Abstract
Objective: It has been reported that being part of a minority group may be negatively associated with self-perceived health. The objective of this analysis was to determine whether there are differences in perceived health between the Francophone minority and Anglophone majority in New Brunswick, the only officially bilingual province in Canada.
Methods: Data from the first four primary cycles of the Canadian Community Health Survey (2001 to 2007) were obtained for 17,729 New Brunswick residents. Odds of reporting good health among Francophones and Anglophones were compared using multivariate logistic regressions accounting for age, health-related behaviours, socio-demographic variables, and medical conditions.
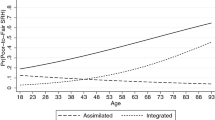
Results: In the final models, Francophone men and women were less likely than Anglophones to report their health as being good, although these differences were not statistically significant (Odds ratio, 95% confidence interval: 0.88, 0.61–1.26; 0.71, 0.49-1.04, in men and women, respectively).
Conclusion: This study suggests that being part of the linguistic minority in New Brunswick is not associated with statistically significant differences in self-perceived health.
Résumé
Objectif: Faire partie d’un groupe minoritaire peut être lié à une moins bonne santé perçue. L’objectif de cette analyse est de déterminer s’il existe des différences au niveau de la santé perçue entre la minorité francophone et la majorité anglophone du Nouveau-Brunswick, la seule province officiellement bilingue au Canada.
Méthodes: Les données des quatre premiers cycles de l’Enquête sur la santé dans les collectivités canadiennes (2001 à 2007) ont été obtenues pour 17 729 résidents du Nouveau-Brunswick. Les chances de rapporter une bonne santé chez les francophones et les anglophones ont été comparées en utilisant des rapports de côtes prenant en considération les variables âge, comportements liés à la santé, facteurs sociodémographiques, et conditions médicales.
Résultats: Dans les modèles finaux, les hommes et femmes francophones étaient moins enclins que les anglophones à rapporter une bonne santé, mais ces différences n’étaient pas statistiquement significatives (rapport de côtes, intervalle de confiance à 95 %: 0,88, 0,61–1,26; 0,71, 0,49–1,04, chez les hommes et les femmes, respectivement).
Conclusion: Cette étude suggère que le statut de francophone en situation minoritaire au Nouveau-Brunswick n’est pas lié à une différence statistiquement significative de la santé perçue.
Similar content being viewed by others
References
Commission on Social Determinants of Health. Final Report: Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva, Switzerland: World Health Organization, 2008.
Marmot M. Social determinants of health inequalities. Lancet 2005;365(9464):1099–104.
Tarlov, AR. Public policy frameworks for improving population health. Ann N Y Acad Sci 1999;896:281–93.
Kawachi I. Social capital and community effects on population and individual health. Ann N Y Acad Sci 1999;896:120–30.
Willams DR, Collins C. US socioeconomic and racial differences in health: Patterns and explanations. Annu Rev Sociol 1995;21:349–86.
Davey Smith G, Neaton JD, Wentworth D, Stamler R, Stamler J. Mortality differences between black and white men in the USA: Contribution of income and other risk factors among men screened for the MRFIT. MRFIT Research Group. Multiple Risk Factor Intervention Trial. Lancet 1998;351(9107):934–39.
Australian Bureau of Statistics/Australian Institute of Health and Welfare. The Health and Welfare of Australian’s Aboriginal and Torres Strait Islander Peoples. Commonwealth of Australia: The Australian Government, 2008.
Kobayashi KM, Prus S, Lin Z. Ethnic differences in self-rated and functional health: Does immigrant status matter? Ethn Health 2008;13(2):129–47.
Kopec JA, Williams JI, To T, Austin, PC. Cross-cultural comparisons of health status in Canada using the Health Utilities Index. Ethn Health 2001;6(1):41–50.
Bouchard L, Gaboury I, Chomienne M-H, Gilbert A, Dubois L. La santé en situation linguistique minoritaire. Healthcare Policy 2009;4(4):33–40.
Bouchard L, Gilbert A, Landry R, Deveau K. Social capital, health, and Francophone minorities. Can J Public Health 2006;97(Suppl 2):S16–S20.
Institut Franco-Ontarien/Programme de recherche, d’éducation et de développement en santé publique. Deuxième rapport sur la santé des francophones de l’Ontario. Ontario: Office of Francophone Affairs, 2005.
Desjardins L. La santé des francophones du Nouveau-Brunswick. Les Éditions de la Francophonie. 2003;258.
Robichaud J-B. La santé des francophones. Objectif 2000, Vol. 1. Moncton, Nouveau-Brunswick: Éditions Acadie, 1985;189.
Thomas S, Wannell B. Combining cycles of the Canadian Community Health Survey. Health Report (Statistics Canada, Catalogue 82-003-X) 2009;20(1):53–58.
Bouchard L, Gaboury I, Dubois L, Gilbert A, Chomienne MH, Beauregard N, Berthelot, JM. Disparités de santé et francophonie minoritaire. 96e Conférence annuelle de l’Association canadienne de santé publique, Ottawa, 2005.
Idler EL, Benyamini Y. Self-rated health and mortality: A review of twentyseven community studies. J Health Soc Behav 1997;38(1):21–37.
Rao JNK, Wu CFJ, Yue K. Some recent work on resampling methods for complex surveys. Survey Methodology (Statistics Canada, Catalogue 12-001) 1992;18(2):209–17.
Shetterly SM, Baxter J, Mason LD, Hamman, RF. Self-rated health among Hispanic vs. non-Hispanic white adults: The San Luis Valley Health and Aging Study. Am J Public Health 1996;86(12):1798–801.
Spencer SM, Schulz R, Rooks RN, Albert SM, Thorpe RJ Jr, Brenes GA, et al. Racial differences in self-rated health at similar levels of physical functioning: An examination of health pessimism in the health, aging, and body composition study. J Gerontol B Psychol Sci Soc Sci 2009;64(1):87–94.
Bailis DS, Segall A, Chipperfield, JG. Two views of self-rated general health status. Soc Sci Med 2003;56(2):203–17.
Quesnel-Vallée A. Self-rated health: Caught in the crossfire of the quest for “true” health. Int J Epidemiol 2007;36(6):1161–64.
Commission on the Future of Healthcare in Canada. Building on values: The Future of Health Care in Canada, Final Report. Ottawa, ON: Health Canada, 2002.
Bowen S. Language Barriers in Access to Health Care/Barrières linguistiques dans l’accès aux soins de santé. Minister of Public Works and Government Services, Health Canada, 2001.
Schofield A, Bourgeois D. Socially responsible medical education: Innovations and challenges in a minority setting. Med Educ 2010;44(3):263–71.
Nyqvist F, Finnäs F, Jakobsson G, Koskinen S. The effect of social capital on health: The case of two language groups in Finland. Health Place 2008;14(2):347–60.
Komar M, Nagymajtényi L, Nyari T, Paulik E. The determinants of self-rated health among ethnic minorities in Hungary. Ethn Health 2006;11(2):121–32.
Marmot M. Status Syndrome. London, UK: Bloomsbury Publishing, 2004;288.
Wilkinson, RG. Health, hierarchy and social anxiety. Ann N Y Acad Sci 1999;896:48–63.
St-Pierre M, Béland Y. Mode Effects in the Canadian Community Health Survey: A Comparison of CAPI and CATI. Proceedings of the Annual Meeting of the American Statistical Association, Survey Research Methods Section, American Statistical Association, 2004.
Author information
Authors and Affiliations
Corresponding author
Additional information
Acknowledgement of support: The analyses were performed in the context of research programs funded by the Canadian Institutes of Health Research (Bouchard et al. Les déterminants de la santé des minorités francophones une analyse secondaire de l’ESCC) and the Consortium national de formation en santé, volet Université de Moncton (Bourque et al.).
Conflict of Interest: None to declare.
Rights and permissions
About this article
Cite this article
Bélanger, M., Bouchard, L., Gaboury, I. et al. Perceived Health Status of Francophones and Anglophones in an Officially Bilingual Canadian Province. Can J Public Health 102, 122–126 (2011). https://doi.org/10.1007/BF03404160
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03404160