Abstract
Background
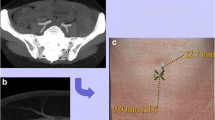
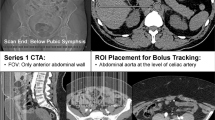
The use of the deep inferior epigastric artery perforator (DIEP) flap has gained popularity as a technique for autologous breast reconstruction. This surgery entails finely dissecting the perforators of the deep inferior epigastric artery passing through the rectus abdominis muscle, while deciding which of the perforators will best supply the flap. Computed tomography angiography (CTA) has emerged as the imaging modality of choice for preoperative evaluation. This study evaluates the accuracy of CTA in identifying perforator anatomy and flap volume calculation, as well as its impact on the patient’s outcome.
Methods
A prospective study was conducted. Thirty-two consecutive patients that underwent CT angiography prior to unilateral DIEP flap reconstruction surgery were included in the study. The control group was composed of 32 patients, who were operated on by the same surgical team, using the same surgical technique, prior to the initiation of the CTA study. The imaging provided by CTA was correlated with actual intra-operative findings. Operative time, the duration of hospital stay, and postoperative complications were assessed. The volume of the flap as calculated by CT was compared to the flap’s actual weight after harvest.
Results
CTA identified 285 perforators; of these, 278 were found intra-operatively. There was no statistically significant difference between the data provided by the CT and intra-operative findings. The use of CTA was associated with decreased operating time (unilateral, 424 versus 546 min, p < 0.0001) and significantly decreased hospitalization (unilateral, 7.6 versus 11.6 days, p = 0.0002). There was good correlation between the volume of the flap as calculated by CT and the flap’s measured weight after harvest (1117 cm3 versus 1181 g, r = 0.774).
Conclusions
CTA is an accurate tool in planning and calculating flap volume of DIEP flap and is associated with improved outcomes.
Level of Evidence: Level III, diagnostic study.


Similar content being viewed by others
References
Allen RJ, Treece P (1994) Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg 32:32–38
Blondeel PN, Vanderstraeten GG, Monstrey SJ et al (1997) The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 50:322–330
Nahabedian MY, Dooley W, Singh N, Mansan PM (2002) Contour abnormalities of the abdomen after breast reconstruction with abdominal flaps: the role of muscle preservation. Plast Reconstr Surg 109:91–101
Nahabedian MY, Momen B (2005) Lower abdominal bulge after deep inferior epigastric perforator flap (DIEP) breast reconstruction. Ann Plast Surg 54:124–129
Nahabedian MY, Momen B, Galdino G, Manson PN (2002) Breast reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 110:466–475
Masia J, Clavero JA, Larranaga JR et al (2006) Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg 59:594–599
Alonso-Burgos A, Garcia-Tutor E, Bastarrika G et al (2006) Preopearative planning of deep inferior epigastric artery perforator flap reconstruction with multi-slice-CT angiography: imaging findings and initial experience. J Plast Reconstr Aesthet Surg 59:585–593
Rozen WM, Phillips TJ, Ashton MW et al (2008) Preoperative imaging for DIEA perforator flaps: a comparative study of computed tomography and Doppler ultrasound. Plast Reconstr Surg 121:9–16
Masia J, Larranaga J, Clavera JA et al (2008) The value of the multidetector row computed tomography for the preoperative planning of deep inferior epigastric artery perforator flap. Ann Plast Surg 60:29–36
Rozen WM, Ashton MW, Stella DL et al (2008) The accuracy of computed tomography angiography for mapping the perforators of the deep inferior epigastric artery: a blinded, prospective cohort study. Plast Reconstr Surg 122:1003–1009
Masia J, Kosutic D, Clavero JA et al (2010) Preoperative computed tomographic angiogram for deep inferior epigastric artery perforator flap breast reconstruction. J Reconstr Microsurg 26:21–28
Rozen WM, Ashton MW, Grinsell D et al (2008) Establishing the case for CT angiography in the preoperative imaging of abdominal wall perforators. Microsurgery 28:306–313
Rozen WM, Anaveker HNS, Ashton MW et al (2009) Does the preoperative imaging of perforators with CT angiography improve operative outcomes in breast reconstruction? Microsurgery 28:516–523
Blondeel PN, Beyens G, Vergaeghe R et al (1998) Doppler flowmetry in the planning of perforator flaps. Br J Plast Surg 51:202–209
Giunta RE, Geisweid A, Feller AM (2000) The value of preoperative Doppler sonography for planning free perforator flaps. Plast Reconstr Surg 105:2381–2386
Hallock GG (2003) Doppler sonography and colour duplex imaging for planning a perforator flap. Clin Plast Surg 30:347–357
Taylor GI, Doyle M, McCarten G (1990) The Doppler probe for planning flaps: anatomical study and clinical applications. Br J Plast Surg 43:1–16
Chernyak V, Rozenbit AM, Greenspun DT et al (2009) Breast reconstruction with deep inferior epigastric artery perforator flap: 3.0-T gadolinium-enhanced MR imaging for preoperative localizing of abdominal wall perforators. Radiology 250:417–424
Schaverien MV, Ludman CN, Neil-Dwyer J et al (2011) Contrast-enhanced magnetic resonance angiography for preoperative imaging of deep inferior epigastric artery perforator flaps: advantages and disadvantages compared with computed tomography angiography: a United Kingdom perspective. Ann Plast Surg 67:671–674
Casey WJ, Chew RT, Rebecca AM et al (2009) Advantages of preoperative computed tomography in deep inferior epigastric artery perforator flap breast reconstruction. Plast Reconstr Surg 123:1148–1155
Gacto-Sanchez P, Sicilia-Castro D, Gomez-Cia T et al (2009) Computed tomographic angiography with VirSSPA three-dimensional software for perforator navigation improves preoperative outcomes in DIEP flap breast reconstructions. Plast Reconstr Surg 125:24–31
Saba L, Atzeni M, Ribuffo D et al (2012) Analysis of deep inferior epigastric perforator (DIEP) arteries by using MDCTA: comparison between 2 post-processing techniques. Eur J Radiol 81(8):1828–1833
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
An approval from the ethical committee of the hospital was obtained. Therefore, the study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Patient consent
All patients provided verbal and written informed consent before their inclusion in this study.
Conflict of interest
Galia Ronen, Arye Blachar, Aryeh Abelow, Eyal Gur, and Yoav Barnea declare that they have no conflict of interest.
Funding
None
Rights and permissions
About this article
Cite this article
Ronen, G., Blachar, A., Abelow, A. et al. Computed tomography angiography (CTA) assisted preoperative planning and volume calculation of deep inferior epigastric artery perforator (DIEP) flap for breast reconstruction. Eur J Plast Surg 40, 441–446 (2017). https://doi.org/10.1007/s00238-017-1295-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-017-1295-x