Abstract
Study design
Retrospective cohort.
Objectives
To compare postoperative functional improvement in patients who underwent staged versus non-staged anterior–posterior spinal arthrodesis for adult spinal deformity (ASD).
Summary of background data
In patients with ASD, spinal arthrodesis can be performed in 2 stages to avoid the physiologic insult of a lengthy surgery. The association between staged surgery and postoperative functional improvement has not been well studied.
Methods
We included 87 patients (59 women) with ASD who underwent anterior–posterior spinal arthrodesis of > 5 levels with fixation to the pelvis from 2010–2014. Primary outcomes were the frequency of achieving at least a minimal clinically important difference (MCID) in the Scoliosis Research Society-22r (SRS-22r) Activity domain and the timeframe in which it was achieved. The secondary outcome was patient satisfaction (SRS-22r Patient Satisfaction domain). A Cox proportional hazard model was used to compare functional improvement over time between staged and non-staged groups. Our study was powered to detect a relative hazard ratio of 0.53, β = 0.20. α = 0.05.
Results
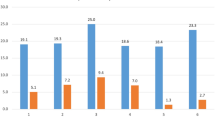
The frequency of achieving an MCID in SRS-22r Activity score did not differ significantly between the staged group (33/41 patients) and the non-staged group (34/46 patients) (hazard ratio 0.74; 95% confidence interval 0.41–1.36). Median times to achieving an MCID in SRS-22r Activity score were 191 days (interquartile range: 86–674) in the staged group and 181 days (interquartile range: 72–474) in the non-staged group (p = .75). The staged and non-staged groups had similar SRS-22r Patient Satisfaction scores at 3–9 months postoperatively and at final follow-up (both, p > .05).
Conclusion
Patients with ASD who underwent staged anterior–posterior spinal arthrodesis within 3 months after index surgery were similarly likely to experience functional improvement in the same timeframe as patients who underwent non-staged surgery. Patient satisfaction did not differ significantly between staged and non-staged groups.
Level of evidence
III.


Similar content being viewed by others
References
Pellisé F, Vila-Casademunt A, Ferrer M et al (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24:3–11
Daniels AH, DePasse JM, Eberson CP et al (2013) Adult spinal deformity: contemporary treatment and patient outcomes. R Island Med J 2015(98):32–41
Riley MS, Bridwell KH, Lenke LG et al (2018) Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine 28:194–200
Scheer JK, Smith JS, Clark AJ et al (2015) Comprehensive study of back and leg pain improvements after adult spinal deformity surgery: analysis of 421 patients with 2-year follow-up and of the impact of the surgery on treatment satisfaction. J Neurosurg Spine 22:540–553
Anand N, Kong C, Fessler RG (2017) A staged protocol for circumferential minimally invasive surgical correction of adult spinal deformity. Neurosurgery 81:733–739
Hassanzadeh H, Gjolaj JP, El Dafrawy MH et al (2013) The timing of surgical staging has a significant impact on the complications and functional outcomes of adult spinal deformity surgery. Spine J 13:1717–1722
Rhee JM, Bridwell KH, Lenke LG et al (2003) Staged posterior surgery for severe adult spinal deformity. Spine (Phila Pa 1976) 28:2116–2121
Passias PG, Poorman GW, Jalai CM et al (2017) Outcomes of open staged corrective surgery in the setting of adult spinal deformity. Spine J 17:1091–1099
Faloon MJ, Essig D, Cho W et al (2015) Unplanned reoperations affect long-term outcomes in adult spinal deformity patients undergoing long fusions to the sacrum. Spine Deform 3:367–371
Than KD, Park P, Tran S et al (2019) Analysis of complications with staged surgery for less invasive treatment of adult spinal deformity. World Neurosurg 126:e1337–e1342
Bridwell KH, Berven S, Glassman S et al (2007) Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine (Phila Pa 1976) 32:2220–2225
Bridwell KH, Cats-Baril W, Harrast J et al (2005) The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: a study of response distribution, concurrent validity, internal consistency, and reliability. Spine (Phila Pa 1976) 30:455–461
Fairbank JCT, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25:2940–2952 ((discussion 53))
Crawford CH III, Glassman SD, Bridwell KH et al (2015) The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 40:377–381
Gum JL, Lenke LG, Bumpass D et al (2016) Does planned staging for posterior-only vertebral column resections in spinal deformity surgery increase perioperative complications? Spine Deform 4:131–137
Choi YJ, Ra HJ (2016) Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res 28:1–15
Lyu H, Wick EC, Housman M et al (2013) Patient satisfaction as a possible indicator of quality surgical care. JAMA Surg 148:362–367
Tsai TC, Orav EJ, Jha AK (2015) Patient satisfaction and quality of surgical care in US hospitals. Ann Surg 261:2–8
Katayanagi J, Iida T, Hayamizu A et al (2019) Effect of long spinal fusion including the pelvis on activities of daily living related to lumbar spinal function in adults with spinal deformity. J Orthop Sci 24:409–414
Kyrölä K, Kautiainen H, Pekkanen L et al (2019) Long-term clinical and radiographic outcomes and patient satisfaction after adult spinal deformity correction. Scand J Surg 108:343–351
Sciubba DM, Scheer JK, Yurter A et al (2016) Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J 25:2433–2441
Liu S, Diebo BG, Henry JK et al (2016) The benefit of nonoperative treatment for adult spinal deformity: identifying predictors for reaching a minimal clinically important difference. Spine J 16:210–218
Scheer JK, Osorio JA, Smith JS et al (2018) Development of a preoperative predictive model for reaching the Oswestry Disability Index minimal clinically important difference for adult spinal deformity patients. Spine Deform 6:593–599
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
ABH, VP, MR: conception and design; acquisition and data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; supervision. MM: conception and design; analysis and interpretation of data; drafting of the manuscript; statistical analysis; supervision. MR: conception and design; drafting of the manuscript; critical revision of the manuscript for important intellectual content; supervision. RLS: conception and design; acquisition and data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; administration, technical, or material support; supervision. KMK: conception and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; administration, technical, or material support; supervision. BJN: conception and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; administration, technical, or material support; supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest with respect to the authorship and/or publication of this article.
Ethical approval
The study was approved by our institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harris, A.B., Puvanesarajah, V., Raad, M. et al. How is staging of ALIF following posterior spinal arthrodesis to the pelvis related to functional improvement in patients with adult spinal deformity?. Spine Deform 9, 1085–1091 (2021). https://doi.org/10.1007/s43390-020-00272-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00272-5