound Obstet Gynecol. 1996;8:87–92.
Konje JC, Taylor DJ, Rennie MJ. Application of ultrasonic transit time flowmetry to the measurement of umbilical vein blood flow at caesarean section. Br J Obstet Gynaecol. 1996;103:1004–8.
Xia B, Heimbach T, Gollen R, Nanavati C, He H. A simplified PBPK modeling approach for prediction of pharmacokinetics of four primarily renally excreted and CYP3A metabolized compounds during pregnancy. AAPS J. 2013;15:1012–24.
De Sousa MM, Hirt D, Urien S, Valade E, Bouazza N, Foissac F, et al. Physiologically-based pharmacokinetic modeling of renally excreted antiretroviral drugs in pregnant women. Br J Clin Pharmacol. 2015;80:1031–41.
Luecke RH, Wosilait WD, Pearce BA, Young JF. A physiologically based pharmacokinetic computer model for human pregnancy. Teratology. 1994;49:90–103.
Bravo-Valenzuela NJ, Peixoto AB, Carrilho MC, Siqueira Pontes AL, Chagas CC, Simioni C, et al. Fetal cardiac function by three-dimensional ultrasound using 4D-STIC and VOCAL: an update. J Ultrason. 2019;19:287–94.
Sato M, Tsukimori K, Fujita Y, Morihana E, Fusazaki N, Takahata Y, et al. Prenatal diagnosis of coarctation of the aorta using 4-dimensional fetal echocardiography with power Doppler imaging and spatiotemporal image correlation. J Ultrasound Med. 2013;32:719–21.
Rizzo G, Capponi A, Cavicchioni O, Vendola M, Arduini D. Fetal cardiac stroke volume determination by four-dimensional ultrasound with spatio-temporal image correlation compared with two-dimensional and Doppler ultrasonography. Prenat Diagn. 2007;27:1147–50.
Deng J, Rodeck CH. Current applications of fetal cardiac imaging technology. Curr Opin Obstet Gynecol. 2006;18:177–84.
Chaoui R, Hoffmann J, Heling KS. Three-dimensional (3D) and 4D color Doppler fetal echocardiography using spatio-temporal image correlation (STIC). Ultrasound Obstet Gynecol. 2004;23:535–45.
Crispi F, Gratacos E. Fetal cardiac function: technical considerations and potential research and clinical applications. Fetal Diagn Ther. 2012;32:47–64.
Acknowledgements
We thank Eleanor Savill and Anna Kenworthy for their assistance with collecting the references and preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the conduct of this study or the preparation of this article.
Conflict of Interest
All authors are full-time employees of Certara UK Limited (Simcyp Division). The activities of Certara are supported by a consortium of pharmaceutical companies. The Simcyp Simulator is currently freely available, following completion of the training workshop, to approved members of academic institutions and other not-for-profit organizations for research and teaching purposes.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Availability material
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abduljalil, K., Pan, X., Clayton, R. et al. Fetal Physiologically Based Pharmacokinetic Models: Systems Information on Fetal Cardiac Output and Its Distribution to Different Organs during Development. Clin Pharmacokinet 60, 741–757 (2021). https://doi.org/10.1007/s40262-020-00973-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-020-00973-0