Abstract
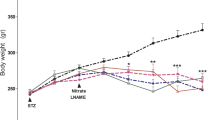
The present study aims to evaluate the effects of a dihydropyridine (DHP) derivative calcium channel antagonist nitrendipine (NIT) on lipid peroxidation (LPO), liver enzyme markers, glucose and lipid profile in rats with streptozotocin (STZ)-induced diabetes. A total of 24 female Sprague Dawley rats were classified into three groups as controls, STZ and STZ+NIT. Fasting blood glucose (FBG), triglyceride (TG), total cholesterol (TC) and high-density lipoprotein (HDL) levels, and alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activity were measured seven weeks after the administration of STZ and NIT. The levels of thiobarbituric acid substance (TBARS), glutathione (GSH) and total thiol content (T-SH), as well as the levels of nitric oxide and metabolites (NO, nitrate, nitrite), were evaluated to assess the level of lipid peroxidation in liver, brain, kidney, heart and eye tissues. STZ significantly increased FBG levels, ALT and AST activity, and TBARS levels (p < 0.001, for all), and significantly reduced the levels of GSH and T-SH (p < 0.05), as well as total NO and nitrate (p < 0.001). STZ triggered LPO in tissues, while simultaneously causing a marked decrease in endogenous antioxidant content. NIT administration protect the kidney (p < 0.05), heart (p < 0.01), brain (p < 0.001) and eye (p < 0.05) tissues from LPO, and also normalized the elevated FBG levels and the activity of ALT and AST (p < 0.001, for all). NIT further stimulated GSH and T-SH production, particularly in the liver, kidney and heart tissues. The results of the present study suggest that NIT shows hypoglycemic activity in STZ-DM rats by increasing insulin sensitivity in the peripheral target tissues.
Similar content being viewed by others
REFERENCES
Volpe, C.M.O., Villar-Delfino, P.H., Dos Anjos, P.M.F., and Nogueira-Machado, J.A., Cellular death, reactive oxygen species (ROS) and diabetic complications, Cell Death Dis., 2018, vol. 9, p. 119.
Mahjoub, S. and Masrour-Roudsari, J., Role of oxidative stress in pathogenesis of metabolic syndrome, Caspian J. Intern. Med., 2012, vol. 3, pp. 386–396.
Giacco, F. and Brownlee, M., Oxidative stress and diabetic complications, Circ. Res., 2010, vol. 107, pp. 1058–1070.
Gvazava, I.G., Rogovaya, O.S., Borisov, M.A., Vorotelyak, E.A., and Vasiliev, A.V., Pathogenesis of type 1 diabetes mellitus and rodent experimental models, Acta Naturae, 2018, vol. 10, pp. 24–33.
Derkach, K.V., Shpakova, E.A., Bondareva, V.M., and Shpakov, A.O., The effect of intranasal administration of proinsulin C-peptide and its C-terminal fragment on metabolic parameters in rats with streptozotocin diabetes, J. Evol. Biochem. Phys., 2018, vol. 54, pp. 242–245.
King, A.J., The use of animal models in diabetes research, Br. J. Pharmacol., 2012, vol. 166, pp. 877–894.
Nahdi, A.M.T.A., John, A., and Raza, H., Elucidation of molecular mechanisms of streptozotocin-induced oxidative stress, apoptosis, and mitochondrial dysfunction in Rin-5F pancreatic β-cells, Oxid. Med. Cell. Longev., 2017, vol. 2017, p. 7054272.
Raza, H. and John, A., Streptozotocin-induced cytotoxicity, oxidative stress and mitochondrial dysfunction in human hepatoma HepG2 cells, Int. J. Mol. Sci., 2012, vol. 13, pp. 5751–5767.
Singh, R., Bhardwaj, P., and Sharma, P., Antioxidant and toxicological evaluation of Cassia sopherain streptozotocin-induced diabetic Wistar rats, Pharmacognosy Res., 2013, vol. 5, pp. 225–232.
He, L., He, T., Farrar, S., Ji, L., Liu, T., and Ma, X., Antioxidants maintain cellular redox homeostasis by elimination of reactive oxygen species, Cell. Physiol. Biochem., 2017, vol. 44, pp. 532–553.
Aktay, G., Gursoy, S.O., Uyumlu, U., Unuvar, S., and Ilhan, N., Protective effect of atorvastatin on oxidative stress in streptozotocin-induced diabetic rats independently their lipid-lowering effects, J. Biochem. Mol. Toxicol., 2019, vol. 33, p. e22295.
Cominacini, L., Fratta Pasini, A., Garbin, U., Pastorino, A.M., Davoli, A., Nava, C., Campagnola, M., Rossato, P., and Lo Cascio, V., Antioxidant activity of different dihydropyridines, Biochem. Biophys. Res. Commun., 2003, vol. 302, pp. 679–684.
Salazar, T., Gonzalez, A., and Bandyopadhyay, D., Dihydropyridines as calcium channel blockers: An overview, J. Anal. Pharm. Res., 2017, vol. 5, p. 00148.
Guibert, C., Ducret, T., and Savineau, J.P., Voltage-independent calcium influx in smooth muscle, Prog. Biophys. Mol. Biol., 2008, vol. 98, pp. 10–23.
Chaudhry, R., Miao, J.H., and Rehman, A., Physiology, Cardiovascular, 2020 Mar 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2020
Haidara, M.A., Mikhailidis, D.P., Rateb, M.A., Ahmed, Z.A., Yassin, H.Z., Ibrahim, I.M., and Rashed, L.A., Evaluation of the effect of oxidative stress and vitamin E supplementation on renal function in rats with streptozotocin-induced Type 1 diabetes, J. Diabetes Complications, 2009, vol. 23, pp. 130–136.
Ohkawa, H., Ohishi, N., and Yagi, K., Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction, Anal. Biochem., 1979, vol. 95, pp. 351–358.
Jamall, I.S. and Smith, J.C., Effects of cadmium on glutathione peroxidase, superoxide dismutase and lipid peroxidation in the rat heart: A possible mechanism of cadmium cardiotoxicity, Toxicol. Appl. Pharmacol., 1985, vol. 80, pp. 33–42.
Sedlak, J. and Lindsay, R.H., Estimation of total protein-bound and nonprotein sulfhydryl groups in tissue with Ellman’s reagent, Anal. Biochem., 1968, vol. 25, pp. 192–205.
Gromova, L.V., Polozov, A.S., Kornyushin, O.V., Grefner, N.M., Dmitrieva, Y.V., Alekseeva, A.S., and Gruzdkov, A.A., Glucose absorption in the rat small intestine under experimental type 2 diabetes mellitus, J. Evol. Biochem. Phys., 2019, vol. 55, pp. 155–157.
Maritim, A.C., Sanders, R.A., and Watkins, J.B. III., Diabetes, oxidative stress, and antioxidants: a review, J. Biochem. Mol. Toxicol., 2003, vol. 17, pp. 24–38.
Matough, F.A., Budin, S.B., Hamid, Z.A., Alwahaibi, N., and Mohamed, J., The role of oxidative stress and antioxidants in diabetic complications, Sultan Qaboos Univ. Med. J., 2012, vol. 12, pp. 5–18.
Nopparat, J., Nualla-Ong, A., and Phongdara, A., Treatment with Pluchea indica (L.) Less. leaf ethanol extract alleviates liver injury in multiple low‑dose streptozotocin‑induced diabetic BALB/c mice, Exp. Ther. Med., 2020, vol. 20, pp. 1385–1396.
Köksal, B., Emre, M.H., and Polat, A., Investigation of propolis’ effect on thiobarbituric acid reactive substances and anti-oxidant enzyme levels of hippocampus in diabetic rats induced by streptozotocin, Open Access Maced. J. Med. Sci., 2015, vol. 3, pp. 52–56.
Milkovic, L., Vukovic, T., Zarkovic, N., Tatzber, F., Bisenieks, E., Kalme, Z., Bruvere, I., Ogle, Z., Poikans, J., Velena, A., and Duburs, G., Antioxidative 1,4-dihydropyridine derivatives modulate oxidative stress and growth of human osteoblast-like cells in vitro, Antioxidants (Basel), 2018, vol. 7, p. 123.
Liliany, S.B.A., Cláudia, S.S., and Rildo, A.V., Previous exercise training reduces markers of renal oxidative stress and inflammation in streptozotocin-induced diabetic female rats, J. Diabetes Res., 2018, vol. 2018, pp. 1–9.
Akila, G., Djamil, K., and Sadia, B., Portulaca oleracea leaf aqueous lyophilized extract reduces hyperglycemia and improves antioxidant status of red blood cells and liver in streptozotocin-induced diabetic Wistar rats, J. Pharmacy Pharmacol., 2017, vol. 5, pp. 139–148.
Aydın, M. and Celik, S., Effects of lycopene on plasma glucose, insulin levels, oxidative stress, and body weights of streptozotocin-induced diabetic rats, Turk. J. Med. Sci., 2014, vol. 42, pp. 1406–1413.
Sayed, A.A., Ferulsinaic acid modulates SOD, GSH, and antioxidant enzymes in diabetic kidney, Evid. Based Complement. Alternat. Med., 2012, vol. 2012, pp. 580104.
Shan, G., Yang, F., Zhou, L., Tang, T., Okoro, E.U., Yang, H., and Guo, Z., Increase in blood glutathione and erythrocyte proteins related to glutathione generation, reduction and utilization in African-American old women with diabetes, J. Sci. Technol. Environ., 2015, vol. 5, p. 3000251.
Espino, J., Pariente, J.A., and Rodríguez, A.B., Role of melatonin on diabetes-related metabolic disorders, World Journal of Diabetes, 2011, vol. 2, pp. 82–91.
Ebrahimi, Z., Khazaei, M.R., Ghanbari, E., and Khazaei, M., Renal tissue damages and its antioxidant status improved by Crab Shell extract in streptozotocin-induced diabetic rat, Adv. Biomed. Res., 2019, vol. 8, p. 41.
Khorsand, M., Akmali, M., and Akhzari, M., Efficacy of melatonin in restoring the antioxidant status in the lens of diabetic rats induced by streptozotocin, J. Diabetes Metab. Disord., 2019, vol. 18, pp. 543–549.
Espino, J., Pariente, J.A., and Rodríguez, A.B., Role of melatonin on diabetes-related metabolic disorders, World Journal of Diabetes, 2011, vol. 2, pp. 82–91.
Rivera, I., Cauvi, D., Arispe, N., and Maio, A.D., Nitrendipine, an antihypertensive alpha calcium channel blocker, is cytotoxic to neuroblastoma cells, Mol. Cell. Tox., 2019, vol. 15, pp. 469–475.
Derkach, K.V., Zorina, I.I., Zakharova, I.O., Basova, N.E., Bakhtyukov, A.A., and Shpakov, A.O., The influence of intranasally administered insulin and C-peptide on AMP-activated protein kinase activity, mitochondrial dynamics and apoptosis markers in the hypothalamus of rats with streptozotocin-induced diabetes, J. Evol. Biochem. Phys., 2020, vol. 56, pp. 207–217.
Funding
Supported by İnönü University Scientific Research Projects Department, project no. 2011/68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
All procedures for the care and use of animals were carried out in accordance with the requirements of the Inonu University Experimental Animals Ethics Committee (Ethics approval number; 2009/02). All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
СONFLICT OF INTEREST
No conflict of interest was declared.
Additional information
The original online version of this article was revised: the issue date is not January 2020, but January 2021
Rights and permissions
About this article
Cite this article
Ünüvar, S., Gürsoy, Ş., Berk, A. et al. Antioxidant Effect of a Dihydropyridine Calcium Antagonist Nitrendipine in Streptozotocin-Induced Diabetes. J Evol Biochem Phys 57, 126–133 (2021). https://doi.org/10.1134/S0022093021010129
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0022093021010129