Abstract
Purpose
Poor sleep and mood may be predisposing factors for acne. We aimed to investigate the associations between acne and sleep quality, circadian preferences, and mood.
Methods
This case–control study recruited patients with acne and age- and sex-matched healthy controls. We used the Investigator’s Global Assessment to evaluate acne severity and various validated questionnaires to measure sleep quality, daytime sleepiness, sleep apnea, circadian preference, and mood symptoms.
Results
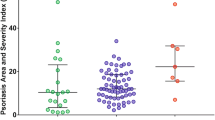
A total of 81 patients with acne (age: 21.6 ± 5.0 years, 52% female) and 76 controls were recruited. Compared to controls, patients had a higher score on the Pittsburgh Sleep Quality Index (5.2 ± 2.6 vs. 4.1 ± 2.3, p = 0.008) and State–Trait Anxiety Inventory (State: 44.6 ± 9.7 vs. 40.6 ± 6.6, p = 0.003; Trait: 47.9 ± 8.2 vs. 45.3 ± 6.2, p = 0.03), and a lower score on a reduced version of the Morningness and Eveningness Questionnaire (13.9 ± 2.6 vs. 14.7 ± 2.3, p = 0.05) and Epworth Sleepiness Scale (7.4 ± 3.4 vs. 8.6 ± 3.6, p = 0.04). Acne severity was associated with sleep quality (β = 0.33), eveningness (β = 0.34), depression (β = 0.66), and anxiety (State: β = 1.73; Trait: β = 1.21), even when adjusted for education level and family history of acne.
Conclusion
Acne is highly associated with poor sleep and mood. Dermatologists are advised to attend closely to the psychological impact of acne. Improvements in sleep and mood may benefit the treatment of acne.
Similar content being viewed by others
Data Availability
The data of this study can be requested from the Department of Dermatology, Chengdu Medical College, via the corresponding author.
Data Availability
The data of this study can be requested from the Department of Dermatology, Chengdu Medical College, via the corresponding author.
References
Williams HC, Dellavalle RP, Garner S (2012) Acne vulgaris. Lancet 379:361–372. https://doi.org/10.1016/S0140-6736(11)60321-8
Schafer T, Nienhaus A, Vieluf D, Berger J, Ring J (2001) Epidemiology of acne in the general population: the risk of smoking. Br J Dermatol 145:100–104. https://doi.org/10.1046/j.1365-2133.2001.04290.x
Wu TQ, Mei SQ, Zhang JX et al (2007) Prevalence and risk factors of facial acne vulgaris among Chinese adolescents. Int J Adolesc Med Health 19:407–412. https://doi.org/10.1515/ijamh.2007.19.4.407
Jafferany M (2007) Psychodermatology: a guide to understanding common psychocutaneous disorders. Prim Care Companion J Clin Psychiatry 9:203–213. https://doi.org/10.4088/pcc.v09n0306
Hu T, Wei Z, Ju Q, Chen W (2021) Sex hormones and acne: state of the art. J Dtsch Dermatol Ges 19:509–515. https://doi.org/10.1111/ddg.14426
Lucky AW, Biro FM, Huster GA, Leach AD, Morrison JA, Ratterman J (1994) Acne vulgaris in premenarchal girls. An early sign of puberty associated with rising levels of dehydroepiandrosterone. Arch Dermatol 130:308–314. https://doi.org/10.1001/archderm.130.3.308
Arakaki FH, Xerfan EMS, Tufik S, Andersen ML (2020) Acne in men due to protein supplementation: how sleep could be related? Sleep Med 75:7–7. https://doi.org/10.1016/j.sleep.2020.06.007
Xerfan EMS, Facina AS, Andersen ML, Tufik S, Tomimori J (2021) Acne flare-up due to mask wearing: a current pandemic scenario and its relationship with sleep. Skin Res Technol 27:1002–1003. https://doi.org/10.1111/srt.13048
Kubota Y, Shirahige Y, Nakai K, Katsuura J, Moriue T, Yoneda K (2010) Community-based epidemiological study of psychosocial effects of acne in Japanese adolescents. J Dermatol 37:617–622. https://doi.org/10.1111/j.1346-8138.2010.00855.x
Misery L, Wolkenstein P, Amici JM et al (2015) Consequences of acne on stress, fatigue, sleep disorders and sexual activity: a population-based study. Acta Derm Venereol 95:485–488. https://doi.org/10.2340/00015555-1998
Chaudhary S, Ameer A, Sarwar MZ, Naqi SA, Butt AI (2021) A cross-sectional study of body mass index and sleep quality as risk factors to severity of acne. J Pak Med Assoc 71:2148–2150. https://doi.org/10.47391/JPMA.404
Alsulaimani H, Kokandi A, Khawandanh S, Hamad R (2020) Severity of acne vulgaris: comparison of two assessment methods. Clin Cosmet Investig Dermatol 13:711–716. https://doi.org/10.2147/CCID.S266320
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Adan A, Almirall H (1991) Horne & Östberg morningness-eveningness questionnaire: a reduced scale. Pers Individ Dif 12:241–253. https://doi.org/10.1016/0191-8869(91)90110-W
Carciofo R, Du F, Song N, Qi Y, Zhang K (2012) Age-related chronotype differences in Chinese, and reliability assessment of a reduced version of the Chinese Morningness-Eveningness Questionnaire. Sleep Biol Rhythms 10:310–318. https://doi.org/10.1111/j.1479-8425.2012.00577.x
Chung F, Yegneswaran B, Liao P et al (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108:812–821. https://doi.org/10.1097/ALN.0b013e31816d83e4
Beck AT, Erbaugh J, Ward CH, Mock J, Mendelsohn M (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004
Spielberger C, Gorsuch R, Lushene R, Vagg PR, Jacobs G (1983) Manual for the state-trait anxiety inventory (form Y1–Y2). Consulting Psychologists Press
Julian LJ (2011) Measures of anxiety: State-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11):S467–S472. https://doi.org/10.1002/acr.20561
Wei B, Pang Y, Zhu H et al (2010) The epidemiology of adolescent acne in North East China. J Eur Acad Dermatol Venereol 24:953–957. https://doi.org/10.1111/j.1468-3083.2010.03590.x
Suh DH, Kim BY, Min SU et al (2011) A multicenter epidemiological study of acne vulgaris in Korea. Int J Dermatol 50:673–681. https://doi.org/10.1111/j.1365-4632.2010.04726.x
Morssinkhof MWL, van Wylick DW, Priester-Vink S et al (2020) Associations between sex hormones, sleep problems and depression: a systematic review. Neurosci Biobehav Rev 118:669–680. https://doi.org/10.1016/j.neubiorev.2020.08.006
Lord C, Sekerovic Z, Carrier J (2014) Sleep regulation and sex hormones exposure in men and women across adulthood. Pathol Biol (Paris) 62:302–310. https://doi.org/10.1016/j.patbio.2014.07.005
Oh DY, Park SM, Choi SW (2020) Daytime neurophysiological hyperarousal in chronic insomnia: a study of qEEG. J Clin Med 9(11):3425. https://doi.org/10.3390/jcm9113425
Kim JE, Cho BK, Cho DH, Park HJ (2013) Expression of hypothalamic-pituitary-adrenal axis in common skin diseases: evidence of its association with stress-related disease activity. Acta Derm Venereol 93:387–393. https://doi.org/10.2340/00015555-1557
Tasoula E, Gregoriou S, Chalikias J et al (2012) The impact of acne vulgaris on quality of life and psychic health in young adolescents in Greece. Results of a population survey. An Bras Dermatol 87:862–869. https://doi.org/10.1590/s0365-05962012000600007
Acknowledgements
The authors would like to thank the participants for their participation and cooperation.
Funding
This work was supported by grants from the Medical Research Project of Sichuan Province (No. S20003), the Special Research Fund (No. CYFY2019ZD05), and the Liyan Workshop Medical Beauty Research Center Special Project (20YM001) from the First Affiliated Hospital of Chengdu Medical College. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Chengdu Medical College. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, J., Peng, K., Zhang, Y. et al. Sleep quality, circadian preferences, and mood among patients with acne vulgaris: a case–control study. Sleep Breath 27, 1997–2003 (2023). https://doi.org/10.1007/s11325-023-02777-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02777-5