Abstract
Purpose
While tendon degeneration has been known to be an important cause of rotator cuff disease, few studies have objectively proven the association of tendon degeneration and rotator cuff disease. The purpose of this study was to investigate changes of tendon degeneration with respect to the stage of rotator cuff disease.
Methods
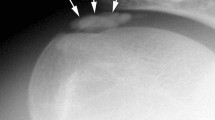
A total of 48 patients were included in the study: 12 with tendinopathy, 12 with a partial-thickness tear (pRCT), 12 with a full-thickness tear (fRCT), and 12 as the control. A full-thickness supraspinatus tendon sample was harvested en bloc from the middle portion between the lateral edge and the musculotendinous junction of the tendon using a biopsy punch with a diameter of 3 mm. Harvested samples were evaluated using a semi-quantitative grading scale with 7 parameters after haematoxylin and eosin staining.
Results
There was no significant difference in age, gender, symptom duration, and Kellgren-Lawrence grade between the groups except for the global fatty degeneration index. All of the seven parameters were significantly different between the groups and could be categorized as follows: early responders (fibre structure and arrangement), gradual responder (rounding of the nuclei), after-tear responders (cellularity, vascularity, and stainability), and late responder (hyalinization). The total degeneration scores were not significantly different between the control (6.08 ± 1.16) and tendinopathy (6.67 ± 1.83) (n.s.). However, the score of pRCT group (10.42 ± 1.31) was greater than that of tendinopathy (P < 0.001), and so was the score of fRCT (12.33 ± 1.15) than that of pRCT (p = 0.009).
Conclusion
This study showed that the degeneration of supraspinatus tendon increases as the stage of rotator cuff disease progresses from tendinopathy to pRCT, and then to fRCT. The degree of degeneration of tendinopathy was not different from that of normal but aged tendons, and significant tendon degeneration began from the stage of pRCT. The clinical relevance of the study is that strategies and goals of the treatment for rotator cuff disease should be specific to its stage, in order to prevent disease progression for tendinopathy and pRCT, as well to restore the structural integrity for fRCT.
Level of evidence
Diagnostic, Level I.


Similar content being viewed by others
References
Arnoczky SP, Lavagnino M, Egerbacher M (2007) The mechanobiological aetiopathogenesis of tendinopathy: is it the over-stimulation or the under-stimulation of tendon cells? Int J Exp Pathol 88(4):217–226
Del Buono A, Battery L, Denaro V, Maccauro G, Maffulli N (2011) Tendinopathy and inflammation: some truths. Int J Immunopathol Pharmacol 24(1 Suppl 2):45–50
Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS (2013) The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg 22(12):1628–1632
Ersen A, Demirhan M, Atalar AC, Kapicioglu M, Baysal G (2014) Platelet-rich plasma for enhancing surgical rotator cuff repair: evaluation and comparison of two application methods in a rat model. Arch Orthop Trauma Surg 134(3):405–411
Harvie P, Ostlere SJ, Teh J, McNally EG, Clipsham K, Burston BJ et al (2004) Genetic influences in the aetiology of tears of the rotator cuff. J Bone Joint Surg 86(5):696–700
Hashimoto T, Nobuhara K, Hamada T (2003) Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Orthop Relat Res 415:111–120
Hawkins RJ, Kennedy JC (1980) Impingement syndrome in athletes. Am J Sports Med 8(3):151–158
Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM (2013) Does this patient with shoulder pain have rotator cuff disease?: The Rational Clinical Examination systematic review. JAMA: J Am Med Assoc 310(8):837–847
Jo CH, Chang MS (2015) Degeneration Exists along the Entire Length of the Supraspinatus Tendon in Patients with a Rotator Cuff Tear. Clin Shoulder Elbow 18(2):61–67
Jo CH, Kim JE, Yoon KS, Lee JH, Kang SB, Lee JH et al (2011) Does platelet-rich plasma accelerate recovery after rotator cuff repair? A prospective cohort study. Am J Sports Med 39(10):2082–2090
Jo CH, Yoon KS, Lee JH, Kang SB, Lee JH, Han HS et al (2011) The effect of multiple channeling on the structural integrity of repaired rotator cuff. Knee Surg Sports Traumatol Arthrosc 19(12):2098–2107
Jobe FW, Moynes DR (1982) Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med 10(6):336–339
Kessel L, Watson M (1977) The painful arc syndrome. Clinical classification as a guide to management. J Bone Joint Surg 59(2):166–172
Khan KM, Bonar F, Desmond PM, Cook JL, Young DA, Visentini PJ et al (1996) Patellar tendinosis (jumper’s knee): findings at histopathologic examination, US, and MR imaging. Victorian Institute of Sport Tendon Study Group. Radiology 200(3):821–827
Lazarides AL, Alentorn-Geli E, Choi JH, Stuart JJ, Lo IK, Garrigues GE et al (2015) Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg 24(11):1834–1843
Lohr JF, Uhthoff HK (1990) The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res 254(254):35–38
Longo UG, Franceschi F, Ruzzini L, Rabitti C, Morini S, Maffulli N et al (2008) Histopathology of the supraspinatus tendon in rotator cuff tears. Am J Sports Med 36(3):533–538
Longo UG, Franceschi F, Ruzzini L, Rabitti C, Morini S, Maffulli N et al (2009) Characteristics at haematoxylin and eosin staining of ruptures of the long head of the biceps tendon. Br J Sports Med 43(8):603–607
Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ (2006) Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J Bone Joint Surg 88(4):489–495
McCarrel TM, Minas T, Fortier LA (2012) Optimization of leukocyte concentration in platelet-rich plasma for the treatment of tendinopathy. J Bone Joint Surg Am 94(19):e143
McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA 3rd (2015) Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med 43(2):491–500
McMaster WC, Troup J (1993) A survey of interfering shoulder pain in United States competitive swimmers. Am J Sports Med 21(1):67–70
Movin T, Guntner P, Gad A, Rolf C (1997) Ultrasonography-guided percutaneous core biopsy in Achilles tendon disorder. Scand J Med Sci Sports 7(4):244–248
Neer CS 2nd (1972) Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am 54(1):41–50
Neer CS 2nd (1983) Impingement lesions. Clin Orthop Relat Res 173(173):70–77
Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG (2007) Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res 455:52–63
Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA 3rd (2011) Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Joint Surg Am 93(19):1827–1832
Rees JD, Wilson AM, Wolman RL (2006) Current concepts in the management of tendon disorders. Rheumatology 45(5):508–521
Riley G (2008) Tendinopathy–from basic science to treatment. Nat Clin Pract Rheumatol 4(2):82–89
Sano H, Ishii H, Trudel G, Uhthoff HK (1999) Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: a comparative study with human cadaveric shoulders. J Shoulder Elbow Surg 8(6):574–579
Sundman EA, Cole BJ, Fortier LA (2011) Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med 39(10):2135–2140
Tilley JM, Murphy RJ, Chaudhury S, Czernuszka JT, Carr AJ (2014) Effect of tear size, corticosteroids and subacromial decompression surgery on the hierarchical structural properties of torn supraspinatus tendons. Bone Joint Res 3(8):252–261
van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM (1996) Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract: J R Coll Gen Pract 46(410):519–523
Via AG, De Cupis M, Spoliti M, Oliva F (2013) Clinical and biological aspects of rotator cuff tears. Muscles Ligaments Tendons J 3(2):70–79
Watson EM, Sonnabend DH (2002) Outcome of rotator cuff repair. J Shoulder Elbow Surg 11(3):201–211
Yadav H, Nho S, Romeo A, MacGillivray JD (2009) Rotator cuff tears: pathology and repair. Knee Surg Sports Traumatol Arthrosc 17(4):409–421
Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA (2006) The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 88(8):1699–1704
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H et al (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 19(1):116–120
Acknowledgements
This research was supported by a Grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (HI14C2748) and by the Bio & Medical Technology Development Program of the NRF funded by the Korean government, MSIP (NRF-2011-0019773 & 2015M3A9E6028412).
Author’s contributions
CHJ designed the study, analysed the data, and drafted the manuscript. WHS, WKP, and JEK participated in the histological assessment. SJS participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors have no conflict of interest to disclose.
Funding
This research was funded by grants of the KHIDI and the NRF (HI14C2748, NRF20110019773 & 2015M3A9E6028412).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of SMG-SNU Boramae Medical Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Jo, C.H., Shin, W.H., Park, J.W. et al. Degree of tendon degeneration and stage of rotator cuff disease. Knee Surg Sports Traumatol Arthrosc 25, 2100–2108 (2017). https://doi.org/10.1007/s00167-016-4376-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4376-7