Abstract
Purpose
The primary aim was to determine whether a shock index (SI) ≥ 1 in adult trauma patients was associated with increased in-hospital mortality compared to an SI < 1.
Methods
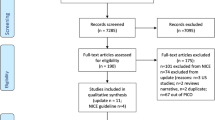
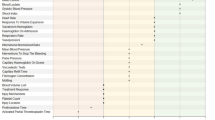
This systematic review including a meta-analysis was performed in accordance with the PRISMA guidelines. EMBASE, MEDLINE, and Cochrane Library were searched, and two authors independently screened articles, performed the data extraction, and assessed risk of bias. Studies were included if they reported in-hospital, 30-day, or 48-h mortality, length of stay, massive blood transfusion or ICU admission in trauma patients with SI recorded at arrival in the emergency department or trauma center. Risk of bias was assessed using the Newcastle–Ottawa Scale, and the strength and quality of the body of evidence according to GRADE. Data were pooled using a random effects model. Inter-rater reliability was assessed with Cohen’s kappa.
Results
We screened 1350 citations with an inter-rater reliability of 0.90. Thirty-eight cohort studies were included of which 14 reported the primary outcome. All studies reported a significant higher in-hospital mortality in adult trauma patients with an SI ≥ 1 compared to those having an SI < 1. Twelve studies involving a total of 348,687 participants were included in the meta-analysis. The pooled risk ratio (RR) of in-hospital mortality was 4.15 (95% CI 2.96–5.83). The overall quality of evidence was low.
Conclusions
This systematic review found a fourfold increased risk of in-hospital mortality in adult trauma patients with an initial SI ≥ 1 in the emergency department or trauma center.


Similar content being viewed by others
References
Geneva WHO. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. 2018.
Sobrino J, Shafi S. Timing and causes of death after injuries. Proc (Bayl Univ Med Cent). 2013;26(2):120–3. https://doi.org/10.1080/08998280.2013.11928934.
Kauvar DS, Lefering R, Wade CE. Impact of Hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma Acute Care Surg. 2006;60(6):S3–11.
Pacagnella RC, Souza JP, Durocher J, et al. A systematic review of the relationship between blood loss and clinical signs. PLoS One. 2013;8(3):e57594–e57594. https://doi.org/10.1371/journal.pone.0057594.
Frank M, Schmucker U, Stengel D, et al. Proper estimation of blood loss on scene of trauma: tool or tale? J Trauma Acute Care Surg. 2010;69(5):1191–5.
ATLS—Advanced Trauma Life Support Guidelines 10th Edition
Birkhahn RH, Gaeta TJ, Terry D, et al. Shock index in diagnosing early acute hypovolemia. Am J Emerg Med. 2005;23(3):323–6. https://doi.org/10.1016/j.ajem.2005.02.029.
Mutschler M, Nienaber U, Münzberg M, et al. The Shock Index revisited—a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care. 2013;17(4):R172. https://doi.org/10.1186/cc12851.
Pandit V, Rhee P, Hashmi A, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(4):1111–5. https://doi.org/10.1097/TA.0000000000000160.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700. https://doi.org/10.1136/bmj.b2700.
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA, et al. statement: An updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. https://doi.org/10.1136/bmj.n71.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1.
Covidence—Better systematic review management. https://www.covidence.org/. Accessed 1 May 2021.
Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 May 2021.
Londoño J, Niño C, Díaz J, et al. Association of clinical hypoperfusion variables with lactate clearance and hospital mortality. Shock. 2018;50(3):286–92. https://doi.org/10.1097/SHK.0000000000001066.
Salottolo KM, Mains CW, Offner PJ, et al. A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med. 2013;21:7. https://doi.org/10.1186/1757-7241-21-7.
Fröhlich M, Driessen A, Böhmer A, et al. Is the shock index based classification of hypovolemic shock applicable in multiple injured patients with severe traumatic brain injury?—An analysis of the TraumaRegister DGU(®). Scand J Trauma Resusc Emerg Med. 2016;24(1):148. https://doi.org/10.1186/s13049-016-0340-2.
Bhandarkar P, Munivenkatappa A, Roy N, et al. Pattern and distribution of shock index and age shock index score among trauma patients in towards improved trauma care outcomes (TITCO) dataset. Bull Emerg Trauma. 2018;6(4):313–7. https://doi.org/10.29252/beat-060407.
Kim SY, Hong KJ, Shin SD, et al. Validation of the shock index, modified shock index, and age shock index for predicting mortality of geriatric trauma patients in emergency departments. J Korean Med Sci. 2016;31(12):2026–32. https://doi.org/10.3346/jkms.2016.31.12.2026.
Lai W-H, Wu S-C, Rau C-S, et al. Systolic blood pressure lower than heart rate upon arrival at and departure from the emergency department indicates a poor outcome for adult trauma patients. Int J Environ Res Public Health. 2016. https://doi.org/10.3390/ijerph13060528.
Mitra B, Fitzgerald M, Chan J. The utility of a shock index ≥ 1 as an indication for pre-hospital oxygen carrier administration in major trauma. Injury. 2014;45(1):61–5. https://doi.org/10.1016/j.injury.2013.01.010.
Huang J-F, Tsai Y-C, Rau C-S, et al. Systolic blood pressure lower than the heart rate indicates a poor outcome in patients with severe isolated traumatic brain injury: a cross-sectional study. Int J Surg. 2019;61:48–52. https://doi.org/10.1016/j.ijsu.2018.11.030.
Ono Y, Yokoyama H, Matsumoto A, et al. Is preoperative period associated with severity and unexpected death of injured patients needing emergency trauma surgery? J Anesth. 2014;28(3):381–9. https://doi.org/10.1007/s00540-013-1727-0.
El-Menyar A, Abdelrahman H, Alhammoud A, et al. Prognostic role of shock index in traumatic pelvic fracture: a retrospective analysis. J Surg Res. 2019;243:410–8. https://doi.org/10.1016/j.jss.2019.05.062.
Haider A, Con J, Prabhakaran K, et al. Developing a simple clinical score for predicting mortality and need for ICU in trauma patients. Am Surg. 2019;85(7):733–7.
Odom SR, Howell MD, Gupta A, et al. Extremes of shock index predicts death in trauma patients. J Emerg Trauma Shock. 2016;9(3):103–6. https://doi.org/10.4103/0974-2700.185272.
Cannon CM, Braxton CC, Kling-Smith M, et al. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67(6):1426–30. https://doi.org/10.1097/TA.0b013e3181bbf728.
Chiu WC, Powers DB, Hirshon JM, et al. Impact of trauma centre capacity and volume on the mortality risk of incoming new admissions. BMJ Mil Health. 2020. https://doi.org/10.1136/bmjmilitary-2020-001483.
Lammers D, Conner J, Marenco C, et al. Optimal prospective predictors of mortality in austere environments. J Surg Res. 2020;255:297–303. https://doi.org/10.1016/j.jss.2020.05.040.
McNab A, Burns B, Bhullar I, et al. A prehospital shock index for trauma correlates with measures of hospital resource use and mortality. Surgery. 2012;152(3):473–6. https://doi.org/10.1016/j.surg.2012.07.010.
Singh A, Ali S, Agarwal A, et al. Correlation of shock index and modified shock index with the outcome of adult trauma patients: a prospective study of 9860 patients. N Am J Med Sci. 2014;6(9):450–2. https://doi.org/10.4103/1947-2714.141632.
Wan-Ting C, Chin-Hsien L, Cheng-Yu L, et al. Reverse shock index multiplied by Glasgow Coma Scale (rSIG) predicts mortality in severe trauma patients with head injury. Sci Rep. 2020;10(1):2095. https://doi.org/10.1038/s41598-020-59044-w.
Thom O, Taylor DM, Wolfe RE, et al. Pilot study of the prevalence, outcomes and detection of occult hypoperfusion in trauma patients. Emerg Med J. 2010;27(6):470–2. https://doi.org/10.1136/emj.2009.073254.
Pouraghaei M, Vahdati S, Moharamzadeh P, et al. The impact of prehospital emergency services on the outcome of trauma patients. Arch Trauma Res. 2020;9(3):139–42. https://doi.org/10.4103/atr.atr_75_19.
Vandromme MJ, Griffin RL, Kerby JD, et al. Identifying risk for massive transfusion in the relatively normotensive patient: utility of the prehospital shock index. J Trauma. 2011;70(2):384–90. https://doi.org/10.1097/TA.0b013e3182095a0a.
Jehan F, Con J, McIntyre M, et al. Pre-hospital shock index correlates with transfusion, resource utilization and mortality; the role of patient first vitals. Am J Surg. 2019;218(6):1169–74. https://doi.org/10.1016/j.amjsurg.2019.08.028.
Lai W-H, Rau C-S, Hsu S-Y, et al. Using the reverse shock index at the injury scene and in the emergency department to identify high-risk patients: a cross-sectional retrospective study. Int J Environ Res Public Health. 2016;13(4):357. https://doi.org/10.3390/ijerph13040357.
Kheirbek T, Thomas JM, Cao J, et al. Prehospital shock index outperforms hypotension alone in predicting significant injury in trauma patients. Trauma Surg Acute Care Open. 2021;6(1): e000712. https://doi.org/10.1136/tsaco-2021-000712.
Pottecher J, Ageron F-X, Fauché C, et al. Prehospital shock index and pulse pressure/heart rate ratio to predict massive transfusion after severe trauma: retrospective analysis of a large regional trauma database. J Trauma Acute Care Surg. 2016;81(4):713–22. https://doi.org/10.1097/TA.0000000000001191.
Schroll R, Swift D, Tatum D, et al. Accuracy of shock index versus ABC score to predict need for massive transfusion in trauma patients. Injury. 2018;49(1):15–9. https://doi.org/10.1016/j.injury.2017.09.015.
Yumoto T, Iida A, Hirayama T, et al. Immediate screening method for predicting the necessity of massive transfusions in trauma patients: a retrospective single-center study. J Intensive Care. 2014;2(1):54. https://doi.org/10.1186/s40560-014-0054-3.
Campos-Serra A, Montmany-Vioque S, Rebasa-Cladera P, et al. The use of the Shock Index as a predictor of active bleeding in trauma patients. Cir Esp. 2018;96(8):494–500. https://doi.org/10.1016/j.ciresp.2018.04.004.
Joseph B, Khan M, Truitt M, et al. Massive transfusion: the revised assessment of bleeding and transfusion (RABT) score. World J Surg. 2018;42(11):3560–7. https://doi.org/10.1007/s00268-018-4674-y.
Olaussen A, Peterson EL, Mitra B, et al. Massive transfusion prediction with inclusion of the pre-hospital Shock Index. Injury. 2015;46(5):822–6. https://doi.org/10.1016/j.injury.2014.12.009.
Plewa MC, Ewing M, Vyas N, et al. A clinical rule for predicting massive transfusion in trauma victims. Ann Emerg Med. 2013;62(4 Suppl. 1):S116. https://doi.org/10.1016/j.annemergmed.2013.07.150.
Kim MJ, Park JY, Kim MK, et al. Usefulness of shock index to predict outcomes of trauma patient: a retrospective cohort study. J Trauma Inj. 2019;32(1):17–25. https://doi.org/10.20408/jti.2018.034.
Jouini S, Jebali A, Hedhli H, et al. Predictive value of shock index ≥ 1 in severe trauma patients in emergency department. Tunis Med. 2019;97(6):802–7.
Björkman J, Raatiniemi L, Setälä P, et al. Shock index as a predictor for short-term mortality in helicopter emergency medical services: a registry study. Acta Anaesthesiol Scand. 2021;65(6):816–23. https://doi.org/10.1111/aas.13765.
Zarzaur BL, Croce MA, Fischer PE, et al. New vitals after injury: shock index for the young and age x shock index for the old. J Surg Res. 2008;147(2):229–36. https://doi.org/10.1016/j.jss.2008.03.025.
Martín-Rodríguez F, López-Izquierdo R, Del Pozo VC, et al. Accuracy of National Early Warning Score 2 (NEWS2) in prehospital triage on in-hospital early mortality: a multi-center observational prospective cohort study. Prehosp Disaster Med. 2019;34(6):610–8. https://doi.org/10.1017/S1049023X19005041.
Zhang X, Wang Z, Wang Z, et al. The prognostic value of shock index for the outcomes of acute myocardial infarction patients: a systematic review and meta-analysis. Med (United States). 2017. https://doi.org/10.1097/MD.0000000000008014.
Middleton DJ, Smith TO, et al. Shock index predicts outcome in patients with suspected sepsis or community-acquired pneumonia: a systematic review. J Clin Med. 2019. https://doi.org/10.3390/jcm8081144.
Balhara KS, Hsieh YH, Hamade B, et al. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J. 2017;34(2):89–94. https://doi.org/10.1136/emermed-2015-205532.
Funding
This study was funded by Department of Anesthesia, Centre of Head and Orthopaedics, Rigshospitalet, Denmark.
Author information
Authors and Affiliations
Contributions
MV, MØ, JS, and LSR have contributed to the conception and design of the study. MV and MØ screened articles, collected data, and assessed risk of bias. All the authors were involved in the analysis and interpretation of data as well as drafting and revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Registration and protocol
The protocol was registered in PROSPERO database of systematic reviews and can be accessed through their database. Registration number: CRD42021226881. An amendment was made when the inclusion criteria of age ≥ 18 years, was changed to age ≥ 16 years.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vang, M., Østberg, M., Steinmetz, J. et al. Shock index as a predictor for mortality in trauma patients: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 48, 2559–2566 (2022). https://doi.org/10.1007/s00068-022-01932-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01932-z