Abstract
Aim
To explore whether long-term adherence to preventive statin therapy depends on socioeconomic position (SEP).
Methods
A cohort of individuals without established cardiovascular disease (CVD) or diabetes initiating preventive statin therapy during 2002–2005 was followed in the individual-level Danish registries for 4 years or until censoring events (death, emigration, CVD or diabetes). Only individuals aged 40–84 years for whom information was available on the SEP indicators, education and income were included (N = 76,038). Two different aspects of poor adherence were applied as outcome measures: (1) Proportion of days covered (PDC) with medication below 80 %, assuming a daily dose of one tablet (continuity); (2) Discontinuation defined as a gap between two consecutive prescriptions exceeding 365 days (persistence). Stratum-specific logistic regression analyses were applied to estimate the odds ratio (OR) for PDC <80 % across SEP, adjusting for age and hypertension. Hazard ratio (HR) for discontinuation was estimated by Cox regression analyses.
Results
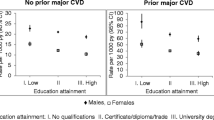
Adjusting mutually for income and education, the OR for PDC <80 % decreased with increasing income. Comparing the highest income quintile with the lowest, the OR were 0.64 (95 % Confidence Interval 0.64–0.65) and 0.73 (0.73–0.74) in men aged 40–64 and 65–84 years, respectively; in women, the figures were 0.79 (0.79–0.79) and 0.95 (0.94–0.95), respectively. While observed increases in adherence with longer education in unadjusted analyses were attenuated after adjustment for income among men, the potential inverse relationship between length of education and adherence was enhanced among women. Applying discontinuation as outcome, analogous differences were demonstrated.
Conclusion
Adherence to preventive statin therapy in Denmark decreases with decreasing income—especially in men aged 40–64 years.

Similar content being viewed by others
References
Scandinavian Simvastatin Survival Study Group (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344(8934):1383–1389
Ong HT (2005) The statin studies: from targeting hypercholesterolaemia to targeting the high-risk patient. QJM 98(8):599–614
De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J et al (2003) European guidelines on cardiovascular disease prevention in clinical practice. Third joint task force of European and other societies on cardiovascular disease prevention in clinical practice. Eur Heart J 24(17):1601–1610
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R et al (2007) European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Atherosclerosis 194(1):1–45
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G et al (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24(11):987–1003
Brindle P, Beswick A, Fahey T, Ebrahim S (2006) Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: a systematic review. Heart 92(12):1752–1759
Abramson J, Wright JM (2007) Are lipid-lowering guidelines evidence-based? Lancet 369(9557):168–169
Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P (2004) Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol 159(9):882–890
Wallach Kildemoes H, Diderichsen F, Krasnik A, Lange T, Andersen M (2012) Is the high-risk strategy to prevent cardiovascular disease equitable? A pharmacoepidemiological cohort study. BMC Publ Health 12(1):610
Getz L, Sigurdsson JA, Hetlevik I (2003) Is opportunistic disease prevention in the consultation ethically justifiable? BMJ 327(7413):498–500
McElduff P, Jaefarnezhad M, Durrington PN (2006) American, British and European recommendations for statins in the primary prevention of cardiovascular disease applied to British men studied prospectively. Heart 92(9):1213–1218
Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL (2003) Primary care: is there enough time for prevention? Am J Public Health 93(4):635–641
Manuel DG, Kwong K, Tanuseputro P, Lim J, Mustard CA, Anderson GM et al (2006) Effectiveness and efficiency of different guidelines on statin treatment for preventing deaths from coronary heart disease: modelling study. BMJ 332(7555):1419
Brugts JJ, Deckers JW (2010) Statin prescription in men and women at cardiovascular risk: to whom and when? Curr Opin Cardiol 25(4):484–489
Getz L, Sigurdsson JA, Hetlevik I, Kirkengen AL, Romundstad S, Holmen J (2005) Estimating the high risk group for cardiovascular disease in the Norwegian HUNT 2 population according to the 2003 European guidelines: modelling study. BMJ 331(7516):551
Lynch J, Davey SG, Harper S, Bainbridge K (2006) Explaining the social gradient in coronary heart disease: comparing relative and absolute risk approaches. J Epidemiol Community Health 60(5):436–441
Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J et al (1991) Health inequalities among British civil servants: the Whitehall II study. Lancet 337(8754):1387–1393
Mackenbach JP, Bos V, Andersen O, Cardano M, Costa G, Harding S et al (2003) Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol 32(5):830–837
Capewell S (2008) Will screening individuals at high risk of cardiovascular events deliver large benefits? No. BMJ 337:a1395
Rose G (1992) The strategy of preventive medicine. Oxford University Press, Oxford
Sigurdsson EL, Thorgeirsson G (2003) Primary prevention of cardiovascular diseases. Scand J Prim Health Care 21(2):68–74
Emberson J, Whincup P, Morris R, Walker M, Ebrahim S (2004) Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur Heart J 25(6):484–491
Manuel DG, Lim J, Tanuseputro P, Anderson GM, Alter DA, Laupacis A et al (2006) Revisiting Rose: strategies for reducing coronary heart disease. BMJ 332(7542):659–662
Marmot M, Friel S, Bell R, Houweling TA, Taylor S (2008) Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 372(9650):1661–1669
Atkinson T (2002) Social inclusion and the European Union. J Common Market Stud 40(4):625–643
Wallach Kildemoes H, Hendriksen C, Andersen M (2012) Drug utilization according to reason for prescribing: a pharmacoepidemiologic method based on an indication hierarchy. Pharmacoepidemiol Drug Saf 21(10):1027–1035
Bouchard MH, Dragomir A, Blais L, Berard A, Pilon D, Perreault S (2007) Impact of adherence to statins on coronary artery disease in primary prevention. Br J Clin Pharmacol 63(6):698–708
Perreault S, Blais L, Dragomir A, Bouchard MH, Lalonde L, Laurier C et al (2005) Persistence and determinants of statin therapy among middle-aged patients free of cardiovascular disease. Eur J Clin Pharmacol 61(9):667–674
Perreault S, Blais L, Lamarre D, Dragomir A, Berbiche D, Lalonde L et al (2005) Persistence and determinants of statin therapy among middle-aged patients for primary and secondary prevention. Br J Clin Pharmacol 59(5):564–573
Bates TR, Connaughton VM, Watts GF (2009) Non-adherence to statin therapy: a major challenge for preventive cardiology. Expert Opin Pharmacother 10(18):2973–2985
Larsen J, Andersen M, Kragstrup J, Gram LF (2002) High persistence of statin use in a Danish population: compliance study 1993-1998. Br J Clin Pharmacol 53(4):375–378
Poluzzi E, Strahinja P, Lanzoni M, Vargiu A, Silvani MC, Motola D et al (2008) Adherence to statin therapy and patients’ cardiovascular risk: a pharmacoepidemiological study in Italy. Eur J Clin Pharmacol 64(4):425–432
Rasmussen JN, Gislason GH, Rasmussen S, Abildstrom SZ, Schramm TK, Kober L et al (2007) Use of statins and beta-blockers after acute myocardial infarction according to income and education. J Epidemiol Commun Health 61(12):1091–1097
Hanley GE, Morgan S, Reid RJ (2011) Income-related inequity in initiation of evidence-based therapies among patients with acute myocardial infarction. J Gen Intern Med 26(11):1329–1335
Hempler NF, Diderichsen F, Larsen FB, Ladelund S, Jorgensen T (2010) Do immigrants from Turkey, Pakistan and Yugoslavia receive adequate medical treatment with beta-blockers and statins after acute myocardial infarction compared with Danish-born residents? A register-based follow-up study. Eur J Clin Pharmacol 66(7):735–742
Sanchez-Ramirez DC, Krasnik A, Kildemoes HW (2013) Do immigrants from Turkey, Pakistan and Ex-Yugoslavia with newly diagnosed type 2 diabetes initiate recommended statin therapy to the same extent as Danish-born residents? A nationwide register study. Eur J Clin Pharmacol 69(1):87–95
Ellis JJ, Erickson SR, Stevenson JG, Bernstein SJ, Stiles RA, Fendrick AM (2004) Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med 19(6):638–645
Schneeweiss S, Patrick AR, Maclure M, Dormuth CR, Glynn RJ (2007) Adherence to statin therapy under drug cost sharing in patients with and without acute myocardial infarction: a population-based natural experiment. Circulation 115(16):2128–2135
Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H (2011) Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation and archiving. Scand J Public Health 39 Suppl 7:12–16
Kildemoes HW, Sorensen HT, Hallas J (2011) The Danish national prescription registry. Scand J Public Health 39 Suppl 7:38–41
WHO Collaborating centre for Drug Statistics Methodology (2010) Guidelines for ATC classification and DDD assignment. Norwegian Institute of Public Health, Oslo
Gardarsdottir H, Souverein PC, Egberts TC, Heerdink ER (2010) Construction of drug treatment episodes from drug-dispensing histories is influenced by the gap length. J Clin Epidemiol 63(4):422–427
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish national patient register. Scand J Public Health 39[7 Suppl]:30–33
Lesen E, Sandstrom TZ, Carlsten A, Jonsson AK, Mardby AC, Sundell KA (2011) A comparison of two methods for estimating refill adherence to statins in Sweden: the RARE project. Pharmacoepidemiol Drug Saf 20(10):1073–1079
Nielsen LH, Lokkegaard E, Andreasen AH, Keiding N (2008) Using prescription registries to define continuous drug use: how to fill gaps between prescriptions. Pharmacoepidemiol Drug Saf 17(4):384–388
Kildemoes HW, Støvring H, Andersen M (2008) Driving forces behind increasing cardiovascular drug utilization: a dynamic pharmacoepidemiological model. Br J Clin Pharmacol 66(6):885–895
Ruokoniemi P, Korhonen MJ, Helin-Salmivaara A, Lavikainen P, Jula A, Junnila SY et al (2011) Statin adherence and the risk of major coronary events in patients with diabetes: a nested case–control study. Br J Clin Pharmacol 71(5):766–776
Kemp A, Roughead E, Preen D, Glover J, Semmens J (2010) Determinants of self-reported medicine underuse due to cost: a comparison of seven countries. J Health Serv Res Policy 15(2):106–114
Law MR, Cheng L, Dhalla IA, Heard D, Morgan SG (2012) The effect of cost on adherence to prescription medications in Canada. CMAJ 184(3):297–302
Olejaz M, Juul NA, Rudkjobing A, Okkels BH, Krasnik A, Hernandez-Quevedo C (2012) Denmark health system review. Health Syst Transit 14(2):I–192
Pedersen KM (2003) Pricing and reimbursement of drugs in Denmark. Eur J Health Econom 4:60–65
Thiebaud P, Patel BV, Nichol MB (2008) The demand for statin: the effect of copay on utilization and compliance. Health Econ 17(1):83–97
Gibson TB, Mark TL, Axelsen K, Baser O, Rublee DA, McGuigan KA (2006) Impact of statin copayments on adherence and medical care utilization and expenditures. Am J Manag Care 12(Spec no):SP11–SP19
Ye X, Gross CR, Schommer J, Cline R, St Peter WL (2007) Association between copayment and adherence to statin treatment initiated after coronary heart disease hospitalization: a longitudinal, retrospective, cohort study. Clin Ther 29(12):2748–2757
Thomson S, Mossialos E (2004) Influencing demand for drugs through cost sharing. In: Mossialos E, Mrazek M, Walley T (eds) Regulating pharmaceuticals in Europe: Striving for efficiency, equity and quality. Open University Press, Berkshire, pp 227–246
Marmot M (2002) The influence of income on health: views of an epidemiologist. Health Aff (Millwood ) 21(2):31–46
Brookhart MA, Patrick AR, Schneeweiss S, Avorn J, Dormuth C, Shrank W et al (2007) Physician follow-up and provider continuity are associated with long-term medication adherence: a study of the dynamics of statin use. Arch Intern Med 167(8):847–852
Benner JS, Tierce JC, Ballantyne CM, Prasad C, Bullano MF, Willey VJ et al (2004) Follow-up lipid tests and physician visits are associated with improved adherence to statin therapy. PharmacoEconomics 22[Suppl 3]:13–23
Corrao G, Scotti L, Zambon A, Baio G, Nicotra F, Conti V et al (2011) Cost-effectiveness of enhancing adherence to therapy with statins in the setting of primary cardiovascular prevention. Evidence from an empirical approach based on administrative databases. Atherosclerosis 217(2):479–485
Mauskop A, Borden WB (2011) Predictors of statin adherence. Curr Cardiol Rep 13(6):553–558
Chan DC, Shrank WH, Cutler D, Jan S, Fischer MA, Liu J et al (2010) Patient, physician, and payment predictors of statin adherence. Med Care 48(3):196–202
Hvelplund A, Galatius S, Madsen M, Sorensen R, Madsen JK, Iversen AZ et al (2012) Significance of the invasive strategy after acute myocardial infarction on prognosis and secondary preventive medication: a nationwide study of 6364 women and 11,915 men. J Invasive Cardiol 24(1):19–24
Vaidya V, Partha G, Karmakar M (2012) Gender differences in utilization of preventive care services in the United States. J Womens Health (Larchmt) 21(2):140–145
Simpson RJ Jr, Mendys P (2010) The effects of adherence and persistence on clinical outcomes in patients treated with statins: a systematic review. J Clin Lipidol 4(6):462–471
Andersohn F, Willich SN (2009) The healthy adherer effect. Arch Intern Med 169(17):1635–1636
Shrank WH, Patrick AR, Brookhart MA (2011) Healthy user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med 26(5):546–550
Tziomalos K, Athyros VG, Mikhailidis DP (2008) Statin discontinuation: an underestimated risk? Curr Med Res Opin 24(11):3059–3062
Schouten O, Hoeks SE, Welten GM, Davignon J, Kastelein JJ, Vidakovic R et al (2007) Effect of statin withdrawal on frequency of cardiac events after vascular surgery. Am J Cardiol 100(2):316–320
Pineda A, Cubeddu LX (2011) Statin rebound or withdrawal syndrome: does it exist? Curr Atheroscler Rep 13(1):23–30
Gomez Sandoval YH, Braganza MV, Daskalopoulou SS (2011) Statin discontinuation in high-risk patients: a systematic review of the evidence. Curr Pharm Des 17(33):3669–3689
Støvring H, Harmsen CG, Wisloff T, Jarbol DE, Nexoe J, Nielsen JB et al (2012) A competing risk approach for the European Heart SCORE model based on cause-specific and all-cause mortality. Eur J Prev Cardiol. doi: 10.1177/2047487312445425
Acknowledgement
This study was financed partly by a grant from the Danish Health Foundation and partly by the Nordea Foundation, the latter financing the Centre for Healthy Aging. The study was defined and performed by the researchers, only.
Conflict of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wallach-Kildemoes, H., Andersen, M., Diderichsen, F. et al. Adherence to preventive statin therapy according to socioeconomic position. Eur J Clin Pharmacol 69, 1553–1563 (2013). https://doi.org/10.1007/s00228-013-1488-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-013-1488-6