Abstract
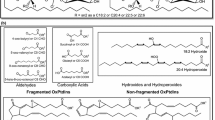
Oxylipins are oxidation products of polyunsaturated fatty acids (PUFAs) that affect a broad range of physiological processes, including cell proliferation, inflammation, inflammation resolution, and vascular function. Moreover, oxylipins are readily detectable in plasma, and certain subsets of oxylipins have been detected in human atherosclerotic lesions. Taken together, we set out to produce a detailed quantitative assessment of plasma and plaque oxylipins in a widely used model of atherosclerosis, to identify potential biomarkers of disease progression. We administered regular chow or regular chow supplemented with 0.5 % cholesterol (HC) to male New Zealand white rabbits for 12 weeks to induce hypercholesterolemia and atherosclerosis. Our targeted lipidomic analyses of oxylipins on plaques isolated from rabbits fed the HC diet detected 34 oxylipins, 28 of which were in compliance with our previously established quality control acceptance criteria. The arachidonic acid (AA) metabolite derived from the COX pathway, 6-keto-PGF1α was the most abundant plaque oxylipin, followed by the linoleic acid (LA) metabolites 9-HODE, 13-HODE and 9,12,13-TriHOME and the arachidonic acid (AA)-derivatives 11-HETE and 12-HETE. We additionally found that the most abundant oxylipins in plasma were three of the five most abundant oxylipins in plaque, namely 11-HETE, 13-HODE, and 9-HODE. The studies reported here make the first step towards a comprehensive characterization of oxylipins as potentially translatable biomarkers of atherosclerosis.




Similar content being viewed by others
Abbreviations
- AA 20:4 n-6:
-
Arachidonic acid
- ALA 18:3 n-3:
-
Polyunsaturated fatty acid precursors to oxylipin synthesis: alpha-linoleic acid
- DHA 22:6 n-3:
-
Docosahexaenoic acid
- DiHDPEs:
-
Dihydroxydocosapentaenoic acids
- DiHETEs:
-
Dihydroxyeicosatetraenoic acids
- DiHETrEs:
-
Dihydroxyeicosatrienoic acids
- DiHODEs:
-
Dihydroxyoctadecadienoic acids
- DiHOMEs:
-
Dihydroxyoctadecenoic acids
- EPA 20:5 n-6:
-
Eicosapentaenoic acid
- EpDPEs:
-
Epoxydocosapentaenoic acids
- EpETEs:
-
Epoxyeicosatetraenoic acids
- EpETrEs:
-
Epoxyeicosatrienoic acids
- EpODEs:
-
Epoxyoctadecadienoic acids
- EpOMEs:
-
Epoxyoctadecenoic acids
- HDoHEs:
-
Hydroxydocosahexaenoic acids
- HEPEs:
-
Hydroxyeicosapentaenoic acids
- HETEs:
-
Hydroxyeicosatetraenoic acids
- HODEs:
-
Hydroxyoctadecadienoic acids
- HOTrEs:
-
Hydroxyoctadecatrienoic acids
- LA 18:2 n-6:
-
Linoleic acid
- PGs:
-
Products of polyunsaturated fatty acid metabolism: prostaglandins
- TXBs:
-
Thromboxanes
References
Laufs U, Weintraub WS, Packard CJ (2013) Beyond statins: what to expect from add-on lipid regulating therapy? Eur Heart J 34(34):2660–2665
Cohen JC, Hobbs HH (2013) Genetics: simple genetics for a complex disease. Science 340(6133):689–690
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB (2013) Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127(1):e6–e245
Libby P (2005) The forgotten majority: unfinished business in cardiovascular risk reduction. J Am Coll Cardiol 46(7):1225–1228
Buczynski MW, Dumlao DS, Dennis EA (2009) Thematic Review Series: Proteomics. An integrated omics analysis of eicosanoid biology. J Lipid Res 50(6):1015–1038
Schuchardt JP, Schmidt S, Kressel G, Dong H, Willenberg I, Hammock BD, Hahn A, Schebb NH (2013) Comparison of free serum oxylipin concentrations in hyper- vs. normolipidemic men. Prostaglandins Leukot Essent Fatty Acids 89(1):19–29
Stenson WF (2007) Prostaglandins and epithelial response to injury. Curr Opin Gastroenterol 23(2):107–110
Wray J, Bishop-Bailey D (2008) Epoxygenases and peroxisome proliferator-activated receptors in mammalian vascular biology. Exp Physiol 93(1):148–154
Stables MJ, Gilroy DW (2011) Old and new generation lipid mediators in acute inflammation and resolution. Prog Lipid Res 50(1):35–51
Serhan CN, Chiang N, Van Dyke TE (2008) Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol 8(5):349–361
Spector AA, Fang X, Snyder GD, Weintraub NL (2004) Epoxyeicosatrienoic acids (EETs): metabolism and biochemical function. Prog Lipid Res 43(1):55–90
Bruins MJ, Dane AD, Strassburg K, Vreeken RJ, Newman JW, Salem N Jr, Tyburczy C, Brenna JT (2013) Plasma oxylipin profiling identifies polyunsaturated vicinal diols as responsive to arachidonic acid and docosahexaenoic acid intake in growing piglets. J Lipid Res 54(6):1598–1607
Gertow K, Nobili E, Folkersen L, Newman JW, Pedersen TL, Ekstrand J, Swedenborg J, Kuhn H, Wheelock CE, Hansson GK, Hedin U, Haeggstrom JZ, Gabrielsen A (2011) 12- and 15-lipoxygenases in human carotid atherosclerotic lesions: associations with cerebrovascular symptoms. Atherosclerosis 215(2):411–416
Quehenberger O, Armando AM, Brown AH, Milne SB, Myers DS, Merrill AH, Bandyopadhyay S, Jones KN, Kelly S, Shaner RL, Sullards CM, Wang E, Murphy RC, Barkley RM, Leiker TJ, Raetz CR, Guan Z, Laird GM, Six DA, Russell DW, McDonald JG, Subramaniam S, Fahy E, Dennis EA (2010) Lipidomics reveals a remarkable diversity of lipids in human plasma. J Lipid Res 51(11):3299–3305
Mallat Z, Nakamura T, Ohan J, Leseche G, Tedgui A, Maclouf J, Murphy RC (1999) The relationship of hydroxyeicosatetraenoic acids and F2-isoprostanes to plaque instability in human carotid atherosclerosis. J Clin Invest 103(3):421–427
Finking G, Hanke H (1997) Nikolaj Nikolajewitsch Anitschkow (1885–1964) established the cholesterol-fed rabbit as a model for atherosclerosis research. Atherosclerosis 135(1):1–7
Strassburg K, Huijbrechts AM, Kortekaas KA, Lindeman JH, Pedersen TL, Dane A, Berger R, Brenkman A, Hankemeier T, van Duynhoven J, Kalkhoven E, Newman JW, Vreeken RJ (2012) Quantitative profiling of oxylipins through comprehensive LC-MS/MS analysis: application in cardiac surgery. Anal Bioanal Chem 404(5):1413–1426
Yin W, Carballo-Jane E, McLaren DG, Mendoza VH, Gagen K, Geoghagen NS, McNamara LA, Gorski JN, Eiermann GJ, Petrov A, Wolff M, Tong X, Wilsie LC, Akiyama TE, Chen J, Thankappan A, Xue J, Ping X, Andrews G, Wickham LA, Gai CL, Trinh T, Kulick AA, Donnelly MJ, Voronin GO, Rosa R, Cumiskey AM, Bekkari K, Mitnaul LJ, Puig O, Chen F, Raubertas R, Wong PH, Hansen BC, Koblan KS, Roddy TP, Hubbard BK, Strack AM (2012) Plasma lipid profiling across species for the identification of optimal animal models of human dyslipidemia. J Lipid Res 53(1):51–65
Burleigh ME, Babaev VR, Oates JA, Harris RC, Gautam S, Riendeau D, Marnett LJ, Morrow JD, Fazio S, Linton MF (2002) Cyclooxygenase-2 promotes early atherosclerotic lesion formation in LDL receptor-deficient mice. Circulation 105(15):1816–1823
Funk CD (2006) Lipoxygenase pathways as mediators of early inflammatory events in atherosclerosis. Arterioscler, Thromb, Vasc Biol 26(6):1204–1206
Yla-Herttuala S, Rosenfeld ME, Parthasarathy S, Glass CK, Sigal E, Witztum JL, Steinberg D (1990) Colocalization of 15-lipoxygenase mRNA and protein with epitopes of oxidized low density lipoprotein in macrophage-rich areas of atherosclerotic lesions. Proc Natl Acad Sci U S A 87(18):6959–6963
Yla-Herttuala S, Rosenfeld ME, Parthasarathy S, Sigal E, Sarkioja T, Witztum JL, Steinberg D (1991) Gene expression in macrophage-rich human atherosclerotic lesions. 15-lipoxygenase and acetyl low density lipoprotein receptor messenger RNA colocalize with oxidation specific lipid-protein adducts. J Clin Invest 87(4):1146–1152
Vangaveti V, Baune BT, Kennedy RL (2010) Hydroxyoctadecadienoic acids: novel regulators of macrophage differentiation and atherogenesis. Ther Adv Endocrinol Metab 1(2):51–60
Bolick DT, Srinivasan S, Whetzel A, Fuller LC, Hedrick CC (2006) 12/15 lipoxygenase mediates monocyte adhesion to aortic endothelium in apolipoprotein E-deficient mice through activation of RhoA and NF-kappaB. Arterioscler, Thromb, Vasc Biol 26(6):1260–1266
Tam VC, Quehenberger O, Oshansky CM, Suen R, Armando AM, Treuting PM, Thomas PG, Dennis EA, Aderem A (2013) Lipidomic profiling of influenza infection identifies mediators that induce and resolve inflammation. Cell 154(1):213–227
Lundstrom SL, Levanen B, Nording M, Klepczynska-Nystrom A, Skold M, Haeggstrom JZ, Grunewald J, Svartengren M, Hammock BD, Larsson BM, Eklund A, Wheelock AM, Wheelock CE (2011) Asthmatics exhibit altered oxylipin profiles compared to healthy individuals after subway air exposure. PLoS One 6(8), e23864
Nording ML, Yang J, Hegedus CM, Bhushan A, Kenyon NJ, Davis CE, Hammock BD (2010) Endogenous Levels of Five Fatty Acid Metabolites in Exhaled Breath Condensate to Monitor Asthma by High-Performance Liquid Chromatography: Electrospray Tandem Mass Spectrometry. IEEE Sens J 10(1):123–130
Hopkins PN (2013) Molecular biology of atherosclerosis. Physiol Rev 93(3):1317–1542
Moore KJ, Sheedy FJ, Fisher EA (2013) Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol 13(10):709–721
Dennis EA, Deems RA, Harkewicz R, Quehenberger O, Brown HA, Milne SB, Myers DS, Glass CK, Hardiman G, Reichart D, Merrill AH Jr, Sullards MC, Wang E, Murphy RC, Raetz CR, Garrett TA, Guan Z, Ryan AC, Russell DW, McDonald JG, Thompson BM, Shaw WA, Sud M, Zhao Y, Gupta S, Maurya MR, Fahy E, Subramaniam S (2010) A mouse macrophage lipidome. J Biol Chem 285(51):39976–39985
Acknowledgments
The authors thank the MRL Postdoctoral Fellowship Program for financial support. L.A.B. is supported by a research fellowship provided by the MRL Postdoctoral fellowship program. The manuscript was written through contributions from all authors. All authors have given approval to the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 25 kb)
Rights and permissions
About this article
Cite this article
Bojic, L.A., McLaren, D.G., Harms, A.C. et al. Quantitative profiling of oxylipins in plasma and atherosclerotic plaques of hypercholesterolemic rabbits. Anal Bioanal Chem 408, 97–105 (2016). https://doi.org/10.1007/s00216-015-9105-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-015-9105-4