Abstract
Purpose
Both increased as well as decreased cancer mortality among psychiatric patients has been reported, but competing death causes were not included in the analyses. This study aims to investigate whether observed cancer mortality in patients with psychiatric disorders might be biased by competing death causes.
Method
In this retrospective cohort study on data from the Psychiatric Case Register Middle Netherlands linked to the death register of Statistics Netherlands, the risk of cancer death among patients with schizophrenia (N = 4,590), bipolar disorder (N = 2,077), depression (N = 15,130) and their matched controls (N = 87,405) was analyzed using a competing risk model.
Results
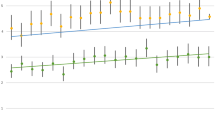
Compared to controls, higher hazards of cancer death were found in patients with schizophrenia (HR = 1.61, 95 % CI 1.26–2.06), bipolar disorder (HR = 1.20, 95 % CI 0.81–1.79) and depression (HR = 1.26, 95 % CI 1.10–1.44). However, the HRs of death due to suicide and other death causes were more elevated. Consequently, among those who died, the 12-year cumulative risk of cancer death was significantly lower.
Conclusions
Our analysis shows that, compared to the general population, psychiatric patients are at higher risk of dying from cancer, provided that they survive the much more elevated risks of suicide and other death causes.
Similar content being viewed by others
References
Commissioners in Lunacy for England and Wales (1909) Annual Report, HMSO, London
Mortensen PB (1989) The incidence of cancer in schizophrenic patients. J Epidemiol Commun Health 43:43–47
Goldacre MJ, Kurina LM, Wotton CJ, Yeates D, Seagroatt V (2005) Schizophrenia and cancer: an epidemiological study. Br J Psychiatry 187:334–338
Tran E, Rouillon F, Loze JY, Casadebaig F, Phillippe A, Vitry F, Limosin F (2009) Cancer mortality in patients with schizophrenia. Cancer 115:3555–3562
Hippisley-Cox J, Yinogradova Y, Coupland C, Parker C (2007) Risk of malignancy in patients with schizophrenia or bipolar disorder. Arch Gen Psychiatr 64:1368–1376
Saha S, Chant D, McGrath JA (2007) Systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 64:1123–1131
Hodgson R, Wildgust HJ, Bushe CJ (2010) Cancer and schizophrenia: is there a paradox? J Psychopharmacol 24(11):51–60
Hawton K, Harriss L, Zahl D (2006) Deaths from all causes in a long-term follow-up study of 11 583 deliberate self-harm patients. Psych Med 36:397–405
Carney CP, Jones LS (2006) Medical comorbidity in women and men with bipolar disorders: a population-based controlled study. Psychosom Med 68:684–691
Barchana M, Levav I, Lipshitz I, Pugachova I, Kohn R, Wezman A, Grinshpoon A (2008) Enhanced cancer risk among patients with bipolar disorder. J Affect Disord 108:43–48
Oerlemans MEJ, van den Akker M, Schuurman AG, Kellen E, Buntinx F (2007) A meta-analysis on depression and subsequent cancer risk. Clin Pract Epidemiol Ment Health 3:29
Dalton SO, Mellemkjaer L, Olsen JH, Mortensen PB, Johansen C (2002) Depression and cancer risk: a register-based study of patients hospitalized with affective disorders, Denmark, 1969–1993. Am J Epidemiol 155(12):1088–1095
Putter H, Fiocco M, Geskus RB (2006) Tutorial in biostatistics: competing risks and multi-state models. Stat Med 7(26):2389–2430
Koller MT, Stijnen T, Steyerberg EW, Lubson J (2008) Meta-analyses of chronic disease trials with competing causes of death may yield biased odds ratio. J Clin Epidemiol 61(4):365–372
Smeets HM, Laan W, Engelhard IM, Boks MPM, Geerlings MI, de Wit NJ (2011) The psychiatric case register middle Netherlands. BMC Psychiatry 11:106
Laan W, Termorshuizen F, Smeets HM, Boks MP, de Wit NJ, Geerlings MI (2011) A comorbid anxiety disorder does not result in an excess risk of death among patients with a depressive disorder. J Affect Disord 135:284–291
Coviello V, Bogess M (2004) Cumulative incidence estimation in the presence of competing risks. STATA J 4:103–112
Chou FH, Tsai KY, Su CY, Lee CC (2011) The incidence and relative risk factors for developing cancer among patients with schizophrenia: a nine-year follow-up study. Schizophr Res 129(2–3):97–103
Cohen ME, Dembling B, Schorling JB (2002) The association between schizophrenia and cancer: a population-based mortality study. Schizophr Res 57:139–146
Høyer EH, Mortensen PB, Olesen AV (2000) Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. Br J Psychiatry 176:76–82
Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V (2001) Mental disorders and cause-specific mortality. Br J Psychiatry 179:498–502
Gross AL, Gallo JJ, Eaton WW (2010) Depression and cancer risk: 24 years of follow-up of the Baltimore Epidemiologic Catchment Area sample. Cancer Causes Control 21(2):191–199
Brown S, Birtwistle J, Roe L, Thompson C (1999) The unhealthy lifestyle of people with schizophrenia. Psychol Med 29:697–701
Miech RA, Caspi A, Moffitt TE, Entner Wright BR, Silva PA (1999) Low socioeconomic status and mental disorders: a longitudinal study of selection and causation during young adulthood. AJS 104(4):1096–1131
Bebbington P, Ramana R (1995) The epidemiology of bipolar affective disorder. Soc Psychiatry Psychiatr Epidemiol 30:279–292
Tsuchiya KJ, Agerbo E, Byrne M, Mortensen PB (2004) Higher socio-economic status of parents may increase risk for bipolar disorder in the offspring. Psychol Med 34:787–793
Meyer JM, Stahl SM (2009) The metabolic syndrome and schizophrenia. Acta Psychiatr Scand 119:4–14
Steingart A, Cotterchio M, Kreiger N, Sloan M (2003) Antidepressant medication use and breast cancer risk: a case-control study. Int J Epidemiol 32:961–966
Coogan PF, Palmer JR, Strom BL, Rosenberg L (2005) Use of selective serotonin reuptake inhibitors and the risk of breast cancer. Am J Epidemiol 162:835–838
Carrillo JA, Benitez J (1999) Are antipsychotic drugs potentially chemopreventive agents for cancer? Eur J Clin Pharmacol 55:487–488
Park JK, Lee HJ, Kim JW et al (2004) Difference in p53 gene polymorphisms between Korean schizophrenia and lung cancer patients. Schizophr Res 67:71–74
Mykletun A, Bjerkeset O, Dewey M, Prince M, Overland S, Stewart R (2007) Anxiety, depression, and cause-specific mortality: the HUNT study. Psychosom Med 69:323–331
Ji J, Sundquist K, Ning Y, Kendler KS, Sundquist J, Chen X (2012) Incidence of cancer in patients with schizophrenia and their first-degree relatives: a population-based study in Sweden. Schizophr Bull. doi:10.1093/schbul/sbs065
Chou FH, Tsai KY, Su CY, Lee CC (2011) The incidence and relative risk factors for developing cancer among patients with schizophrenia: a nine-year follow-up study. Schizophr Res 129:97–103
Goldacre MJ, Wotton CJ, Yeates D, Seagroatt V, Flint J (2007) Cancer in people with depression or anxiety: record-linkage study. Soc Psychiatry Psychiatr Epidemiol 42:683–689
Mitchell AJ, Malone D, Doebbeling CC (2009) Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry 194:491–499
Polednak AP (2012) US regional differences in death rates from depression. Soc Psychiatry Psychiatr Epidemiol. doi:10.1007/s00127-012-0503-z
Bostwick JM, Pancratz VS (2000) Affective disorders and suicide risk: a reexamination. Am J Psychiatry 157:1925–1932
Palmer BA, Pankratz VS, Bostwick JM (2005) The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 62:247–253
Acknowledgments
We like to thank Statistics Netherlands (Centraal Bureau voor de Statistiek, CBS) for kindly providing the data necessary for the present analysis. Furthermore, we like to thank the participating psychiatric hospitals and services for providing all data for the database of the Psychiatric Case Register Middle Netherlands (PCR-MN). Structural funding of the Psychiatric Case Registers is provided by the participating psychiatric hospitals and services and by the Ministry of Health, Welfare and Sport (VWS). Representatives of the participating psychiatric hospitals and services co-decide on research priorities. Neither these participating psychiatric hospitals and services nor the VWS had a role in the study design, analysis, and interpretation of the data, in the writing of the present report, and in the decision to submit for publication.
Conflict of interest
All authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guan, N.C., Termorshuizen, F., Laan, W. et al. Cancer mortality in patients with psychiatric diagnoses: a higher hazard of cancer death does not lead to a higher cumulative risk of dying from cancer. Soc Psychiatry Psychiatr Epidemiol 48, 1289–1295 (2013). https://doi.org/10.1007/s00127-012-0612-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0612-8