Abstract
Purpose
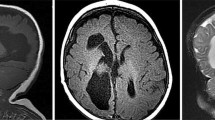
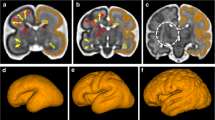
Neuroimaging techniques including structural magnetic resonance imaging (MRI) and functional positron emission tomography (PET) are useful in categorizing various midbrain-hindbrain (MHB) malformations, both in allowing diagnosis and in helping to understand the developmental processes that were disturbed. Brain imaging phenotypes of numerous malformations are characteristic features that help in guiding the genetic testing in case of direct neuroimaging-genotype correlation or, at least, to differentiate among MHB malformations entities. The present review aims to provide the reader with an update of the use of neuroimaging applications in the fine analysis of MHB malformations, using a comprehensive, recently proposed developmental and genetic classification.
Methods
We have performed an extensive systematic review of the literature, from the embryology main steps of MHB development through the malformations entities, with regard to their molecular and genetic basis, conventional MRI features, and other neuroimaging characteristics.
Results
We discuss disorders in which imaging features are distinctive and how these features reflect the structural and functional impairment of the brain.
Conclusion
Recognition of specific MRI phenotypes, including advanced imaging features, is useful to recognize the MHB malformation entities, to suggest genetic investigations, and, eventually, to monitor the disease outcome after supportive therapies.






















Similar content being viewed by others
References
Niesen CE (2002) Malformations of the posterior fossa: current perspectives. Semin Pediatr Neurol 9(4):320–34
Patel S, Barkovich AJ (2002) Analysis and classification of cerebellar malformations. AJNR Am J Neuroradiol 23:1074–1087
Parisi MA, Dobyns WB (2003) Human malformations of the midbrain and hindbrain: review and proposed classification scheme. Mol Genet Metab 80(1–2):36–53
Barkovich AJ, Millen KJ, Dobyns WB (2007) A developmental classification of malformations of the brainstem. Ann Neurol 62(6):625–39
Jissendi-Tchofo P, Kara S, Barkovich AJ (2009) Midbrain-hindbrain involvement in lissencephalies. Neurology 3;72(5):410–8
Barkovich AJ, Millen KJ, Dobyns WB (2009) A developmental and genetic classification for midbrain-hindbrain malformations. Brain 132(Pt 12):3199–230
Chizhikov V, Millen KJ (2003) Development and malformations of the cerebellum in mice. Mol Genet Metab 80(1–2):54–65
Dastjerdi FV, Consalez GG, Hawkes R (2012) Pattern formation during development of the embryonic cerebellum. Front Neuroanat 6:10
Xenaki D, Martin IB, Yoshida L, Ohyama K, Gennarini G, Grumet M, Sakurai T, Furley AJ (2011) F3/contactin and TAG1 play antagonistic roles in the regulation of sonic hedgehog-induced cerebellar granule neuron progenitor proliferation. Development 138(3):519–29
Fink AJ, Englund C, Daza RA, Pham D, Lau C, Nivison M, Kowalczyk T, Hevner RF (2006) Development of the deep cerebellar nuclei: transcription factors and cell migration from the rhombic lip. J Neurosci 15;26(11):3066–76
Bloch-Gallego E, Causeret F, Ezan F, Backer S, Hidalgo-Sánchez M (2005) Development of precerebellar nuclei: instructive factors and intracellular mediators in neuronal migration, survival and axon pathfinding. Brain Res Brain Res Rev 49(2):253–66
Sgaier SK, Millet S, Villanueva MP, Berenshteyn F, Song C, Joyner AL (2005) Morphogenetic and cellular movements that shape the mouse cerebellum; insights from genetic fate mapping. Neuron 6;45(1):27–40
Frayne R, Goodyear BG, Dickhoff P, Lauzon ML, Sevick RJ (2003) Magnetic resonance imaging at 30 Tesla: challenges and advantages in clinical neurological imaging. Invest Radiol 38(7):385–402
Runge VM, Case RS, Sonnier HL (2006) Advances in clinical 3-tesla neuroimaging. Invest Radiol 41(2):63–7
Moseley ME, Liu C, Rodriguez S, Brosnan T (2009) Advances in magnetic resonance neuroimaging. Neurol Clin 27(1):1–19
Ment LR, Bada HS, Barnes P, Grant PE, Hirtz D, Papile LA, Pinto-Martin J, Rivkin M, Slovis TL (2002) Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58(12):1726–38
Zimmerman RA, Bilaniuk LT, Pollock AN, Feygin T, Zarnow D, Schwartz ES, Harris C (2006) 3.0 T versus 1.5 T pediatric brain imaging. Neuroimaging Clin N Am 16(2):229–39
Hoon AH Jr, Melhem ER (2000) Neuroimaging: applications in disorders of early brain development. J Dev Behav Pediatr 21(4):291–302
Mugler JP III, Brookeman JR (1991) Rapid three-dimensional T1-weighted MR imaging with the MP-RAGE sequence. J Magn Reson Imaging 1:561–567
Mugler JP III, Spraggins TA, Brookeman JR (1991) T2-weighted three-dimensional MP-RAGE MR imaging. J Magn Reson Imaging 1:731–737
Conklin J, Winter JD, Thompson RT, Gelman N (2008) High-contrast 3D neonatal brain imaging with combined T1- and T2-weighted MP-RAGE. Magn Reson Med 59(5):1190–6
Srinivasan L, Dutta R, Counsell SJ, Allsop JM, Boardman JP, Rutherford MA, Edwards AD (2007) Quantification of deep gray matter in preterm infants at term-equivalent age using manual volumetry of 3-tesla magnetic resonance images. Pediatrics 119(4):759–65
Prastawa M, Gilmore JH, Lin W, Gerig G (2005) Automatic segmentation of MR images of the developing newborn brain. Med Image Anal 9:457–466
Barkovich AJ (2005) Pediatric Neuroimaging, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 294–339
Wedeen VJ, Hagmann P, Tseng WY, Reese TG, Weisskoff RM (2005) Mapping complex tissue architecture with diffusion spectrum magnetic resonance imaging. Magn Reson Med 54(6):1377–86
Tuch DS (2004) Q-ball imaging. Magn Reson Med 52(6):1358–72
Mukherjee P, McKinstry RC (2006) Diffusion tensor imaging and tractography of human brain development. Neuroimaging Clin N Am 16(1):19–43
Widjaja E, Blaser S, Raybaud C (2006) Diffusion tensor imaging of midline posterior fossa malformations. Pediatr Radiol 36(6):510–7
Wahl M, Barkovich AJ, Mukherjee P (2010) Diffusion imaging and tractography of congenital brain malformations. Pediatr Radiol 40(1):59–67
Poretti A, Meoded A, Rossi A, Raybaud C, Huisman TA (2013) Diffusion tensor imaging and fiber tractography in brain malformations. Pediatr Radiol 43(1):28–54
Patil S, Biassoni L, Borgwardt L (2007) Nuclear medicine in pediatric neurology and neurosurgery: epilepsy and brain tumors. Semin Nucl Med 37(5):357–81
Cha S (2003) Perfusion MR imaging: basic principles and clinical applications. Magn Reson Imaging Clin N Am 11(3):403–13
Cha S (2006) Dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging in pediatric patients. Neuroimaging Clin N Am 16(1):137–47
Ivancevic MK, Geerts L, Weadock WJ, Chenevert TL (2009) Technical principles of MR angiography methods. Magn Reson Imaging Clin N Am 17(1):1–11
Wang J, Licht DJ (2006) Pediatric perfusion MR imaging using arterial spin labeling. Neuroimaging Clin N Am 16(1):149–67
Sehgal V, Delproposto Z, Haacke EM, Tong KA, Wycliffe N, Kido DK, Xu Y, Neelavalli J, Haddar D, Reichenbach JR (2005) Clinical applications of neuroimaging with susceptibility-weighted imaging. J Magn Reson Imaging 22(4):439–50
Niwa T, de Vries LS, Benders MJ, Takahara T, Nikkels PG, Groenendaal F (2011) Punctate white matter lesions in infants: new insights using susceptibility-weighted imaging. Neuroradiology 53(9):669–79
Shi Y, Jin RB, Zhao JN, Tang SF, Li HQ, Li TY (2009) Brain positron emission tomography in preterm and term newborn infants. Early Hum Dev 85(7):429–32
Leach JL, Holland SK (2010) Functional MRI in children: clinical and research applications. Pediatr Radiol 40(1):31–49
Vigneron DB (2006) Magnetic resonance spectroscopic imaging of human brain development. Neuroimaging Clin N Am 16(1):75–85
Xu D, Vigneron D (2010) Magnetic resonance spectroscopy imaging of the newborn brain: a technical review. Semin Perinatol 34(1):20–7
Mamourian AC, Miller G (1994) Neonatal pontomedullary disconnection with aplasia or destruction of the lower brain stem: a case of pontoneocerebellar hypoplasia. AJNR Am J Neuroradiol 15(8):1483–5, 49-53
Barth PG, de Vries LS, Nikkels PG, Troost D (2008) Congenital brainstem disconnection associated with a syrinx of the brainstem. Neuropediatrics 39(1):1–7
Poretti A, Boltshauser E, Plecko B (2007) Brainstem disconnection: case report and review of the literature. Neuropediatrics 38(4):210–2
Sarnat HB, Benjamin DR, Siebert JR, Kletter GB, Cheyette SR (2002) Agenesis of the mesencephalon and metencephalon with cerebellar hypoplasia: putative mutation in the EN2 gene: report of 2 cases in early infancy. Pediatr Dev Pathol 5(1):54–68
Scholpp S, Lohs C, Brand M (2003) Engrailed and Fgf8 act synergistically to maintain the boundary between diencephalon and mesencephalon. Development 130(20):4881–93
Duffield C, Jocson J, Wootton-Gorges SL (2009) Brainstem disconnection. Pediatr Radiol 39(12):1357–60
Jurkiewicz E, Dobrzańska A, Nowak K, Pleskaczyńska (2010) A MRI findings in the young infant with brainstem disconnection and extracerebral features Report of one case and review of the literature. Brain Dev 32(6):495–8
Okumura A, Lee T, Shimojima K, Hisata K, Shoji H, Takanashi J, Yamamoto T, Shimizu T, Barkovich AJ (2009) Brainstem disconnection associated with nodular heterotopia and proatlantal arteries. Am J Med Genet A 149A(11):2479–83
Kumar R, Macey PM, Woo MA, Alger JR, Harper RM (2008) Diffusion tensor imaging demonstrates brainstem and cerebellar abnormalities in congenital central hypoventilation syndrome. Pediatr Res 64(3):275–80
Zaki MS, Saleem SN, Dobyns WB, Barkovich AJ, Bartsch H, Dale AM, Ashtari M, Akizu N, Gleeson JG, Grijalvo-Perez AM (2012) Diencephalic-mesencephalic junction dysplasia: a novel recessive brain malformation. Brain 135(Pt 8):2416–27
Savoiardo M, Minati L, Farina L, De Simone T, Aquino D, Mea E, Filippini G, Bussone G, Chiapparini L (2007) Spontaneous intracranial hypotension with deep brain swelling. Brain 130(Pt 7):1884–93
Chizhikov VV, Millen KJ (2005) Roof plate-dependent patterning of the vertebrate dorsal central nervous system. Dev Biol 277(2):287–95
Toelle SP, Yalcinkaya C, Kocer N, Deonna T, Overweg-Plandsoen WC, Bast T, Kalmanchey R, Barsi P, Schneider JF, Capone Mori A, Boltshauser E (2002) Rhombencephalosynapsis: clinical findings and neuroimaging in 9 children. Neuropediatrics 33:209–214
Ishak GE, Dempsey JC, Shaw DW, Tully H, Adam MP, Sanchez-Lara PA, Glass I, Rue TC, Millen KJ, Dobyns WB, Doherty D (2012) Rhombencephalosynapsis: a hindbrain malformation associated with incomplete separation of midbrain and forebrain, hydrocephalus and a broad spectrum of severity. Brain 135(Pt 5):1370–86
McAuliffe F, Chitayat D, Halliday W, Keating S, Shah V, Fink M, Nevo O, Ryan G, Shannon P, Blaser S (2008) Rhombencephalosynapsis: prenatal imaging and autopsy findings. Ultrasound Obstet Gynecol 31(5):542–8
Pasquier L, Marcorelles P, Loget P, Pelluard F, Carles D, Perez MJ, Bendavid C, de La Rochebrochard C, Ferry M, David V, Odent S, Laquerrière A (2009) Rhombencephalosynapsis and related anomalies: a neuropathological study of 40 fetal cases. Acta Neuropathol 117(2):185–200
Sukhudyan B, Jaladyan V, Melikyan G, Schlump JU, Boltshauser E, Poretti A (2010) Gómez-López-Hernández syndrome: reappraisal of the diagnostic criteria. Eur J Pediatr 169(12):1523–8
Whitehead MT, Choudhri AF, Grimm J, Nelson MD (2014) Rhombencephalosynapsis as a cause of aqueductal stenosis: an under-recognized association in hydrocephalic children. Pediatr Radiol 44(7):849–56
Engle EC (2007) Oculomotility disorders arising from disruptions in brainstem motor neuron development. Arch Neurol 64(5):633–7
Calabrese G, Telvi L, Capodiferro F, Morizio E, Pizzuti A, Stuppia L, Bordoni R, Ion A, Fantasia D, Mingarelli R, Palka G (2000) Narrowing the Duane syndrome critical region at chromosome 8q13 down to 40 kb. Eur J Hum Genet 8:319–324
Appukuttan B, Gillanders E, Juo SH, Freas-Lutz D, Ott S, Sood R, Van Auken A, Bailey-Wilson J, Wang X, Patel RJ, Robbins CM, Chung M, Annett G, Weinberg K, Borchert MS, Trent JM, Brownstein MJ, Stout JT (1999) Localization of a gene for Duane retraction syndrome to chromosome 2q31. Am J Hum Genet 65(6):1639–46
Engle EC (2010) Human genetic disorders of axon guidance. Cold Spring Harb Perspect Biol 2(3):a001784
Khan AO, Oystreck D (2006) Clinical characteristics of bilateral Duane syndrome. J AAPOS 10(3):198–201
Abramson DL, Cohen M, Mulliken JB (1998) Moëbius syndrome: classification and grading system. Plast Reconstr Surg 102:961–967
Verzijl HT, Valk J, de Vries R, Padberg GW (2005) Radiologic evidence for absence of the facial nerve in Möbius syndrome. Neurology 64(5):849–55
Pedraza S, Gámez J, Rovira A, Zamora A, Grive E, Raguer N, Ruscalleda J (2000) MRI findings in Möbius syndrome: correlation with clinical features. Neurology 55(7):1058–60
Ouanounou S, Saigal G, Birchansky S (2005) Möbius syndrome. AJNR Am J Neuroradiol 26(2):430–2
Barth PG, Majoie CB, Caan MW, Weterman MA, Kyllerman M, Smit LM, Kaplan RA, Haas RH, Baas F, Cobben JM, Poll-The BT (2007) Pontine tegmental cap dysplasia: a novel brain malformation with a defect in axonal guidance. Brain 130(Pt 9):2258–66
Denis D, Dauletbekov D, Girard N (2008) Duane retraction syndrome: type II with severe abducens nerve hypoplasia on magnetic resonance imaging. J AAPOS 12(1):91–3
Hodaie M, Quan J, Chen DQ (2010) In vivo visualization of cranial nerve pathways in humans using diffusion-based tractography. Neurosurgery 66(4):788–95
Poretti A, Boltshauser E, Doherty D (2014) Cerebellar hypoplasia: differential diagnosis and diagnostic approach. Am J Med Genet C: Semin Med Genet 166C(2):211–26
Barkovich AJ (2012) Developmental disorders of the midbrain and hindbrain. Front Neuroanat 6:7
Broccoli V, Boncinelli E, Wurst W (1999) The caudal limit of Otx2 expression positions the isthmic organizer. Nature 401(6749):164–8
Sellick GS, Barker KT, Stolte-Dijkstra I, Fleischmann C, Coleman RJ, Garrett C, Gloyn AL, Edghill EL, Hattersley AT, Wellauer PK, Goodwin G, Houlston RS (2004) Mutations in PTF1A cause pancreatic and cerebellar agenesis. Nat Genet 36(12):1301–5
Hoshino M, Nakamura S, Mori K, Kawauchi T, Terao M, Nishimura YV, Fukuda A, Fuse T, Matsuo N, Sone M, Watanabe M, Bito H, Terashima T, Wright CV, Kawaguchi Y, Nakao K, Nabeshima Y (2005) Ptf1a, a bHLH transcriptional gene, defines GABAergic neuronal fates in cerebellum. Neuron 47(2):201–13
Millen KJ, Steshina EY, Iskusnykh IY, Chizhikov VV (2014) Transformation of the cerebellum into more ventral brainstem fates causes cerebellar agenesis in the absence of Ptf1a function. Proc Natl Acad Sci USA 111(17):E1777–86
Poretti A, Prayer D, Boltshauser E (2009) Morphological spectrum of prenatal cerebellar disruptions. Eur J Paediatr Neurol 13(5):397–407
Aldinger KA, Lehmann OJ, Hudgins L, Chizhikov VV, Bassuk AG, Ades LC, Krantz ID, Dobyns WB, Millen KJ (2009) FOXC1 is required for normal cerebellar development and is a major contributor to chromosome 6p253 Dandy-Walker malformation. Nat Genet 41(9):1037–42
Calabrò F, Arcuri T, Jinkins JR (2000) Blake's pouch cyst: an entity within the Dandy-Walker continuum. Neuroradiology 42(4):290–5
Yildiz H, Yazici Z, Hakyemez B, Erdogan C, Parlak M (2006) Evaluation of CSF flow patterns of posterior fossa cystic malformations using CSF flow MR imaging. Neuroradiology 48(9):595–605
Boddaert N, Klein O, Ferguson N, Sonigo P, Parisot D, Hertz-Pannier L, Baraton J, Emond S, Simon I, Chigot V, Schmit P, Pierre-Kahn A, Brunelle F (2003) Intellectual prognosis of the Dandy-Walker malformation in children: the importance of vermian lobulation. Neuroradiology 45(5):320–4
Robinson S, Cohen AR (2000) Cowden disease and Lhermitte-Duclos disease: characterization of a new phakomatosis. Neurosurgery 46(2):371–83
Abel TW, Baker SJ, Fraser MM, Tihan T, Nelson JS, Yachnis AT, Bouffard JP, Mena H, Burger PC, Eberhart CG (2005) Lhermitte-Duclos disease: a report of 31 cases with immunohistochemical analysis of the PTEN/AKT/mTOR pathway. J Neuropathol Exp Neurol 64(4):341–9
Kulkantrakorn K, Awwad EE, Levy B, Selhorst JB, Cole HO, Leake D, Gussler JR, Epstein AD, Malik MM (1997) MRI in Lhermitte-Duclos disease. Neurology 48(3):725–31
Thomas B, Krishnamoorthy T, Radhakrishnan VV, Kesavadas C (2007) Advanced MR imaging in Lhermitte-Duclos disease: moving closer to pathology and pathophysiology. Neuroradiology 49(9):733–8
Padma MV, Jacobs M, Sequeira P, Adineh M, Satter M, Kraus G, Mantil JC (2004) Functional imaging in Lhermitte-Duclos disease. Mol Imaging Biol 6(5):319–23
Klisch J, Juengling F, Spreer J, Koch D, Thiel T, Büchert M, Arnold S, Feuerhake F, Schumacher M (2001) Lhermitte-Duclos disease: assessment with MR imaging, positron emission tomography, single-photon emission CT, and MR spectroscopy. AJNR Am J Neuroradiol 22(5):824–30
Moonis G, Ibrahim M, Melhem ER (2004) Diffusion-weighted MRI in Lhermitte-Duclos disease: report of two cases. Neuroradiology 46(5):351–4
Sener RN (1997) MR demonstration of cerebral hemimegalencephaly associated with cerebellar involvement (total hemimegalencephaly). Comput Med Imaging Graph 21(3):201–4
Flores-Sarnat L (2002) Hemimegalencephaly: part 1 genetic, clinical, and imaging aspects. J Child Neurol 17(5):373–84
Flores-Sarnat L, Sarnat HB, Dávila-Gutiérrez G, Alvarez A (2003) Hemimegalencephaly: part 2 Neuropathology suggests a disorder of cellular lineage. J Child Neurol 18(11):776–85
Finding of Rare Disease Genes (FORGE) Canada Consortium, Rivière JB, Mirzaa GM, O'Roak BJ, Beddaoui M, Alcantara D, Conway RL, St-Onge J, Schwartzentruber JA, Gripp KW, Nikkel SM, Worthylake T, Sullivan CT, Ward TR, Butler HE, Kramer NA, Albrecht B, Armour CM, Armstrong L, Caluseriu O, Cytrynbaum C, Drolet BA, Innes AM, Lauzon JL, Lin AE, Mancini GM, Meschino WS, Reggin JD, Saggar AK, Lerman-Sagie T, Uyanik G, Weksberg R, Zirn B, Beaulieu CL, Majewski J, Bulman DE, O'Driscoll M, Shendure J, Graham JM Jr, Boycott KM, Dobyns WB (2012) De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet 44(8):934–40
Lee JH, Huynh M, Silhavy JL, Kim S, Dixon-Salazar T, Heiberg A, Scott E, Bafna V, Hill KJ, Collazo A, Funari V, Russ C, Gabriel SB, Mathern GW, Gleeson JG (2012) De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nat Genet 44(8):941–5
Poduri A, Evrony GD, Cai X, Elhosary PC, Beroukhim R, Lehtinen MK, Hills LB, Heinzen EL, Hill A, Hill RS, Barry BJ, Bourgeois BF, Riviello JJ, Barkovich AJ, Black PM, Ligon KL, Walsh CA (2012) Somatic activation of AKT3 causes hemispheric developmental brain malformations. Neuron 74(1):41–8
Sato N, Yagishita A, Oba H, Miki Y, Nakata Y, Yamashita F, Nemoto K, Sugai K, Sasaki M (2007) Hemimegalencephaly: a study of abnormalities occurring outside the involved hemisphere. AJNR Am J Neuroradiol 28(4):678–82
Sato N, Ota M, Yagishita A, Miki Y, Takahashi T, Adachi Y, Nakata Y, Sugai K, Sasaki M (2008) Aberrant midsagittal fiber tracts in patients with hemimegalencephaly. AJNR Am J Neuroradiol 29(4):823–7
Colombo N, Salamon N, Raybaud C, Ozkara C, Barkovich AJ (2009) Imaging of malformations of cortical development. Epileptic Disord 11(3):194–205
Parisi MA (2009) Clinical and molecular features of Joubert syndrome and related disorders. Am J Med Genet C: Semin Med Genet 151C(4):326–40
Bolduc ME, Limperopoulos C (2009) Neurodevelopmental outcomes in children with cerebellar malformations: a systematic review. Dev Med Child Neurol 51(4):256–67
Goetz SC, Anderson KV (2010) The primary cilium: a signalling centre during vertebrate development. Nat Rev Genet 11(5):331–44
Sattar S, Gleeson JG (2011) The ciliopathies in neuronal development: a clinical approach to investigation of Joubert syndrome and Joubert syndrome-related disorders. Dev Med Child Neurol 53(9):793–8
Valente EM, Dallapiccola B, Bertini E (2013) Joubert syndrome and related disorders. Handb Clin Neurol 113:1879–88
Romani M, Micalizzi A, Valente EM (2013) Joubert syndrome: congenital cerebellar ataxia with the molar tooth. Lancet Neurol 12(9):894–905
Friede RL, Boltshauser E (1978) Uncommon syndromes of cerebellar vermis aplasia. I: Joubert syndrome. Dev Med Child Neurol 20(6):758–63
Lee SK, Kim DI, Kim J, Kim DJ, Kim HD, Kim DS, Mori S (2005) Diffusion-tensor MR imaging and fiber tractography: a new method of describing aberrant fiber connections in developmental CNS anomalies. Radiographics 25(1):53–65
Poretti A, Boltshauser E, Loenneker T, Valente EM, Brancati F, Il'Yasov K, Huisman TAGM (2007) Diffusion tensor imaging in Joubert Syndrome. AJNR 28:1929–1933
Juric-Sekhar G, Adkins J, Doherty D, Hevner RF (2012) Joubert syndrome: brain and spinal cord malformations in genotyped cases and implications for neurodevelopmental functions of primary cilia. Acta Neuropathol 123(5):695–709
Rossi A, Catala M, Biancheri R, Di Comite R, Tortori-Donati P (2004) MR imaging of brain-stem hypoplasia in horizontal gaze palsy with progressive scoliosis. AJNR Am J Neuroradiol 25(6):1046–8
Bomfim RC, Távora DG, Nakayama M, Gama RL (2009) Horizontal gaze palsy with progressive scoliosis: CT and MR findings. Pediatr Radiol 39(2):184–7
Sicotte NL, Salamon G, Shattuck DW, Hageman N, Rüb U, Salamon N, Drain AE, Demer JL, Engle EC, Alger JR, Baloh RW, Deller T, Jen JC (2006) Diffusion tensor MRI shows abnormal brainstem crossing fibers associated with ROBO3 mutations. Neurology 67(3):519–21
Avadhani A, Ilayaraja V, Shetty AP, Rajasekaran S (2010) Diffusion tensor imaging in horizontal gaze palsy with progressive scoliosis. Magn Reson Imaging 28(2):212–6
Jissendi-Tchofo P, Doherty D, McGillivray G, Hevner R, Shaw D, Ishak G, Leventer R, Barkovich AJ (2009) Pontine tegmental cap dysplasia: MR imaging and diffusion tensor imaging features of impaired axonal navigation. AJNR Am J Neuroradiol 30(1):113–9
Rudaks LI, Patel S, Barnett CP (2012) Novel clinical features in pontine tegmental cap dysplasia. Pediatr Neurol 46(6):393–6
CBCD Study Group, Briguglio M, Pinelli L, Giordano L, Ferraris A, Germanò E, Micheletti S, Severino M, Bernardini L, Loddo S, Tortorella G, Ormitti F, Gasparotti R, Rossi A, Valente EM (2011) Pontine tegmental cap dysplasia: developmental and cognitive outcome in three adolescent patients. Orphanet J Rare Dis 6:36
Caan MW, Barth PG, Niermeijer JM, Majoie CB, Poll-The BT (2014) Ectopic peripontine arcuate fibres, a novel finding in pontine tegmental cap dysplasia. Eur J Paediatr Neurol 18(3):434–8
Bacciu A, Ormitti F, Pasanisi E, Vincenti V, Zanetti D, Bacciu S (2010) Cochlear implantation in pontine tegmental cap dysplasia. Int J Pediatr Otorhinolaryngol 74(8):962–6
Desai NK, Young L, Miranda MA, Kutz JW Jr, Roland PS, Booth TN (2011) Pontine tegmental cap dysplasia: the neurotologic perspective. Otolaryngol Head Neck Surg 145(6):992–8
ten Donkelaar HJ, Lammens M, Wesseling P, Thijssen HO, Renier WO (2003) Development and developmental disorders of the human cerebellum. J Neurol 250:1025–1036
Ten Donkelaar HJ, Lammens M (2009) Development of the human cerebellum and its disorders. Clin Perinatol 36(3):513–30
Carletti B, Rossi F (2008) Neurogenesis in the cerebellum. Neuroscientist 14(1):91–100
Manto MU, Jissendi P (2012) Cerebellum: links between development, developmental disorders and motor learning. Front Neuroanat 6:1
Demaerel P (2002) Abnormalities of cerebellar foliation and fissuration: classification, neurogenetics and clinicoradiological correlations. Neuroradiology 44(8):639–46
Mimura N, Yuasa S, Soma M, Jin H, Kimura K, Goto S, Koseki H, Aoe T (2008) Altered quality control in the endoplasmic reticulum causes cortical dysplasia in knock-in mice expressing a mutant BiP. Mol Cell Biol 28(1):293–301
Miyata T, Ono Y, Okamoto M, Masaoka M, Sakakibara A, Kawaguchi A, Hashimoto M, Ogawa M (2010) Migration, early axonogenesis, and reelin-dependent layer-forming behavior of early/posterior-born Purkinje cells in the developing mouse lateral cerebellum. Neural Dev 5:23
Quattrocchi CC, Zanni G, Napolitano A, Longo D, Cordelli DM, Barresi S, Randisi F, Valente EM, Verdolotti T, Genovese E, Specchio N, Vitiello G, Spiegel R, Bertini E, Bernardi B (2013) Conventional magnetic resonance imaging and diffusion tensor imaging studies in children with novel GPR56 mutations: further delineation of a cobblestone-like phenotype. Neurogenetics 14(1):77–83
Demaerel P (2002) Abnormalities of cerebellar foliation and fissuration: classification, neurogenetics and clinicoradiological correlations. Neuroradiology 44(8):639–46,15
Devisme L, Bouchet C, Gonzalès M, Alanio E, Bazin A, Bessières B, Bigi N, Blanchet P, Bonneau D, Bonnières M, Bucourt M, Carles D, Clarisse B, Delahaye S, Fallet-Bianco C, Figarella-Branger D, Gaillard D, Gasser B, Delezoide AL, Guimiot F, Joubert M, Laurent N, Laquerrière A, Liprandi A, Loget P, Marcorelles P, Martinovic J, Menez F, Patrier S, Pelluard F, Perez MJ, Rouleau C, Triau S, Attié-Bitach T, Vuillaumier-Barrot S, Seta N, Encha-Razavi F (2012) Cobblestone lissencephaly: neuropathological subtypes and correlations with genes of dystroglycanopathies. Brain 135(Pt 2):469–82
Misciagna S (2011) Cerebellar contribution to cognitive, emotional, and behavioural functions in children with cerebellar abnormalities. Dev Med Child Neurol 53(12):1075–6
Jissendi-Tchofo P, Pandit F, Soto-Ares G, Vallee L (2011) Neuropsychological evaluation and follow-up of children with cerebellar cortical dysplasia. Dev Med Child Neurol 53(12):1119–27
Bolduc ME, Du Plessis AJ, Sullivan N, Khwaja OS, Zhang X, Barnes K, Robertson RL, Limperopoulos C (2011) Spectrum of neurodevelopmental disabilities in children with cerebellar malformations. Dev Med Child Neurol 53(5):409–16
Soto-Ares G, Delmaire C, Deries B, Vallee L, Pruvo JP (2000) Cerebellar cortical dysplasia: MR findings in a complex entity. AJNR Am J Neuroradiol 21(8):1511–9
Demaerel P, Lagae L, Casaer P, Baert AL (1998) MR of cerebellar cortical dysplasia. AJNR Am J Neuroradiol 19(5):984–6
Soto-Ares G, Devisme L, Jorriot S, Deries B, Pruvo JP, Ruchoux MM (2002) Neuropathologic and MR imaging correlation in a neonatal case of cerebellar cortical dysplasia. AJNR Am J Neuroradiol 23(7):1101–4
Jissendi-Tchofo P, Pandit F, Vallée L, Vinchon M, Pruvo JP, Baleriaux D, Soto Ares G (2012) Brain regional glucose uptake changes in isolated cerebellar cortical dysplasia: qualitative assessment using coregistrated FDG-PET/MRI. Cerebellum 11(1):280–8
Bolduc ME, du Plessis AJ, Sullivan N, Guizard N, Zhang X, Robertson RL, Limperopoulos C (2012) Regional cerebellar volumes predict functional outcome in children with cerebellar malformations. Cerebellum 11(2):531–42
PCH Consortium, Namavar Y, Barth PG, Kasher PR, van Ruissen F, Brockmann K, Bernert G, Writzl K, Ventura K, Cheng EY, Ferriero DM, Basel-Vanagaite L, Eggens VR, Krägeloh-Mann I, De Meirleir L, King M, Graham JM Jr, von Moers A, Knoers N, Sztriha L, Korinthenberg R, Dobyns WB, Baas F, Poll-The BT (2011) Clinical, neuroradiological and genetic findings in pontocerebellar hypoplasia. Brain 134(Pt 1):143–56
Rudnik-Schöneborn S, Barth PG, Zerres K (2014) Pontocerebellar hypoplasia. Am J Med Genet C: Semin Med Genet 166(2):173–83
Maricich SM, Aqeeb KA, Moayedi Y, Mathes EL, Patel MS, Chitayat D, Lyon G, Leroy JG, Zoghbi HY (2011) Pontocerebellar hypoplasia: review of classification and genetics, and exclusion of several genes known to be important for cerebellar development. J Child Neurol 26(3):288–94
Di Costanzo S, Balasubramanian A, Pond HL, Rozkalne A, Pantaleoni C, Saredi S, Gupta VA, Sunu CM, Yu TW, Kang PB, Salih MA, Mora M, Gussoni E, Walsh CA, Manzini MC (2014) POMK mutations disrupt muscle development leading to a spectrum of neuromuscular presentations. Hum Mol Genet. Jun 11
Namavar Y, Chitayat D, Barth PG, van Ruissen F, de Wissel MB, Poll-The BT, Silver R, Baas F (2011) TSEN54 mutations cause pontocerebellar hypoplasia type 5. Eur J Hum Genet 19(6):724–6
Najm J, Horn D, Wimplinger I, Golden JA, Chizhikov VV, Sudi J, Christian SL, Ullmann R, Kuechler A, Haas CA, Flubacher A, Charnas LR, Uyanik G, Frank U, Klopocki E, Dobyns WB, Kutsche K (2008) Mutations of CASK cause an X-linked brain malformation phenotype with microcephaly and hypoplasia of the brainstem and cerebellum. Nat Genet 40(9):1065–7
Mochida GH, Ganesh VS, de Michelena MI, Dias H, Atabay KD, Kathrein KL, Huang HT, Hill RS, Felie JM, Rakiec D, Gleason D, Hill AD, Malik AN, Barry BJ, Partlow JN, Tan WH, Glader LJ, Barkovich AJ, Dobyns WB, Zon LI, Walsh CA (2012) CHMP1A encodes an essential regulator of BMI1-INK4A in cerebellar development. Nat Genet 44(11):1260–4
Förster E, Bock HH, Herz J, Chai X, Frotscher M, Zhao S (2010) Emerging topics in Reelin function. Eur J Neurosci 31(9):1511–8
Burglen L, Chantot-Bastaraud S, Garel C, Milh M, Touraine R, Zanni G, Petit F, Afenjar A, Goizet C, Barresi S, Coussement A, Ioos C, Lazaro L, Joriot S, Desguerre I, Lacombe D, des Portes V, Bertini E, Siffroi JP, de Villemeur TB, Rodriguez D (2012) Spectrum of pontocerebellar hypoplasia in 13 girls and boys with CASK mutations: confirmation of a recognizable phenotype and first description of a male mosaic patient. Orphanet J Rare Dis 7:18
Takanashi J, Arai H, Nabatame S, Hirai S, Hayashi S, Inazawa J, Okamoto N, Barkovich AJ (2010) Neuroradiologic features of CASK mutations. AJNR Am J Neuroradiol 31(9):1619–22
Courchesne E (1997) Brainstem, cerebellar and limbic neuroanatomical abnormalities in autism. Curr Opin Neurobiol 7(2):269–78
Philip RC, Dauvermann MR, Whalley HC, Baynham K, Lawrie SM, Stanfield AC (2012) A systematic review and meta-analysis of the fMRI investigation of autism spectrum disorders. Neurosci Biobehav Rev 36(2):901–42
Frodl T, Skokauskas N (2012) Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatr Scand 125(2):114–26
Paloyelis Y, Mehta MA, Kuntsi J, Asherson P (2007) Functional MRI in ADHD: a systematic literature review. Expert Rev Neurother 7(10):1337–56
Stoodley CJ, Stein JF (2011) The cerebellum and dyslexia. Cortex 47(1):101–16
Shaywitz BA, Lyon GR, Shaywitz SE (2006) The role of functional magnetic resonance imaging in understanding reading and dyslexia. Dev Neuropsychol 30(1):613–32
Stoodley CJ, Schmahmann JD (2010) Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex 46(7):831–44
Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BT (2011) The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol 106(5):2322–45
Tavano A, Borgatti R (2010) Evidence for a link among cognition, language and emotion in cerebellar malformations. Cortex 46:907–18
Prats-Galino A, Soria G, de Notaris M, Puig J, Pedraza S (2012) Functional anatomy of subcortical circuits issuing from or integrating at the human brainstem. Clin Neurophysiol 123(1):4–12
Schmahmann JD (2004) Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci 16:367–78
Acknowledgments
The authors are grateful to Mazen Ahmar (MD, Radiology, Alzahra Hospital, Sharjah, (UAE) for providing us with Fig. 18.
Ethical standards and patient consent
We declare that this manuscript does not contain clinical studies or patient data.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jissendi-Tchofo, P., Severino, M., Nguema-Edzang, B. et al. Update on neuroimaging phenotypes of mid-hindbrain malformations. Neuroradiology 57, 113–138 (2015). https://doi.org/10.1007/s00234-014-1431-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1431-2