Abstract
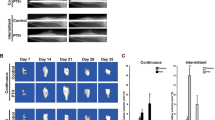
To verify whether PTH acts on bone-specific blood vessels and on cells surrounding these blood vessels, 6-week-old male mice were subjected to vehicle (control group) or hPTH [1–34] (20 µg/kg/day, PTH group) injections for 2 weeks. Femoral metaphyses were used for histochemical and immunohistochemical studies. In control metaphyses, endomucin-positive blood vessels were abundant, but αSMA-reactive blood vessels were scarce. In the PTH-administered mice, the lumen of endomucin-positive blood vessels was markedly enlarged. Moreover, many αSMA-positive cells were evident near the blood vessels, and seemed to derive from those vessels. These αSMA-positive cells neighboring the blood vessels showed features of mesenchymal stromal cells, such as immunopositivity for c-kit and tissue nonspecific alkaline phosphatase (TNALP). Thus, PTH administration increased the population of perivascular/stromal cells positive for αSMA and c-kit, which were likely committed to the osteoblastic lineage. To understand the cellular events that led to increased numbers and size of bone-specific blood vessels, we performed immunohistochemical studies for PTH/PTHrP receptor and VEGF. After PTH administration, PTH/PTHrP receptor, VEGF and its receptor flk-1 were consistently identified in both osteoblasts and blood vessels (endothelial cells and surrounding perivascular cells). Our findings suggest that exogenous PTH increases the number and size of bone-specific blood vessels while fostering perivascular/stromal cells positive for αSMA/TNALP/c-kit.







Similar content being viewed by others
References
Schweser KM, Crist BD (2017) Osteoporosis: a discussion on the past 5 years. Curr Rev Musculoskelet Med 10:265–274
Orwoll E, Scheele W, Paul S, Adami S, Syversen U, Diez-Perez A, Kaufman JM, Clancy AD, Gaich GA (2003) The effect of teriparatide [human parathyroid hormone (1–34)] therapy on bone density in men with osteoporosis. J Bone Miner Res 18:9–17
Cosman F, Hattersley G, Hu MY, Williams GC, Fitzpatrick LA, Black DM (2017) Effects of abaloparatide-SC on fractures and bone mineral density in subgroups of postmenopausal women with osteoporosis and varying baseline risk factors. J Bone Miner Res 32(1):17–23
Skripitz R, Aspenberg P (2004) Parathyroid hormone–a drug for orthopedic surgery? Acta Orthop Scand 75:654–662
Moreira CA, Fitzpatrick LA, Wang Y, Recker RR (2017) Effects of abaloparatide-SC (BA058) on bone histology and histomorphometry: the ACTIVE phase 3 trial. Bone 97:314–319
Luiz de Freitas PH, Li M, Ninomiya T, Nakamura M, Ubaidus S, Oda K, Udagawa N, Maeda T, Takagi R, Amizuka N (2009) Intermittent PTH administration stimulates pre-osteoblastic proliferation without leading to enhanced bone formation in osteoclast-less c-fos(-/-) mice. J Bone Miner Res 24:1586–1597
Yamamoto T, Hasegawa T, Sasaki M, Hongo H, Tsuboi K, Shimizu T, Ohta M, Haraguchi M, Takahata T, Oda K, Freitas PHL, Takakura A, Takao-Kawabata R, Isogai Y, Amizuka N (2016) Frequency of teriparatide administration affects the histological pattern of bone formation in young adult male mice. Endocrinology 157:2604–2620
Dhillon RS, Xie C, Tyler W, Calvi LM, Awad HA, Zuscik MJ, O’Keefe RJ, Schwarz EM (2013) PTH-enhanced structural allograft healing is associated with decreased angiopoietin-2-mediated arteriogenesis, mast cell accumulation, and fibrosis. J Bone Miner Res 28(3):586–597
Jiang X, Xu C, Shi H, Cheng Q (2019) PTH 1–34 improves bone healing by promoting angiogenesis and facilitating MSCs migration and differentiation in a stabilized fracture mouse model. PLoS ONE 14(12):e0226163
Kusumbe AP, Ramasamy SK, Adams RH (2014) Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature 507:323–328
Ramasamy SK, Kusumbe AP, Wang L, Adams RH (2014) Endothelial Notch activity promotes angiogenesis and osteogenesis in bone. Nature 507:376–380
Wang HU, Chen ZF, Anderson DJ (1998) Molecular distinction and angiogenic interaction between embryonic arteries and veins revealed by ephrin-B2 and its receptor Eph-B4. Cell 93(5):741–753
Rundle CH, Xing W, Lau KW, Mohan S (2016) Bidirectional ephrin signaling in bone. Osteoporos Sarcopenia 2:65–76
Zhao C, Irie N, Takada Y, Shimoda K, Miyamoto T, Nishiwaki T, Suda T, Matsuo K (2006) Bidirectional ephrinB2-EphB4 signaling controls bone homeostasis. Cell Metab 4:111–121
Ramasamy SK (2017) Structure and functions of blood vessels and vascular niches in bone. Stem Cells Int 2017:5046953
Armulik A, Genove G, Betsholtz C (2011) Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell 21:193–215
Sivaraj KK, Adams RH (2016) Blood vessel formation and function in bone. Development 143:2706–2715
Aizman I, Holland WS, Yang C, Bates D (2016) alphaSMA expression in large colonies of colony-forming units-fibroblast as an early predictor of bone marrow MSC expandability. Cell Med 8:79–85
Hosoya A, Nakamura H, Ninomiya T, Yoshiba K, Yoshiba N, Nakaya H, Wakitani S, Yamada H, Kasahara E, Ozawa H (2006) Immunohistochemical localization of alpha-smooth muscle actin during rat molar tooth development. J Histochem Cytochem 54(12):1371–1378
Matthews BG, Grcevic D, Wang L, Hagiwara Y, Roguljic H, Joshi P, Shin DG, Adams DJ, Kalajzic I (2014) Analysis of alphaSMA-labeled progenitor cell commitment identifies notch signaling as an important pathway in fracture healing. J Bone Miner Res 29:1283–1294
Kusumbe AP, Ramasamy SK, Itkin T, Mae MA, Langen UH, Betsholtz C, Lapidot T, Adams RH (2016) Age-dependent modulation of vascular niches for haematopoietic stem cells. Nature 532:380–384
Kunisaki Y, Bruns I, Scheiermann C, Ahmed J, Pinho S, Zhang D, Mizoguchi T, Wei Q, Lucas D, Ito K, Mar JC, Bergman A, Frenette PS (2013) Arteriolar niches maintain haematopoietic stem cell quiescence. Nature 502:637–643
Mendez-Ferrer S, Michurina TV, Ferraro F, Mazloom AR, Macarthur BD, Lira SA, Scadden DT, Ma’ayan A, Enikolopov GN, Frenette PS (2010) Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466:829–834
Root SH, Wee NK-Y, Novak S, Rosen CJ, Baron R, Matthews BG, Kalajzic I (2020) Perivascular osteoprogenitors are associated wih transcortical channels of long bones. Stem Cell 38:769–781
Hasegawa T, Yamamoto T, Sakai S, Miyamoto Y, Hongo H, Qiu Z, Abe M, Takeda S, Oda K, de Freitas PHL, Li M, Endo K, Amizuka N (2019) Histological effects of the combined administration of eldecalcitol and a parathyroid hormone in the metaphyseal trabeculae of ovariectomized rats. J Histochem Cytochem 67(3):169–184
Oda K, Amaya Y, Fukushi-Irié M, Kinameri Y, Ohsuye K, Kubota I, Fujimura S, Kobayashi J (1999) A general method for rapid purification of soluble versions of glycosylphosphatidylinositol-anchored proteins expressed in insect cells: an application for human tissue-nonspecific alkaline phosphatase. J Biochem 126:694–699
Deng W (2010) Mesenchymal stem cells express C-kit. Circ Res 107(10):e17
Amizuka N, Lee HS, Kwan MY, Arazani A, Warshawsky H, Hendy GN, Ozawa H, White JH, Goltzman D (1997) Cell-specific expression of the parathyroid hormone (PTH)/PTH-related peptide receptor gene in kidney from kidney-specific and ubiquitous promoters. Endocrinology 138(1):469–481
Jiang L, Zhang W, Wei L, Zhou Q, Yang G, Qian N, Tang Y, Gao Y, Jiang X (2018) Early effects of parathyroid hormone on vascularized bone regeneration and implant osseointegration in aged rats. Biomaterials 179:15–28
Pang PK, Tenner TE Jr, Yee JA, Yang M, Janssen HF (1980) Hypotensive action of parathyroid hormone preparations on rats and dogs. Proc Natl Acad Sci USA 77(1):675–678
Nickols GA (1985) Increased cyclic AMP in cultured vascular smooth muscle cells and relaxation of aortic strips by parathyroid hormone. Eur J Pharmacol 116(1–2):137–144
Nickols GA, Metz MA, Cline WH Jr (1986) Endothelium-independent linkage of parathyroid hormone receptors of rat vascular tissue with increased adenosine 3’,5’-monophosphate and relaxation of vascular smooth muscle. Endocrinology 119(1):349–356
He DD, Tang XT, Dong W, Cui G, Peng G, Yin X, Chen Y, Jing N, Zhou BO (2020) C-kit expression distinguishes fetal from postnatal skeletal progenitors. Stem Cell Rep 14(4):614–630
Portal-Nunez S, Lozano D, Esbrit P (2012) Role of angiogenesis on bone formation. Histol Histopathol 27:559–566
Grüneboom A, Hawwari I, Weidner D, Culemann S, Müller S, Henneberg S, Henneberg S, Brenzel A, Merz S, Bornemann L, Zec K, Wuelling M, Kling L, Hasenberg M, Voortmann S, Lang S, Baum W, Ohs A, Kraff O, Quick HH, Jäger M, Landgraeber S, Dudda M, Danuser R, Stein JV, Rohde M, Gelse K, Garbe AI, Adamczyk A, Westendorf AM, Hoffmann D, Christiansen S, Engel DR, Vortkamp A, Krönke G, Herrmann M, Kamradt T, Schett G, Hasenberg A, Gunzer M (2019) A network of trans-cortical capillaries as mainstay for blood circulation in long bones. Nat Metab 1:236–250
Marini M, Rosa I, Ibba-Manneschi L, Manetti M (2018) Telocytes in skeletal, cardiac and smooth muscle interstitium: morphological and functional aspects. Histol Histopathol 33:1151–1165
Funding
This study was partially supported by grants from Japanese Society for the Promotion of Science (JSPS, 19K10040 to Hasegawa T) and partially supported by a grant-in-aid for young scientists provided by the Japanese Association for Oral Biology and Kazato Research Foundation (Hasegawa T) and by Japan China Sasakawa Medical Fellowship (Zhao S).
Author information
Authors and Affiliations
Contributions
TH designed the study and prepared the first draft of the paper as a corresponding author. SZ is the researcher mainly in charge of this work, including RT-PCR, immunohistochemistry and TEM observation experiments. HH, MA, TY contributed to the experimental work including the preparation of paraffin samples of PTH-administered mice. TY was responsible for statistics. PHLF, ML, KT and NA participated in the discussion, editing and formatting of the manuscript. All authors revised the paper for intellectual content and approved its final version.
Corresponding author
Ethics declarations
Conflict of interest
Shen Zhao, Tomoka Hasegawa, Hiromi Hongo, Tomomaya Yamamoto, Miki Abe, Taiji Yoshida, Mai Haraguchi, Paulo Henrique Luiz de Freitas, Minqi Li, Kanchu Tei, and Norio Amizuka declare no competing interests.
Animal Rights and Informed Consent
All animal experiments in this study were conducted under the Hokkaido University Guidelines for Animal Experimentation. The experimental protocol was approved by the Hokkaido University Animal Care and Use Commitee which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (approved research proposal #15-0032).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhao, S., Hasegawa, T., Hongo, H. et al. Intermittent PTH Administration Increases Bone-Specific Blood Vessels and Surrounding Stromal Cells in Murine Long Bones. Calcif Tissue Int 108, 391–406 (2021). https://doi.org/10.1007/s00223-020-00776-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00776-2