Abstract
Objective
Previous studies demonstrated that prophylactic cranial irradiation (PCI) significantly reduced the incidence of brain metastases in patients with extensive disease small cell lung cancer (ED-SCLC). However, the appropriate timing for PCI in treating ED-SCLC is still unclear. This study aimed to compare the effect and safety of early versus late PCI.
Methods
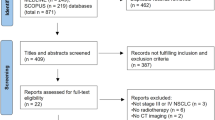
Between November 2011 and July 2016, 103 patients with ED-SCLC were reviewed, receiving appropriate imaging tests to exclude brain metastases prior to cranial irradiation. Of these 103 patients, early PCI was performed in 47 patients and the other 56 patients received late PCI. The primary endpoint was the incidence of brain metastases. The progression-free survival (PFS), overall survival (OS), and adverse events (AEs) were also assessed.
Results
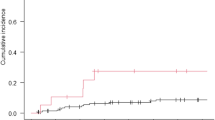
Early PCI significantly lowered the risk of brain metastases, as compared to late PCI (p = 0.024). Additionally, multivariate analyses demonstrated that early PCI was a favorable independent predictor of the incidence of brain metastases. The PFS and OS of patients in the early and late PCI groups were comparable (PFS: 8.4 months vs. 7.5 months, p = 0.234; OS: 16.1 months vs. 15.2 months, p = 0.753). The AEs were generally acceptable in both groups.
Conclusion
To reduce the incidence of brain metastases, early PCI is more effective than late PCI for ED-SCLC patients.
Zusammenfassung
Zusammenfassung
In früheren Studien wurde gezeigt, dass eine prophylaktische Ganzhirnbestrahlung („prophylactic cranial irradiation“, PCI) die Häufigkeit zerebraler Metastasen im Gehirn bei Patienten mit metastasiertem kleinzelligem Lungenkarzinom („extensive disease small cell lung cancer“, ED-SCLC) signifikant reduzieren kann. Der richtige Zeitpunkt einer PCI bei ED-SCLC ist unklar. Ziel dieser Studie ist es, die Wirkung und Sicherheit von früher vs. später PCI zu vergleichen.
Methode
Zwischen November 2011 und Juli 2016 wurden 103 Patienten mit ED-SCLC untersucht. Mittels schnittbildgebender Untersuchung wurden Hirnmetastasen vor der Ganzhirnbestrahlung ausgeschlossen. Bei 47 Patienten wurde eine frühe PCI durchgeführt, bei den anderen 56 Patienten eine späte PCI. Primärer Endpunkt war das Auftreten von Hirnmetastasen. Das progressionsfreie Überleben („progression-free survival“, PFS), Gesamtüberleben („overall survival“, OS) und unerwünschte Ereignisse („adverse events“, AE) wurden ebenfalls ausgewertet.
Ergebnisse
Eine frühe PCI senkt das Risiko für Hirnmetastasen im Vergleich zur späten PCI (p = 0,024). Zusätzlich zeigen multivariate Analysen, dass eine frühe PCI ein unabhängiger Prädiktor für das seltenere Auftreten von zerebralen Filiae war. PFS und OS waren bei Patienten mit früher und später PCI vergleichbar (PFS: 8,4 vs. 7,5 Monate; p = 0,234; OS: 16,1 vs. 15,2 Monate; p = 0,753). Die AE waren in beiden Gruppen tolerabel.
Schlussfolgerung
Um die Auftretenswahrscheinlichkeit von Metastasen im Gehirn zu reduzieren, ist eine frühe PCI effektiver als eine späte PCI bei Patienten mit ED-SCLC.



Similar content being viewed by others
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Govindan R, Page N, Morgensztern D, Read W, Tierney R, Vlahiotis A, Spitznagel EL, Piccirillo J (2006) Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 24:4539–4544
Feld R, Pringle JF, Evans WK, Keen CW, Quirt IC, Curtis JE, Baker MA, Yeoh JL, Deboer G, Brown TC (1981) Combined modality treatment of small cell carcinoma of the lung. Arch Intern Med 141:469–473
Oberg K, Hellman P, Ferolla P, Papotti M (2012) Neuroendocrine bronchial and thymic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 23(Suppl 7):i120–i123
Simon M, Argiris A, Murren JR (2004) Progress in the therapy of small cell lung cancer. Crit Rev Oncol Hematol 49:119–133
Chua YJ, Steer C, Yip D (2004) Recent advances in management of small-cell lung cancer. Cancer Treat Rev 30:521–543
Kurup A, Hanna NH (2004) Treatment of small cell lung cancer. Crit Rev Oncol Hematol 52:117–126
Schnabel T, Schmitt G (1993) The role of radiotherapy in the management of small cell lung cancer (SCLC). Strahlenther Onkol 169:329–338
Socinski MA, Bogart JA (2007) Limited-stage small-cell lung cancer: the current status of combined-modality therapy. J Clin Oncol 25:4137–4145
Stupp R, Monnerat C, Turrisi AR, Perry MC, Leyvraz S (2004) Small cell lung cancer: state of the art and future perspectives. Lung Cancer 45:105–117
Seute T, Leffers P, Ten VG, Twijnstra A (2004) Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer 100:801–806
Komaki R, Cox JD, Whitson W (1981) Risk of brain metastasis from small cell carcinoma of the lung related to length of survival and prophylactic irradiation. Cancer Treat Rep 65:811–814
Hardy J, Smith I, Cherryman G, Vincent M, Judson I, Perren T, Williams M (1990) The value of computed tomographic (CT) scan surveillance in the detection and management of brain metastases in patients with small cell lung cancer. Br J Cancer 62:684–686
Arriagada R, Le Chevalier T, Borie F, Riviere A, Chomy P, Monnet I, Tardivon A, Viader F, Tarayre M, Benhamou S (1995) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. J Natl Cancer Inst 87:183–190
Auperin A, Arriagada R, Pignon JP, Le Pechoux C, Gregor A, Stephens RJ, Kristjansen PE, Johnson BE, Ueoka H, Wagner H, Aisner J (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med 341:476–484
Bernhardt D, Adeberg S, Bozorgmehr F, Opfermann N, Hoerner-Rieber J, Repka MC, Kappes J, Thomas M, Bischoff H, Herth F, Heussel CP, Debus J, Steins M, Rieken S (2017) Nine-year experience: prophylactic cranial irradiation in extensive disease small-cell lung cancer. Clin Lung Cancer 18:e267–e271
Chen Y, Li J, Hu Y, Zhang Y, Lin Z, Zhao Z, Jiao S (2016) Prophylactic cranial irradiation could improve overall survival in patients with extensive small cell lung cancer: a retrospective study. Strahlenther Onkol 192:905–912
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, Postmus P, Collette L, Musat E, Senan S (2007) Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357:664–672
Takahashi T, Yamanaka T, Seto T, Harada H, Nokihara H, Saka H, Nishio M, Kaneda H, Takayama K, Ishimoto O, Takeda K, Yoshioka H, Tachihara M, Sakai H, Goto K, Yamamoto N (2017) Prophylactic cranial irradiation versus observation in patients with extensive-disease small-cell lung cancer: a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 18:663–671
National Cancer Institute (2006) Common Terminology Criteria for Adverse Events (CTCAE) version 3.0. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed 7 June 2017
Windsor AA, Koh ES, Allen S, Gabriel GS, Yeo AE, Allison R, van der Linden YM, Barton MB (2013) Poor outcomes after whole brain radiotherapy in patients with brain metastases: results from an international multicentre cohort study. Clin Oncol (R Coll Radiol) 25:674–680
Farooqi AS, Holliday EB, Allen PK, Wei X, Cox JD, Komaki R (2017) Prophylactic cranial irradiation after definitive chemoradiotherapy for limited-stage small cell lung cancer: Do all patients benefit? Radiother Oncol 122:307–312
Slotman BJ (2015) Prophylactic cranial irradiation postchemotherapy response. J Thorac Oncol 10(suppl 2):S171 (abstract)
Fruh M, De Ruysscher D, Popat S, Crino L, Peters S, Felip E (2013) Small-Cell Lung Cancer (SCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl 6):i99–i105
Suwinski R, Lee SP, Withers HR (1998) Dose-response relationship for prophylactic cranial irradiation in small cell lung cancer. Int J Radiat Oncol Biol Phys 40:797–806
Suwinski R, Withers HR (2003) Time factor and treatment strategies in subclinical disease. Int J Radiat Biol 79:495–502
Sas-Korczynska B, Korzeniowski S, Wojcik E (2010) Comparison of the effectiveness of “late” and “early” prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Strahlenther Onkol 186:315–319
Ramlov A, Tietze A, Khalil AA, Knap MM (2012) Prophylactic cranial irradiation in patients with small cell lung cancer. A retrospective study of recurrence, survival and morbidity. Lung Cancer 77:561–566
Grosshans DR, Meyers CA, Allen PK, Davenport SD, Komaki R (2008) Neurocognitive function in patients with small cell lung cancer: effect of prophylactic cranial irradiation. Cancer 112:589–595
Welzel T, Niethammer A, Mende U, Heiland S, Wenz F, Debus J, Krempien R (2008) Diffusion tensor imaging screening of radiation-induced changes in the white matter after prophylactic cranial irradiation of patients with small cell lung cancer: first results of a prospective study. AJNR Am J Neuroradiol 29:379–383
Wolfson AH, Bae K, Komaki R, Meyers C, Movsas B, Le Pechoux C, Werner-Wasik M, Videtic GM, Garces YI, Choy H (2011) Primary analysis of a phase II randomized trial Radiation Therapy Oncology Group (RTOG) 0212: impact of different total doses and schedules of prophylactic cranial irradiation on chronic neurotoxicity and quality of life for patients with limited-disease small-cell lung cancer. Int J Radiat Oncol Biol Phys 81:77–84
Acknowledgements
This work was jointly supported by National Natural Science Foundation of China (Grants No. 11505012), Beijing Natural Science Foundation (Grants No. 7172048, 1174016 and 1184014), and Capital’s Funds for Health Improvement and Research (2018-4-1027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Chen, J. Li, Y. Zhang, Y. Hu, G. Zhang, X. Yan, Z. Lin, Z. Zhao, and S. Jiao declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Chen, Y., Li, J., Zhang, Y. et al. Early versus late prophylactic cranial irradiation in patients with extensive small cell lung cancer. Strahlenther Onkol 194, 876–885 (2018). https://doi.org/10.1007/s00066-018-1307-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1307-1