Abstract
Purpose
Although cervical total disc replacement (CTDR) is perceived as a safe procedure, no review to date has quantified the complication rates. Of note, heterotopic ossification (HO), one of the complications of CTDR, is hypothesised to cause adjacent segment degeneration (ASDegeneration). This association has not been proven in meta-analysis. Hence, this systematic review and meta-analysis aims to investigate the pooled prevalence of complications following CTDR among studies that concomitantly reported the rate of HO, and the associations between HO and other complications, including ASDegeneration.
Methods
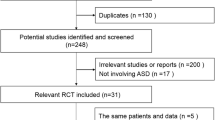
Literatures search was conducted in Embase, MEDLINE, PubMed, and the Cochrane Central Register of Controlled Trials. Complications were stratified into ≥ 1 and < 2 years, ≥ 2 and < 5 years, and ≥ 5 years follow-up. Subgroup and meta-regression analyses were performed.
Results
Fifty-three studies were included, composed of 3223 patients in total. The pooled prevalence of post-operative complications following CTDR was low, ranging from 0.8% in vascular adverse events to 4.7% in dysphagia at short-term follow-up. The rate of ASDegeneration was significantly higher at long-term follow-up (pooled prevalence 36.0%, 95% confidence interval [CI] 22.8–49.1%) than that at mid-term follow-up (pooled prevalence 7.3%, 95% CI 2.8–11.8%). Multivariate meta-regression analysis demonstrated that ASDegeneration was independently and inversely correlated with age (p = 0.007) and positively correlated with HO (p = 0.010) at mid-term follow-up. At long-term follow-up, ASDegeneration was still positively correlated with HO (p = 0.011), but not age. Furthermore, dysphagia was inversely associated with HO (p = 0.016), after adjustment for age and length of follow-up.
Conclusion
In conclusion, HO is associated with ASDegeneration and dysphagia.






Similar content being viewed by others
References
Delamarter RB, Zigler J (2013) Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine (Phila Pa 1976) 38(9):711–717
Chang U-K, Kim DH, Lee MC, Willenberg R, Kim S-H, Lim J (2007) Range of motion change after cervical arthroplasty with ProDisc-C and prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine 7(1):40–46
Shriver MF, Lubelski D, Sharma AM, Steinmetz MP, Benzel EC, Mroz TE (2016) Adjacent segment degeneration and disease following cervical arthroplasty: a systematic review and meta-analysis. Spine J 16(2):168–181
Yi S, Lee DY, Ahn PG, Kim KN, Shin HC (2009) Radiologically documented adjacent-segment degeneration after cervical arthroplasty: characteristics and review of cases. Surg Neurol 72(4):325–329
Hui N, Phan K, Kerferd J, Lee M, Mobbs RJ (2019) Prevalence of and risk factors for heterotopic ossification after cervical total disc replacement: a systematic review and meta-analysis. Glob Spine J. https://doi.org/10.1177/2192568219881163
McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J (2003) Classification of heterotopic ossification (HO) in artificial disk replacement. Clin Spine Surg 16(4):384–389
Ma Z, Ma X, Yang H, Guan X, Li X (2017) Anterior cervical discectomy and fusion versus cervical arthroplasty for the management of cervical spondylosis: a meta-analysis. Eur Spine J 26(4):998–1008
Latka D, Kozlowska K, Miekisiak G, Latka K, Chowaniec J, Olbrycht T, Latka M (2019) Safety and efficacy of cervical disc arthroplasty in preventing the adjacent segment disease: a meta-analysis of mid-to long-term outcomes in prospective, randomized, controlled multicenter studies. Ther Clin Risk Manag 15:531
Zeng J, Liu H, Chen H, Rong X, Meng Y, Yang Y, Deng Y, Ding C (2019) Effect of prosthesis width and depth on heterotopic ossification after cervical disc arthroplasty. Spine (Phila Pa 1976) 44(9):624–628
Phan K, Tian DH, Cao C, Black D, Yan TD (2015) Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg 4(2):112
Phan K, Mobbs RJ (2015) Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 1(1):19
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1
Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM (2006) Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 31(24):2802–2806
Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, Van Tulder MW (2015) 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976) 40(21):1660–1673
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Richards O, Choi D, Timothy J (2012) Cervical arthroplasty: the beginning, the middle, the end? Br J Neurosurg 26(1):2–6
Shriver MF, Lewis DJ, Kshettry VR, Rosenbaum BP, Benzel EC, Mroz TE (2017) Dysphagia rates after anterior cervical diskectomy and fusion: a systematic review and meta-analysis. Glob Spine J 7(1):95–103
Kelly MP, Eliasberg CD, Riley MS, Ajiboye RM, SooHoo NF (2018) Reoperation and complications after anterior cervical discectomy and fusion and cervical disc arthroplasty: a study of 52,395 cases. Eur Spine J 27(6):1432–1439
Zhu Y, Zhang B, Liu H, Wu Y, Zhu Q (2016) Cervical disc arthroplasty versus anterior cervical discectomy and fusion for incidence of symptomatic adjacent segment disease: a meta-analysis of prospective randomized controlled trials. Spine (Phila Pa 1976) 41(19):1493–1502
Zhong Z-M, Zhu S-Y, Zhuang J-S, Wu Q, Chen J-T (2016) Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis. Clin Orthop Relat Res 474(5):1307–1316
Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 34(2):101–107
Dmitriev AE, Kuklo TR, Lehman RA Jr, Rosner MK (2007) Stabilizing potential of anterior, posterior, and circumferential fixation for multilevel cervical arthrodesis: an in vitro human cadaveric study of the operative and adjacent segment kinematics. Spine (Phila Pa 1976) 32(6):E188–E196
Cunningham BW, Hu N, Zorn CM, McAfee PC (2010) Biomechanical comparison of single-and two-level cervical arthroplasty versus arthrodesis: effect on adjacent-level spinal kinematics. Spine J 10(4):341–349
Dejaegher J, Walraevens J, van Loon J, Van Calenbergh F, Demaerel P, Goffin J (2017) 10-year follow-up after implantation of the Bryan cervical disc prosthesis. Eur Spine J 26(4):1191–1198
Luo J, Gong M, Huang S, Yu T, Zou X (2015) Incidence of adjacent segment degeneration in cervical disc arthroplasty versus anterior cervical decompression and fusion meta-analysis of prospective studies. Arch Orthop Trauma Surg 135(2):155–160
Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y (2018) Cervical disc arthroplasty with Prestige-LP for the treatment of contiguous 2-level cervical degenerative disc disease: 5-year follow-up results. Medicine 97(4):e9671
Malham GM, Parker RM, Ellis NJ, Chan PG, Varma D (2014) Cervical artificial disc replacement with ProDisc-C: clinical and radiographic outcomes with long-term follow-up. J Clin Neurosci 21(6):949–953
Kim SH, Chung YS, Ropper AE, Min KH, Ahn TK, Won KS, Shin DA, Han IB (2015) Bone loss of the superior adjacent vertebral body immediately posterior to the anterior flange of Bryan cervical disc. Eur Spine J 24(12):2872–2879
Sun Y, Zhao Y, Pan S, Zhou F, Chen Z, Liu Z (2012) Comparison of adjacent segment degeneration five years after single level cervical fusion and cervical arthroplasty: a retrospective controlled study. Chin Med J 125(22):3939–3941
Zeng J, Liu H, Wang B, Deng Y, Ding C, Chen H, Yang Y, Hong Y, Ning N (2018) Clinical and radiographic comparison of cervical disc arthroplasty with Prestige-LP Disc and anterior cervical fusion: a minimum 6-year follow-up study. Clin Neurol Neurosurg 164:97–102
Lei T, Liu Y, Wang H, Xu J, Ma Q, Wang L, Shen Y (2016) Clinical and radiological analysis of Bryan cervical disc arthroplasty: eight-year follow-up results compared with anterior cervical discectomy and fusion. Int Orthop 40(6):1197–1203
Zhao Y, Zhang Y, Sun Y, Pan S, Zhou F, Liu Z (2016) Application of cervical arthroplasty with Bryan cervical disc: 10-year follow-up results in China. Spine (Phila Pa 1976) 41(2):111–115
Zhao Y, Sun Y, Zhou F, Liu Z (2013) Cervical disc arthroplasty with ProDisc-C artificial disc: 5-year radiographic follow-up results. Chin Med J (Engl) 126(20):3809–3811
Yi S, Shin DA, Kim KN, Choi G, Shin HC, Kim KS (2013) The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J 13(9):1048–1054
Chung S-B, Muradov JM, Lee S-H, Eoh W, Kim E-S (2012) Uncovertebral hypertrophy is a significant risk factor for the occurrence of heterotopic ossification after cervical disc replacement: survivorship analysis of Bryan disc for single-level cervical arthroplasty. Acta Neurochir (Wien) 154(6):1017–1022
Hui N, Phan K, Kerferd J, Lee M, Mobbs RJ (2020) Cervical total disc replacement and heterotopic ossification: a review of literature outcomes and biomechanics. Asian Spine J. https://doi.org/10.31616/asj.2019.0234
Anderson KK, Arnold PM (2013) Oropharyngeal dysphagia after anterior cervical spine surgery: a review. Glob Spine J 3(04):273–286
Olmsted-Davis EA, Salisbury EA, Hoang D, Davis EL, Lazard Z, Sonnet C, Davis TA, Forsberg JA, Davis AR (2017) Progenitors in peripheral nerves launch heterotopic ossification. Stem Cells Transl Med 6(4):1109–1119
Chang U-K, Kim DH, Lee MC, Willenberg R, Kim S-H, Lim J (2007) Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg 7:33–39
Xu S, Liang Y, Meng F, Wang K, Liu H (2019) Radiological exploration on adjacent segments after total cervical disc replacement with Prodisc-C prosthesis. J Orthop Surg Res 14(1):160
Li G, Wang Q, Liu H, Yang Y (2019) Postoperative heterotopic ossification after cervical disc replacement is likely a reflection of the degeneration process. World Neurosurg 125:e1063–e1068
Zhou F, Ju KL, Zhao Y, Zhang F, Pan S, Heller JG, Sun Y (2018) Progressive bone formation after cervical disc replacement. Spine (Phila Pa 1976) 43(3):E163–E170
Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE (2013) What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT. Eur Spine J 22(5):1078–1089
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976) 26(22):2463–2466
Hashimoto K, Aizawa T, Kanno H, Itoi E (2019) Adjacent segment degeneration after fusion spinal surgery—a systematic review. Int Orthop 43(4):987–993
Yang B, Li H, Zhang T, He X, Xu S (2012) The incidence of adjacent segment degeneration after cervical disc arthroplasty (CDA): a meta analysis of randomized controlled trials. PLoS ONE 7(4):e35032
Park WM, Kim K, Kim YH (2015) Changes in range of motion, intradiscal pressure, and facet joint force after intervertebral disc and facet joint degeneration in the cervical spine. J Mech Sci Technol 29(7):3031–3038
Ren D, Hu Z, Yuan W (2016) The study of cobb angular velocity in cervical spine during dynamic extension–flexion. Spine (Phila Pa 1976) 41(7):E410–E415
Shi S, Zheng S, Li X-F, Yang L-L, Liu Z-D, Yuan W (2016) Comparison of 2 zero-profile implants in the treatment of single-level cervical spondylotic myelopathy: a preliminary clinical study of cervical disc arthroplasty versus fusion. PLoS ONE 11(7):e0159761
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hui, N., Phan, K., Cheng, H.M.K. et al. Complications of cervical total disc replacement and their associations with heterotopic ossification: a systematic review and meta-analysis. Eur Spine J 29, 2688–2700 (2020). https://doi.org/10.1007/s00586-020-06400-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06400-z