Abstract
Objectives
Chemotherapy is increasingly a preference-based choice among women diagnosed with early-stage breast cancer. Multicriteria decision analysis (MCDA) is a promising but underutilized method to facilitate shared decision making. We explored the feasibility of conducting an MCDA using direct rank ordering versus a time trade-off (TTO) to assess chemotherapy choice in a large population-based sample.
Methods
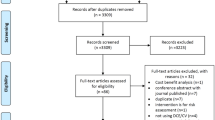
We surveyed 904 early-stage breast cancer survivors who were within 5 years of diagnosis and reported to the Western Washington State Cancer System and Kaiser Permanente Northern California registries. Direct rank ordering of 11 criteria and TTO surveys were conducted from September 2015 to July 2016; clinical data were obtained from registries or medical records. Multivariable regressions estimated post hoc associations between the MCDA, TTO, and self-reported chemotherapy receipt, considering covariates.
Results
Survivors ranged in age from 25 to 74 years and 73.9% had stage I tumors. The response rate for the rank ordering was 81.0%; TTO score was 94.2%. A one-standard deviation increase in the difference between the chemotherapy and no chemotherapy MCDA scores was associated with a 75.1% (95% confidence interval 43.9–109.7%; p < 0.001) increase in the adjusted odds of having received chemotherapy; no association was found between the TTO score and chemotherapy receipt.
Conclusions
A rank-order-based MCDA was feasible and was associated with chemotherapy choice. Future research should consider developing and testing this MCDA for use in clinical encounters. Additional research is required to develop a TTO-based model and test its properties against a pragmatic MCDA to inform future shared decision-making tools.



Similar content being viewed by others
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to Institutional Review Board protocol, but may be available from the corresponding author upon reasonable request.
References
Phelps C, Madhavan G. Using multicriteria approaches to assess the value of health care. Value Health. 2017;20(2):251–5.
Dolan JG, Fraenkel L. Shared decision-making. In: Marsh K, Goetghebeur M, Thokala P, Baltussen R, editors. Multi-criteria decision analysis to support healthcare decisions. Cham: Springer; 2017. p. 199–215.
Institutes of Medicine. Ranking vaccines a prioritization framework. Washington, DC: The National Academies Press; 2012.
Thokala P, Duenas A. Multiple criteria decision analysis for health technology assessment. Value Health. 2012;15(8):1172–81.
Maruthur NM, Joy SM, Dolan JG, Shihab HM, Singh S. Use of the analytic hierarchy process for medication decision-making in type 2 diabetes. PLoS One. 2015;10(5):e0126625.
Ijzerman MJ, Van Til JA, Bridges JF. A comparison of analytic hierarchy process and conjoint analysis methods in assessing treatment alternatives for stroke rehabilitation. Patient. 2012;5(1):45–56.
Dolan JG, Boohaker E, Allison J, Imperiale TF. Can streamlined multicriteria decision analysis be used to implement shared decision making for colorectal cancer screening? Med Decis Mak. 2014;34(6):746–55.
Ghabri S, Josselin J, Le Maux B. Could or should we use MCDA in the French HTA process? Pharmacoeconomics. 2019;37:1417–9.
Marsh KD, Sculpher M, Caro JJ, Tervonen T. The use of MCDA in HTA: great potential, but more effort needed. Value Health. 2018;21(4):394–7.
Marsh K, Lanitis T, Neasham D, Orfanos P, Caro J. Assessing the value of healthcare interventions using multi-criteria decision analysis: a review of the literature. Pharmacoeconomics. 2014;32(4):345–65.
Kujawski E, Triantaphyllou E, Yanase J. Additive multicriteria decision analysis models: misleading aids for life-critical shared decision making. Med Decis Mak. 2019;39(4):437–49.
Dombrovskiy VS, Omelyanovskiy V. Review of multicriteria decision analysis application for decision-making in oncology. Value Health. 2016;19(7):A751.
Simes RJ, Coates AS. Patient preferences for adjuvant chemotherapy of early breast cancer: how much benefit is needed? JNCI Monogr. 2001;30:146–52.
Duric VM, Stockler MR, Heritier S, Boyle F, Beith J, et al. Patients' preferences for adjuvant chemotherapy in early breast cancer: what makes AC and CMF worthwhile now? Ann Oncol. 2005;16(11):1786–94.
Mandelblatt JS, et al. Breast cancer adjuvant chemotherapy decisions in older women: the role of patient preference and interactions with physicians. J Clin Oncol. 2010;28(19):3146–53.
Sella T, Partridge AH. Clinical benefit in the treatment of patients with early breast cancer. Breast. 2019;48(Suppl 1):S115–S11818.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373(21):2005–144.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379(2):111–21.
Vromans R, Tenfelde K, Pauws S, et al. Assessing the quality and communicative aspects of patient decision aids for early-stage breast cancer treatment: a systematic review. Breast Cancer Res Treat. 2019;178(1):1–15.
Ankolekar A, Dekker A, Fijten R, Berlanga A. The benefits and challenges of using patient decision aids to support shared decision making in health care. JCO Clin Cancer Inform. 2018;2:1–10.
Lieu TA, Ray GT, Prausnitz SR, Habel LA, Alexeeff S, Li Y, et al. Oncologist and organizational factors associated with variation in breast cancer multigene testing. Breast Cancer Res Treat. 2017;163(1):167–76.
Ray GT, Mandelblatt J, Habel LA, Ramsey S, Kushi LH, Li Y, et al. Breast cancer multigene testing trends and impact on chemotherapy use. Am J Manag Care. 2016;22(5):e153–160.
Chandler Y, Schechter CB, Jayasekera J, Near A, O'Neill SC, Isaacs C, et al. Cost effectiveness of gene expression profile testing in community practice. J Clin Oncol. 2018;36(6):554–62.
Panattoni L, Lieu TA, Jayasekera J, O’Neill S, Mandelblatt JS, Etzioni R, et al. The impact of gene expression profile testing on confidence in chemotherapy decisions and prognostic expectations. Breast Cancer Res Treat. 2019;173(2):417–27.
Torrance GW, Thomas WH, Sackett DL. A utility maximization model for evaluation of health care programs. Health Serv Res. 1972;7(2):118.
Thokala P, Devlin N, Marsh K, Baltussen R, Boysen M, Kalo Z, et al. Multiple criteria decision analysis for health care decision making—an introduction: report 1 of the ISPOR MCDA Emerging Good Practices Task Force. Value Health. 2016;19(1):1–3.
Marsh K, Ijzerman M, Thokala P, Baltussen R, Boysen M, Kaló Z, et al. Multiple criteria decision analysis for health care decision making—emerging good practices: report 2 of the ISPOR MCDA Emerging Good Practices Task Force. Value Health. 2016;19(2):125–37.
Edwards W, Barron FH. SMARTS and SMARTER: improved simple methods for multiattribute utility measurement. Organ Behav Hum Decis Process. 1994;60(3):306–25.
Dolan JG. Multi-criteria clinical decision support: a primer on the use of multiple criteria decision making methods to promote evidence-based, patient-centered healthcare. Patient. 2010;3(4):229–48.
Barron FH, Barrett BE. Decision quality using ranked attribute weights. Manag Sci. 1996;42(11):1515–23.
Guerra RL, Castaneda L, de Albuquerque RD, Ferreira CB, de Miranda CF, Fernandes RR, et al. Patient preferences for breast cancer treatment interventions: a systematic review of discrete choice experiments. Patient. 2019;12(6):559–69. https://doi.org/10.1007/s40271-019-00375-w.
Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–31.
Attema AE, Edelaar-Peeters Y, Versteegh MM, Stolk EA. Time trade-off: one methodology, different methods. Eur J Health Econ. 2013;14(1):53–64.
Madhavan G, Phelps CE. Human factors in democracy. The Bridge (National Academy of Engineering). Winter. 2018;48(4):40–4.
Balinski M, Laraki R. Judge, Don’t Vote! Oper Res. 2014;62(3):483–511.
Madhavan G, Phelps CE, Rappuoli R. Compare voting systems to improve them. Nature. 2017;12(541):151–3.
Frey MK, Ellis A, Shyne S, Kahn R, Chapman-Davis E, Blank SV. Bridging the gap: a priorities assessment tool to support shared decision making, maximize appointment time, and increase patient satisfaction in women with ovarian cancer. J Oncol Pract. 2020;16(2):e148–e154154.
Acknowledgements
The authors are grateful to Tom Ray, MBA, Stephanie Prausnitz, MS, Pete Bogdanos, Laurel Habel, Ph.D., and Yan Li, MD, Ph.D., of Kaiser Permanente for their contributions to this project.
Author information
Authors and Affiliations
Contributions
LP, CP, and SR contributed to the conception and design of this work, data analysis and interpretation, and drafted the article; LP, TL, and SR contributed to the data collection; TL, SA, and SN contributed to manuscript writing; and JM contributed to the critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Laura Panattoni, Charles Phelps, Tracy A. Lieu, Stacey Alexeeff, Suzanne O’Neill, Jeanne Mandelblatt, and Scott D. Ramsey declare they have no conflicts of interest.
Funding
This research was supported by National Cancer Institute Grant #UO1 CA183081 (to JM, TL, and SR), And was also supported, in part, by Grant #U01 CA152958 from the National Cancer Institute, as part of the Cancer Intervention and Surveillance Modeling Network (CISNET), Grant #R35CA197289 (to JM) from the National Cancer Institute, and a supplement to Grant #UO1 CA183081 from the National Cancer Institute (SCO). The content is solely the responsibility of the authors and does not represent the official views of the National Cancer Institute at the National Institutes of Health.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Panattoni, L., Phelps, C.E., Lieu, T.A. et al. Feasibility of Measuring Preferences for Chemotherapy Among Early-Stage Breast Cancer Survivors Using a Direct Rank Ordering Multicriteria Decision Analysis Versus a Time Trade-Off. Patient 13, 557–566 (2020). https://doi.org/10.1007/s40271-020-00423-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-020-00423-w