Abstract
Cardiac MRI is in many respects an ideal modality for pediatric cardiovascular imaging, enabling a complete noninvasive assessment of anatomy, morphology, function and flow in one radiation-free and potentially non-contrast exam. Nonetheless, traditionally lengthy and complex imaging acquisition strategies have often limited its broader use beyond specialized centers. In this review, the author presents practical cardiac MRI imaging protocols to facilitate the performance of succinct yet successful exams that provide the most salient clinical data for the majority of congenital and acquired pediatric cardiac disease. In addition, the author reviews newer and evolving techniques that permit more rapid but similarly diagnostic MRI, including compressed sensing and artificial intelligence/machine learning reconstruction, four-dimensional flow acquisition and blood pool contrast agents. With the modern armamentarium of cardiac MRI methods, the goal of compact yet comprehensive exams in children can now be realized.
Similar content being viewed by others
Introduction
Cardiovascular pathology comprises a substantial burden of illness in children. Congenital heart disease (CHD) arises in approximately 1 in 100 live births, while cardiomyopathy affects 1 in 100,000 children, at a rate similar to the more common pediatric cancers [1, 2]. Given the variety and complexity of disease, often nonspecific signs and symptoms, and persistence of morbidity among survivors into adulthood, imaging has become essential in the diagnosis and long-term follow-up of these disorders [3, 4]. Echocardiography remains the first-line modality, although its operator-dependence and potential visualization limitations, particularly for intricate malformations and postsurgical anatomy, might necessitate additional complementary modalities [3,4,5]. Cardiac catheterization has for more than 50 years been considered the reference standard for assessing CHD, but its invasive nature discourages its routine diagnostic use [5]. While cardiac CT has become an increasingly attractive alternative, its associated risks of ionizing radiation and iodinated contrast exposure, suboptimal ability to distinguish soft tissues, and lack of flow information diminish its broader utility [4, 5].
Considering the limitations and risks of other complementary modalities, cardiac MRI, in use for more than two decades, has assumed a central role in evaluating both congenital and acquired pediatric cardiovascular disease [5, 6]. In a single exam, precise delineation of cardiac anatomy, comprehensive myocardial and other tissue characterization, and quantitative interrogation of ventricular volumetry, function and flow can be simultaneously achieved [6]. Multiplanar and three-dimensional (3-D) imaging can be readily acquired, and intravenous (IV) contrast agent is not strictly required in many circumstances [5,6,7]. Moreover, there is no ionizing radiation, obviating this key concern among patients prone to frequent follow-up imaging [5].
Relative to other modalities, cardiac MRI, unless contraindicated (e.g., because of an incompatible implanted device), is the noninvasive the test of choice for myocardial evaluation (e.g., for myocarditis or infarct) and volumetry and flow quantification (e.g., for postoperative CHD or valvular heart disease). Depending on local experience and resources, cardiac CT is often preferred for anatomical assessment (e.g., for preoperative CHD), particularly if the coronaries, lungs or airways are of primary concern, although comparable image quality can be achieved with MRI. In either case, echocardiography is generally first performed to help guide the need for further imaging and the specific questions to be answered.
Yet, despite its many potential uses, cardiac MRI poses several challenges that serve to limit its mainstream application in pediatric cardiovascular disease. The most important of these is the technical expertise required to obtain reliably diagnostic scans, including efficient localization of appropriate scan planes in the setting of complex congenital malformations [7]. Moreover, children pose distinct imaging considerations, with inherently smaller anatomy, higher heart rates and difficulty complying with breath-holding instructions and remaining still for exams that often last at least an hour [5, 7]. In younger children, sedation or general anesthesia might be inevitable, requiring additional resources and close patient monitoring [7]. Even when diagnostic exams are obtained, a large amount of data is often amassed that requires efficient reconstruction as well as post-processing and synthesis by an imager with requisite experience [5, 7, 8].
Nonetheless, with a parsimonious approach to image acquisition and effective use of available techniques, the goal of reliably diagnostic yet efficient cardiac MRI in children can now be readily achieved. Herein, the author presents practical cardiac MRI protocols and pearls to facilitate obtaining the most essential qualitative and quantitative data in expedient fashion. In addition, the authors reviews newer methods enabling more rapid and less technically onerous exams with equal or better image quality, including compressed sensing and artificial intelligence (AI)/machine learning reconstruction, use of blood pool contrast agents, and four-dimensional (4-D) flow acquisition strategies. The author also addresses emerging tools to help mitigate workflow inefficiencies while increasing throughput.
General exam considerations
While pediatric cardiac MRI is often individually tailored to the unique circumstances, some general principles apply to help improve the patient experience and probability of a successful yet expedient scan. Careful advance preparation is crucial, and child life staff, if available, should be engaged to discuss the exam in a child-friendly manner with the child and parents while practicing breath-holding instructions and remaining motionless during the study duration [9, 10]. Inspiratory breath-holds are often better understood and tolerated than are end-expiratory breath-holds [9]. Allowing a parent to remain in the MRI scanner room after requisite safety screening can help reduce the child’s anxiety. If available, a mock scanner visit can be arranged to better familiarize the child with the environment [9, 10]. The scanner can be adorned with visually appealing and child-friendly designs (Fig. 1). MRI-compatible video goggles and virtual reality systems can be useful distractions, especially for longer exams (Fig. 2) [10]. Finally, exams should in general be limited to the briefest and most relevant sequences to ensure the highest-priority clinical questions are answered, noting that children are often prone to repeated follow-up imaging [9].
To mitigate cardiac motion, electrocardiographic (ECG) leads are placed on the child, and cardiac MRI sequences are synchronized to the cardiac tracing. Acquisitions might either be prospectively triggered to begin obtaining a segment of k-space with each R wave, or retrospectively gated, with k-space data obtained throughout the cardiac cycle [9, 11]. To minimize respiratory motion, acquisitions can be completed over a breath-hold, although this is more feasible in older children (e.g., older than 7 years), compliant children, and in anesthetized and intubated children in whom breath-holds can be controlled. To avoid the last scenario, a free-breathing approach employing multiple signal averaging can be considered, although with resultant lesser spatial resolution [9]. Alternatively, a respiratory navigator can be utilized, tracking motion of the diaphragm and triggering data acquisition in end-expiration; however, this comes at the cost of increased scan time [9, 12]. Finally, for patient/bulk motion, in addition to the previously described patient preparatory strategies as well as use of sedation, other tactics include the “feed-and-wrap” approach to induce sleep in young infants (e.g., younger than 6 months) and soft (e.g., foam) restraints, with variable effectiveness [9, 13].
Another key consideration is the selection of 1.5-tesla (T) versus 3-T magnetic field strength. Three tesla offers intrinsically higher signal-to-noise and greater ability to leverage acceleration techniques for more efficient imaging, which in the author’s institutional experience are particularly beneficial in the case of neonates and small children [14, 15]. Nonetheless, cardiac MRI at 3 T is notoriously challenging, primarily because of the greater magnetic field inhomogeneities with resultant artifacts as well as specific absorption rate (SAR) limits constraining the use of pulse sequences generating high-power output [15, 16]. Moreover, scan parameters that have been fine-tuned for 1.5 T through long-term experience cannot be directly translated to 3 T and require dedicated adjustments to achieve optimal image quality [14]. Thus, 1.5 T understandably remains the field strength of choice for cardiac MRI at many centers, although ongoing advances might help more broadly ease the transition to 3 T [15].
As in any MRI examination, appropriate safety screening procedures must also be followed to ensure any implanted devices are safe within the magnet using the desired acquisition strategy. Notably, cardiac MRI is now often possible even in children with cardiac implantable electronic devices such as pacemakers. At the author’s institution, in such cases, an intake/triage process is performed in conjunction with electrophysiology and in accordance with Heart Rhythm Society and European Society of Cardiology guidelines, including extensive data-gathering on the exam indications, alternatives, type of device and length of implantation, and patient pacing-dependence [17,18,19]. When the decision is made to proceed, devices are programmed to an MRI-safe conditional pacing mode as per manufacturer guidance by electrophysiology and then reset to previous settings immediately after scan completion. Children are observed throughout with cardiology/electrophysiology support and continuous ECG monitoring [20]. In addition to inherent safety considerations, pacemakers and other implanted devices might also result in artifacts, which can be diagnostically acceptable but should be considered before commencing or continuing the exam [20, 21]. However, the presence of a pacemaker no longer should reflexively exclude consideration for cardiac MRI if the exam is otherwise clinically appropriate and the potential benefits outweigh risks.
Coil selection
As in other areas of MRI, use of appropriate coils is crucial to obtaining high-quality cardiac imaging. Both a transmit (volume) coil that can elicit a homogeneous field in a large region and a receive (surface) coil that enables a high signal-to-noise ratio (SNR) in a localized region are needed. These elements can now be effectively bundled using phased-array coils that combine small coil elements for high SNR in a larger-volume region [22]. In addition, phased-array coils facilitate parallel imaging, a form of imaging acceleration in which k-space is reconstructed from undersampled data acquired by the coil elements [23]. These have been further enhanced by a multiple receiver channel design that allows significant acquisition time savings when combined with parallel imaging methods. At least 8- and commonly up to 32-channel coil arrays are used in cardiac MRI [22, 24].
Nevertheless, most available commercial coils are designed for adult-size patients and are relatively rigid and uncomfortable for pediatric patients. Recently, flexible screen-printed coils have come to fruition; in such devices, the coil elements are printed onto a woven fabric that is child-friendly and improves SNR because of its compact fit, including for cardiac applications [25]. High-flexibility coils that can conform to patient contours, as such as the Adaptive Image Receive (AIR) technology (GE Healthcare, Waukesha, WI), are now increasingly available from commercial vendors and promising for pediatric MRI of the heart and other anatomical regions (Fig. 3) [26, 27].
Flexible MRI coils. Photograph shows several flexible MRI coils (arrows), resting on an MRI table. Better conforming to patient contours than traditional devices, these coils can provide both greater comfort and higher signal-to-noise ratio (SNR) because of their more compact fit. Specific vendor names have been masked
Protocol development
Establishment of an appropriate pediatric cardiac MRI protocol first requires a clear understanding of the anticipated exam goals. In the author’s experience, broadly, most pediatric cardiac MRI is performed for cardiomyopathy (to include myocarditis and viability studies) or CHD (encompassing valvular heart disease and aortopathies along with shunts and complex lesions) [28]. In cardiomyopathy, the main objectives are to establish cardiac morphology, ventricular volumetry/function ± mass, and myocardial tissue characterization [29]. In CHD, the exam generally includes an assessment of intracardiac and extracardiac anatomy and any complicating features (either presurgical or postoperative), ventricular volumetry/function ± mass, valvular function, and pertinent vascular flow measurements [30]. Additional myocardial tissue characterization might be considered in CHD because of its potential prognostic value but is generally not the most essential information in this setting [31]. Herein, this review focuses on these two dominant clinical pathways (cardiomyopathy and CHD). Other indications such as cardiac tumor, pericardial disease/constrictive pericarditis, coronary evaluation and myocardial ischemia/stress perfusion arise less often in typical practice and require dedicated protocols [28].
Cardiomyopathy
Protocol overview
The minimum sequences in a typical protocol for cardiomyopathy consist of (1) cinematic (cine) imaging and (2) late gadolinium enhancement (LGE) [32]. Cine images facilitate qualitative assessment of regional and global biventricular function. In addition, biventricular volumes and ejection fractions can be quantified by tracing biventricular endocardial contours (and epicardial contours, if myocardial mass measurements are needed) in end-diastole and end-systole using dedicated software [29, 32]. LGE imaging allows for identification of areas of myocardial inflammation or fibrosis. These are manifested as foci of high signal caused by the accumulation of gadolinium in tissues with increased extracellular volume fraction with resultant T1-shortening effects [29]. A sample compact cardiomyopathy MRI protocol with pertinent scan parameters at 1.5 T is shown in Table 1.
Both cine and LGE imaging are typically performed in the short-axis plane from base to apex (forming an image “stack”), perpendicular to the long-axis of the body of the left ventricle (LV) based on vertical long axis (LV 2-chamber) and horizontal long axis (4-chamber) localizers. In addition, true 4-chamber and LV 3-chamber views are typically obtained (Fig. 4). These are prescribed to pass through the LV apex, center of the mitral valve and, respectively, the centers of the tricuspid and aortic valves. Finally, the true LV 2-chamber is obtained by a slice passing through the intersection of the 4-chamber and LV 3-chamber prescriptions, thus capturing the anterior and inferior LV myocardial walls. The typical slice thickness is 6–8 mm; for stacks, a 2–4-mm interslice gap (total of 10-mm coverage) might be considered [32].
Standard left ventricular (LV) planes. a–d Short-axis (a), 4-chamber (b), LV 3-chamber (c) and LV 2-chamber (d) end-diastolic balanced steady-state free precession images in a 15-year-old boy with chest pain and a normal cardiac MRI exam. Ao aorta, LA left atrium, RA right atrium, RV right ventricle
Cine imaging considerations
Cine imaging is made possible by capturing imaging data for multiple phases (time points) in the cardiac cycle. By averaging the data for each phase over multiple cardiac cycles in a typically single breath-hold acquisition, a high-resolution of image of each phase can be reconstructed; displaying the images sequentially creates a movie (“cine”) [29]. Cine imaging is achieved through the use of gradient echo (GRE) acquisitions, either spoiled gradient echo (SPGR) or balanced steady-state free precession (bSSFP) [29, 30]. Of these, bSSFP (“bright blood”) is usually preferred because of its higher temporal resolution, SNR and myocardial–blood pool contrast [30, 32].
Because the multi-breath-hold approach to obtain a stack of cine images can be both time-consuming and challenging for children, methods to achieve faster cine imaging have received much interest. As alluded to earlier, parallel imaging has been made possible by phased-array, multichannel receiver coils and is routinely used to accelerate cardiac MRI cine sequences, with a typical acceleration factor of 2 at 1.5 T [32, 33]. Parallel imaging reconstruction algorithms include sensitivity encoding (SENSE) and generalized auto-calibrating partially parallel acquisition (GRAPPA), which use coil sensitivity profiles to perform anti-aliasing (image-based reconstruction) and k-space interpolation (k-space-based reconstruction), respectively [33]. With a streamlined approach and effective use of parallel imaging, relatively efficient cardiac cine imaging can be achieved. For example, in a recent study comparing abbreviated cardiac cine MRI to echocardiography in a cohort of people with Duchenne muscular dystrophy, clinical utility and image quality were rated higher for MRI, while exam duration and patient satisfaction were not statistically different between the two groups [34]. However, there is a limit to the degree of acceleration that is possible with parallel imaging due to reduced SNR and greater artifacts with increasing acceleration [33].
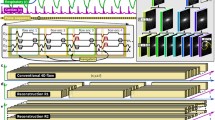
To further increase the speed of cardiac MRI cine imaging, there has been growing use of compressed sensing, involving reconstruction from a pseudorandom undersampling of k-space by leveraging image compressibility (sparsity) [35, 36]. Such techniques can be combined with parallel imaging and are now incorporated into some commercial cardiac MRI cine sequences, allowing further acceleration with relatively immediate image generation. In pilot studies of pediatric patients comparing compressed sensing cardiac cine to conventional acquisitions (both also utilizing parallel imaging acceleration), researchers found similar qualitative image quality and volume, function and LV mass estimates between the two groups, despite reduced (or no) breath-holds and shorter scan times in the compressed sensing cohort [36, 37]. However, with increasing acceleration, there was greater spatial blurring in the compressed sensing group, attributed to the pseudorandom undersampling strategy [37].
More recently, there has been expanding interest in applying artificial intelligence (AI), machine learning and deep learning methods to reconstruct higher-resolution cardiac cine MRI for a given acquisition time or to shorten acquisition time without degrading (or even improving) image quality from undersampled k-space. Such techniques use previous cardiac cine acquisitions (in the image or k-space domain) as training data to develop models for optimizing reconstruction on new cases (not part of the training data) [38,39,40]. In a small pilot study of adults, a deep learning algorithm was trained on fully sampled cardiac cine acquisitions and developed to optimize a parallel imaging reconstruction strategy known as ESPIRiT (eigenvalue-based iterative self-consistent parallel imaging reconstruction) [39,40,41,42]. The method was shown to outperform ESPIRiT combined with compressed sensing for overall image quality and accuracy of left ventricular segmentation when used in conjunction with a 12-fold accelerated bSSFP cardiac cine sequence [39, 41, 42]. A further enhanced version of this deep learning ESPIRiT technique used in combination with a 12-fold accelerated cardiac cine bSSFP sequence was later prospectively compared to conventional bSSFP with parallel imaging in a cohort of pediatric and young adult patients; the two protocols showed similar image quality and volumetry estimates despite substantial time-savings in the deep learning group (Fig. 5) [40]. Additional ongoing research centers on using deep learning to improve traditionally slow reconstruction times in non-Cartesian (e.g., radial) k-space cardiac cine sampling strategies, which otherwise offer shorter acquisition times and increased SNR [43, 44].
Utility of deep learning reconstruction for cardiac cine imaging, here in a 17-year-old girl with hypertrophic cardiomyopathy. a Short-axis end-diastolic conventional balanced steady-state free precession (bSSFP) image shows asymmetrical septal hypertrophy (arrow). LV left ventricle, RV right ventricle. b Short-axis free-breathing deep-learning-reconstructed and 12-fold-accelerated end-diastolic bSSFP image shows slightly less detail but adequate demonstration of the thickened septum (arrow) and ventricles. This is despite an almost 70% reduction in prescribed acquisition time, even without accounting for conventional cine breath-hold and recovery time
A general concern about deep learning reconstruction strategies is that they could produce unusual artifacts or images that obscure important pathology (potentially unbeknown to the interpreter), given that they are based on limited training data [45]. However, this phenomenon might be at least partially mitigated by using deep learning to optimize a k-space and physics-based algorithm with less dependency on the specific images used for training [40]. Nevertheless, while research efforts in deep learning–based reconstruction for cardiac cine imaging appear promising, practical vendor-based solutions are not available at the present time.
Late gadolinium enhancement imaging considerations
Along with functional assessment, LGE is a cornerstone of cardiomyopathy evaluation. Intravenous gadolinium is administered at a typical dose of 0.1–0.2 mmol/kg and images are obtained beginning approximately 8–10 min after injection, up to 30 min post contrast administration [29, 32]. The optimal delay between contrast injection and the start of acquisitions might be shorter, depending on the gadolinium dose and patient physiology. Images are typically obtained in the same planes as cine images (short-axis stack, LV 2- and 3-chamber, 4-chamber), with similar slice thickness, usually in diastole [32].
Central to LGE acquisitions is the use of an inversion recovery (IR) pulse to “null” the normal myocardium so that it appears as dark signal, while abnormal areas of myocardium are high in signal; the operator sets the inversion time (TI) at which the normal myocardium visually appears blackest [29, 46]. There are several methods for achieving LGE, including two-dimensional (2-D) segmented IR with either a gradient recalled echo (GRE) or bSSFP readout, 2-D phase-sensitive inversion recovery (PSIR) with either a GRE or bSSFP readout, and three-dimensional (3-D) IR with a GRE readout. In addition, a 2-D single-shot PSIR-bSSFP sequence is available (Fig. 6) [32, 47]. Preceding LGE acquisitions, a TI scout image, which cycles in cine fashion through a range of TIs, might be considered to help select the optimal TI, although there is imperfect concordance with the optimal TI on subsequent LGE (up to 50-ms difference) [32].
Comparison of late-gadolinium-enhancement techniques in a 17-year-old boy with myocarditis after messenger ribonucleic acid (mRNA)-based coronavirus disease 2019 (COVID-19) vaccination. a–c Short-axis two-dimensional (2-D) inversion recovery (IR) late-gadolinium-enhancement (a), short-axis 2-D phase-sensitive inversion recovery (PSIR) late-gadolinium-enhancement (b) and short-axis 2-D single-shot PSIR late-gadolinium-enhancement (c) images show abnormal subepicardial to mesocardial late myocardial enhancement (arrows). The findings on the PSIR images (b and c) are more conspicuous, even with using the faster single-shot technique. LV left ventricle, RV right ventricle
An advantage of PSIR techniques is that the myocardium remains relatively nulled regardless of the set TI. This can be particularly helpful for less experienced or efficient technologists because the optimal TI changes as contrast agent washes out of the heart, while at the same time there is a limited time window in which diagnostic images can be obtained [46, 47]. However, PSIR might be less sensitive for subendocardial LGE compared to IR techniques [47]. Three-dimensional whole-heart acquisitions offer higher spatial resolution and the ability to perform multiplanar reformats. However, because of their generally longer scan time and lack of phase-sensitive options, gadolinium washout can be problematic at a preselected TI [46]. Finally, despite a lower SNR compared to segmented 2-D PSIR techniques, 2-D single-shot PSIR-bSSFP LGE is relatively rapid, able to image the full heart in one breath-hold, and thus can be an excellent alternative in children with arrhythmia or difficulty breath-holding [32, 46]. In addition, it should be noted that deep learning–based vendor solutions are becoming available to retrospectively reconstruct LGE images with higher SNR and spatial resolution and decreased truncation artifacts (Fig. 7) [48].
Improved late-gadolinium-enhancement imaging with deep-learning-based reconstruction in a 9-year-old boy with a history of multisystem inflammatory syndrome in children (MIS-C) after coronavirus 2019 (COVID-19) infection. a Four-chamber two-dimensional (2-D) phase-sensitive inversion recovery (PSIR) late-gadolinium-enhanced image shows normal and expected myocardial signal but with significant overall image noise. LA left atrium, LV left ventricle, RA right atrium, RV right ventricle. b Corresponding image using a vendor-supplied deep-learning-based reconstruction algorithm shows qualitatively substantially improved image quality
Advanced tissue characterization
Additional tissue characterization sequences are not mandatory but are increasingly used and can be considered depending on the clinical scenario, institutional preferences and patient tolerance. Select slices are obtained at least in the short-axis plane with slice thicknesses similar to those used for cine images [32]. Such (pre-contrast) supplemental sequences include: T1 mapping (usually with a modified Look-Locker inversion recovery [MOLLI] approach), T2 mapping (single-shot, gradient/spin echo, or fast spin echo [FSE]), and T2* mapping (multi-echo GRE), which can be helpful for assessing diffuse fibrosis, diffuse myocardial edema and myocardial iron deposition, respectively. In addition, conventional multi-slice black blood (IR) or bright blood (single-shot or FSE-bSSFP) T2-weighted imaging might be pursued to evaluate for focal myocardial edema, e.g., in the setting of suspected myocarditis (Fig. 8) [29, 31, 32]. Non-contrast T1-mapping would seem a promising alternative to LGE imaging; however, it should be noted that native T1 values vary depending on magnetic field strength, scanner software, manufacturer, sequences used and patient-specific factors (e.g., heart rate) [49, 50]. Extracellular volume fraction is less variable and can be calculated using both pre- and post-gadolinium (10–30 min after administration) T1-map images if the child’s hematocrit (preferably drawn within 24 h of the exam) is known [32, 49].
Active myocarditis with edema in a 17-year-old boy. a Four-chamber T2-weighted double inversion recovery (IR) fast spin-echo MR image shows patchy myocardial edema (arrows). LA left atrium, LV left ventricle, RA right atrium, RV right ventricle. b Four-chamber two-dimensional phase-sensitive IR late-gadolinium-enhancement image shows corresponding areas of abnormal myocardial late enhancement (arrows)
Workflow considerations
With conventional cardiac anatomy, as is often the case with cardiomyopathies, a number of steps in the workflow chain (e.g., plane localization for acquisition, volumetry post-processing, etc.) are relatively similar and repetitive across exams, yet time-consuming to manually perform. Automating (or nearly automating) such processes is now increasingly feasible through the use of AI/deep learning methods, which effectively can “learn” to execute rote tasks from prior data/examples. AI-based vendor solutions for automated ventricular contouring (with expert oversight when needed) are already available with promising results (Fig. 9) [51]. Other works-in-progress include using deep learning for automated cardiac cine scan plane prescription and selection of the optimal TI time for LGE imaging [52, 53]. These applications are likely to increase and to grow more robust in the coming years, allowing for more rapid cardiac MRI acquisition, post-processing and interpretation.
Automated ventricular contouring using deep learning in a 17-year-old boy with a normal cardiac MRI. Screen capture from a commercial cardiac post-processing software package employing deep learning techniques shows extremely accurate ventricular endocardial and epicardial contours (arrows) generated from a short-axis cine balanced steady-state free precession sequence prior to any human adjustment. LV left ventricle, RV right ventricle
Congenital heart disease
Conventional approaches
Congenital heart disease represents an enormous and heterogeneous spectrum of disease that often needs to be interrogated across the lifespan, before and after intervention/surgery, with associated complications. Thus, using conventional techniques, developing an abbreviated yet relatively constant MRI protocol to cover the full range of abnormalities is an immense challenge. A sample conventional congenital protocol with pertinent scan parameters at 1.5 T is shown in Table 2.
As a starting point, in the author’s practice one typically obtains cine imaging, usually bSSFP, in dedicated right ventricular (RV) planes in addition to the previously discussed LV planes (Fig. 10). These include RV 2- and 3-chamber views and a right ventricular outflow tract (RVOT) view. The RV 3-chamber is prescribed to pass through the RV apex and center of the tricuspid and pulmonic valves, akin to the LV 3-chamber. The RV 2-chamber is oriented through the intersection of the 4-chamber and RV 3-chamber prescriptions, akin to the LV 2-chamber. The RVOT view is oriented in the sagittal or oblique sagittal plane through the pulmonary valve [32].
Standard right ventricular (RV) planes in an 18-year-old woman with a history of repaired tetralogy of Fallot, pulmonary atresia and major aortopulmonary collaterals. a–c RV 3-chamber (a), RV 2-chamber (b) and right ventricular outflow tract (RVOT) (c) end-diastolic balanced steady-state free precession MR images show no significant RV dilation. Ao aorta, PA pulmonary artery (main), RA right atrium
Anatomical assessment is a key component of most CHD MRI. This is typically achieved with a contrast-enhanced magnetic resonance (MR) angiography sequence using a 3-D T1-weighted SPGR approach for the shortest imaging time and best delineation of vessels [29, 54]. A sample injection protocol is 0.1–0.2 mmol/kg gadolinium agent, followed by 20 mL saline flush injected at rate of at least 1 mL/s; the contrast agent can also be diluted to prolong the bolus. A test bolus can be used to determine the optimal acquisition timing, or alternatively, dynamic bolus tracking can be utilized [54]. At the author’s institution, a custom ECG-gated and breath-held enhanced 3-D T1 SPGR sequence (“MFAST”) with compressed sensing reconstruction is used; however, a variety of vendor solutions are available [55].
If contrast agent is contraindicated (e.g., allergy, pregnancy, renal insufficiency) or not desired (e.g., concerns about IV line placement or brain deposition of gadolinium), several non-contrast sequences for delineating anatomy are available. Popular among these is a free-breathing ECG-gated and navigator respiratory-gated 3-D SSFP sequence, which is also isotropic, allowing for multiplanar reconstructions [30]. Another option is black blood imaging, as could be achieved with a fast spin-echo double inversion recovery technique, although this option is generally 2-D and thus does not allow for reformats (Fig. 11) [5, 30, 56]. Both of these are generally more time-consuming than contrast-enhanced MR angiography [29].
Comparison of anatomical cardiovascular MRI methods in a 12-year-old boy with Marfan syndrome. a–c Oblique sagittal two-dimensional (2-D) double inversion recovery fast spin-echo (black blood) image (a), oblique sagittal reformat from a non-contrast electrocardiographic (ECG)-gated respiratory-navigated (free-breathing) three-dimensional (3-D) steady-state free precession acquisition (b) and oblique sagittal reformat from a gadolinium-enhanced ECG-gated breath-held MR angiogram with 3-D T1 spoiled gradient echo technique and test bolus timing (c) show dilation of the aortic root (arrow)
The final major component of CHD evaluation is flow imaging. This is conventionally achieved with 2-D phase contrast using an ECG-gated and motion-encoded cine GRE sequence, acquired over multiple heartbeats during a 10–20-s breath-hold, with slice thicknesses 5–8 mm [29,30,31,32, 57]. The acquisition should be prescribed perpendicular in two planes (through-plane encoding) to the anticipated primary blood flow jet along the center of the vessel of interest [32, 57]. The 2-D phase-contrast sequence produces magnitude (anatomical) and phase difference (velocity) images corresponding to changes in appearance of the vessel in cross-section and its blood flow across the cardiac cycle; flow velocities in the main direction of the vessel flow appear as either high or low signal, depending on the vendor, while those in the opposite direction appear as the reverse signal (i.e. low or high, respectively), on the phase difference images [57].
An important operator-designated parameter in 2-D phase-contrast imaging is the velocity encoding sensitivity (VENC), corresponding to the maximum detectable velocity. Setting the VENC too low results in aliasing if the velocities present are higher than the VENC setting (Fig. 12). On the other hand, if the VENC is arbitrarily set high, generalized increased noise appears in the 2-D phase-contrast images, resulting in decreased sensitivity for detecting lower-velocity flow [32, 57]. In CHD, 2-D phase-contrast images are typically obtained at least at the levels of the aortic valve or ascending aorta and pulmonic valve or main pulmonary trunk for calculation the ratio of pulmonary to systemic blood flow (Qp:Qs) [30]. However, depending on the clinical scenario, often other flow measurements are needed (e.g., pulmonary veins in the setting of Fontan physiology, atrioventricular flow for regurgitation, etc.), and given that each 2-D phase-contrast prescription requires localization of the vessel in two orthogonal planes, obtaining these flow measurements can be time-consuming, particularly if the operator is less experienced, the anatomy is unusual or acquisitions need to be repeated because of patient factors (e.g., difficult breath-holding). Deep learning techniques have also recently been used to accelerate 2-D phase-contrast acquisitions [58, 59].
Two-dimensional (2-D) phase-contrast imaging with aliasing in a 13-year-old girl with congenitally corrected transposition of the great arteries post pulmonary artery banding. a Axial magnitude image from a 2-D phase-contrast acquisition shows anatomical narrowing (arrow) at the level of the band. b Corresponding phase velocity image shows central high signal with irregular edges (arrow), indicating aliasing, within the otherwise low signal across the band (flow directed toward the head). The velocity encoding sensitivity (VENC) was set to 3.5 m/s; because aliasing is present, the peak flow across the band must exceed 3.5 m/s
Blood pool contrast agents
Extracellular gadolinium agents are usually the mainstay for post-contrast imaging (e.g., MR angiography). However, these agents, while first taken up into the intravascular space, quickly equilibrate with the extracellular space, with half-life eliminations in the range of 70–90 min [5]. Thus, there is a limited time window for optimally evaluating the vessels of interest, presenting a challenge in the less experienced operator or patient with breath-holding difficulty, etc. [5, 54]. In addition to extracellular gadolinium agents are blood pool intravascular contrast agents that have high molecular weight and affinity for albumin, resulting in prolonged vascular signal and thus flexibility to perform multiple repeats, utilize lower contrast doses, and achieve higher spatial resolution [54].
Popular among the blood pool agents was gadofosveset, providing adequate vascular signal for approximately 45–60 min after administration; however, this agent can no longer be purchased in the United States (U.S.) and thus is not available for routine clinical purposes [5]. As such, there has been growing use of the ultrasmall paramagnetic iron oxide (USPIO) nanoparticle ferumoxytol, in fact designed as a medication to treat iron deficiency anemia, as an off-label blood pool imaging agent. Due to its large size, this molecule has little extravascular leakage, with a circulating half-life of 14–15 h, even affecting MRI signal for days to months after administration [5, 54]. In addition, because it is not renal excreted, it can be safely given to patients with renal disease [5]. For vascular imaging, the agent is typically administered slowly over 5–15 min, diluted in normal saline (3 mg/kg with 1:5 dilution or 0.1 mL/kg) [60,61,62]. Of note, the risk of adverse reactions with ferumoxytol is likely higher than that of gadolinium-based agents, and the agent carries a black box U.S. Food and Drug Administration warning indicating the potential for rare but significant acute hypersensitivity reactions [46, 55]. However, in a recent multicenter study, the rate of adverse events was low (< 2%) and most events were minor [63]. Nevertheless, due to potential for hypotension, vital signs are typically monitored for 30 min after administration by personnel with advanced cardiac or pediatric life support training [62]. Other downsides to ferumoxytol include its greater cost compared to gadolinium-based agents and compromised ability to separate arterial and venous phases given that it is usually not bolus-injected for safety reasons [54, 62].
Four-dimensional flow acquisition
As previously described, the time-consuming nature of prescribing multiple 2-D phase-contrast acquisitions has traditionally been a limitation of CHD MRI. However, the advent of 4-D flow has helped revolutionize the state of imaging [5]. Four-dimensional flow is typically achieved with a retrospectively ECG-gated, respiratory navigator-gated or free-breathing 3-D cine SPGR sequence utilizing short echo times (TE) in the range of 2–4 ms and short repetition times (TR) in the range of 5–7 ms [5, 60, 63]. The acquisition is prescribed as a volume over a region of interest (such as the heart or chest), usually in 5–15 min, and yields 4 time-resolved 3-D datasets corresponding to a magnitude (anatomy) dataset and 3 flow datasets corresponding to velocities in all 3 orthogonal directions (x, y, z) [5, 57, 64]. No detailed knowledge of the anatomy or complex scan plane prescriptions is required. Intravenous contrast agent is not absolutely necessary but improves SNR in the magnitude data and decreases noise in the velocity data [64]. Because of its long half-life, pre-administration of ferumoxytol is particularly advantageous, although gadolinium-based agents can also be used [5]. Using post-processing software, retrospectively, the anatomy can then be viewed in any plane via the cine magnitude data and blood flow quantified via the reconstructed cine velocity data [5, 57].
There are several considerations in implementing 4-D flow. Four-dimensional flow sequences and post-processing visualization software were once limited to local research initiatives; however, they are now increasingly available from commercial vendors [24, 57]. Given the large nature of the datasets and need to perform pre-processing error corrections, 4-D flow reconstruction times can be long, on the order of hours. Thus, images are not available immediately after acquisition, which can be an important consideration for workflow and real-time quality assurance, although reconstruction times continue to decrease [5]. Finally, as in 2-D phase contrast, the VENC must be prospectively set but in all three directions. Because images are not available instantaneously, it can be challenging to prospectively gauge the lowest VENC that will not result in aliasing in the areas of interest. Strategies to overcome this include running the 4-D flow acquisition at different VENCs (at substantial time cost) or using an interleaved multi-VENC acquisition (at lesser time cost). More recent ongoing work centers on using velocity unwrapping techniques to retrospectively de-alias 4-D datasets with associated time savings [65]. At the author’s institution, typical 4-D flow VENC settings (in all three directions) are in the range of 250–350 cm/s.
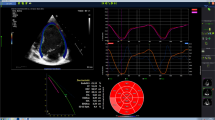
Newer protocol approach to congenital heart disease
Considering the advances noted here, the author’s institution has in recent years adopted a single-sequence approach to CHD in many circumstances, consisting of pre-scan administration of ferumoxytol followed by a 4-D flow acquisition, with retrospective analysis. Several studies have demonstrated good concordance (1) between volumetry and mass measurements obtained with 4-D flow magnitude data, and cine bSSFP sequences; and (2) between 4-D flow and 2-D phase-contrast flow and velocity estimates [61, 66, 67]. Quantitative volumetry and flow measurements between 4-D flow and conventional techniques have also been shown to be relatively similar when using gadolinium-based agents at 1.5 T [68]. Four-dimensional flow can be supplemented with an MR angiography/anatomy sequence if the magnitude data (e.g., from an uncustomized commercial product) are insufficient. Because the lungs and airways might be of concurrent concern, a 3-D T1-weighted ultrashort echo time (UTE) or zero echo time (ZTE) sequence could also be considered if available (although these are not yet widely commercially distributed) (Fig. 13; Online Supplementary Material 1) [62]. If a combined assessment for CHD and LGE/tissue characterization is needed, an abbreviated gadolinium-enhanced 4-D flow sequence (e.g., with fewer phases, decreased resolution, etc.) can be prescribed so that LGE commences relatively immediately after the termination of 4-D flow. Combined blood pool and extracellular contrast agents are another option but with potentially increased administration and scan time [69].
Abbreviated ferumoxytol/four-dimensional (4-D) flow congenital cardiac MRI protocol with the addition of ultrashort echo time (UTE) imaging in a 4-day-old boy with double outlet right ventricle. a Oblique sagittal reformatted image from a free-breathing, unsedated isotropic 4-D flow acquisition shows the abnormal egress of both the aorta (Ao) and main pulmonary artery (PA) from the right ventricle (RV). There is subaortic conus (arrow) causing stenosis. See Online Supplementary Material 1 for full 4-D flow video. b Four-dimensional flow image retrospectively reformatted orthogonal to the PA allows quantitative measurement of PA flow curve (arrow). c Retrospectively reformatted short-axis image allows contouring (arrows) of the left ventricle (LV) and RV with associated quantitative volumetry data (right). d Axial UTE image in the same boy (separate acquisition) provides improved delineation of the lungs and airways (arrows)
Conclusion
With modern techniques, comprehensive yet compact cardiac MRI in children is now a clinical reality for many indications. Careful preparation and consideration of the exam indications (e.g., cardiomyopathy vs. CHD) are paramount to success. The use of flexible coils can provide both improved image quality and a better patient experience. Compressed sensing and deep learning techniques are increasingly available to assist with faster image acquisition (e.g., for 2-D cine bSSFP and phase contrast) as well as workflow elements (e.g., scan plane prescription, post-processing). PSIR methods can help improve the consistency of LGE, especially in less experienced operators. Finally, single-sequence CHD imaging is now possible using 4-D flow, particularly when enhanced with ferumoxytol, although post-gadolinium 4-D flow can be effectively combined with LGE if needed. As cardiac MRI methods continue to advance, the opportunities to achieve rapid and compact yet still comprehensive exams in children should only continue to increase.
References
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Lipshultz SE, Law YM, Asante-Korang A et al (2019) Cardiomyopathy in children: classification and diagnosis: a scientific statement from the American Heart Association. Circulation 140:e9–e68
Truong UT, Kutty S, Broberg CS, Sahn DJ (2012) Multimodality imaging in congenital heart disease: an update. Curr Cardiovasc Imaging Rep 5:481–490
Opfer E, Shah S (2018) Advances in pediatric cardiovascular imaging. Mo Med 115:354–360
Zucker EJ, Koning JL, Lee EY (2017) Cyanotic congenital heart disease: essential primer for the practicing radiologist. Radiol Clin North Am 55:693–716
Banka P, Geva T (2016) Advances in pediatric cardiac MRI. Curr Opin Pediatr 28:575–583
Bailliard F, Hughes ML, Taylor AM (2008) Introduction to cardiac imaging in infants and children: techniques, potential, and role in the imaging work-up of various cardiac malformations and other pediatric heart conditions. Eur J Radiol 68:191–198
Chan FP, Hanneman K (2015) Computed tomography and magnetic resonance imaging in neonates with congenital cardiovascular disease. Semin Ultrasound CT MR 36:146–160
Mitchell FM, Prasad SK, Greil GF et al (2016) Cardiovascular magnetic resonance: diagnostic utility and specific considerations in the pediatric population. World J Clin Pediatr 5:1–15
Kinnebrew SL, Dove CG, Midwin CM et al (2020) The role of child life in pediatric radiology. Pediatr Radiol 50:1509–1513
Tseng WY, Su MY, Tseng YH (2016) Introduction to cardiovascular magnetic resonance: technical principles and clinical applications. Acta Cardiol Sin 32:129–144
Moghari MH, Chan RH, Hong SN et al (2012) Free-breathing cardiac MR with a fixed navigator efficiency using adaptive gating window size. Magn Reson Med 68:1866–1875
Zaitsev M, Maclaren J, Herbst M (2015) Motion artifacts in MRI: a complex problem with many partial solutions. J Magn Reson Imaging 42:887–890
Lee VS, Hecht EM, Taouli B et al (2007) Body and cardiovascular MR imaging at 3.0 T. Radiology 244:692–705
Oshinski JN, Delfino JG, Sharma P et al (2010) Cardiovascular magnetic resonance at 3.0 T: current state of the art. J Cardiovasc Magn Reson 12:55
Willinek WA, Schild HH (2008) Clinical advantages of 3.0 T MRI over 1.5 T. Eur J Radiol 65:2–14
Muthalaly RG, Nerlekar N, Ge Y et al (2007) MRI in patients with cardiac implantable electronic devices. Radiology 289:281–292
Indik JH, Gimbel JR, Abe H et al (2017) 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm 14:e97–e153
Glikson M, Nielsen JC, Kronborg MB et al (2021) ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 42:3427–3520
Klein-Wiele O, Garmer M, Busch M et al (2017) Cardiovascular magnetic resonance in patients with magnetic resonance conditional pacemaker systems at 1.5 T: influence of pacemaker related artifacts on image quality including first pass perfusion, aortic and mitral valve assessment, flow measurement, short tau inversion recovery and T1-weighted imaging. Int J Cardiovasc Imaging 33:383–394
Kaasalainen T, Kivistö S, Holmström M et al (2016) Cardiac MRI in patients with cardiac pacemakers: practical methods for reducing susceptibility artifacts and optimizing image quality. Acta Radiol 57:178–187
Giovannetti G, De Marchi D, Pingitore A (2016) Radiofrequency coils and pulse sequences for cardiac magnetic resonance applications: new perspectives and future developments. Rev Cardiovasc Med 17:124–130
Deshmane A, Gulani V, Griswold MA, Seiberlich N (2012) Parallel MR imaging. J Magn Reson Imaging 36:55–72
Blamire AM (2008) The technology of MRI — the next 10 years? Br J Radiol 81:601–617
Winkler SA, Corea J, Lechêne B et al (2019) Evaluation of a flexible 12-channel screen-printed pediatric MRI coil. Radiology 291:180–185
McGee KP, Stormont RS, Lindsay SA et al (2018) Characterization and evaluation of a flexible MRI receive coil array for radiation therapy MR treatment planning using highly decoupled RF circuits. Phys Med Biol 63:8
Cogswell PM, Trzasko JD, Gray EM et al (2020) Application of adaptive image receive coil technology for whole-brain imaging. AJR Am J Roentgenol 216:552–559
Dickstein K (2008) Clinical utilities of cardiac MRI. European Society of Cardiology Council for Cardiology Practice e-journal. https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-6/Clinical-Utilities-of-cardiac-MRI. Accessed 15 Jun 2022
Situ Y, Birch SCM, Moreyra C, Holloway CJ (2020) Cardiovascular magnetic resonance imaging for structural heart disease. Cardiovasc Diagn Ther 10:361–375
Krishnamurthy R (2008) Pediatric cardiac MRI: anatomy and function. Pediatr Radiol 38:S192–S199
Helbing WA, Ouhlous M (2015) Cardiac magnetic resonance imaging in children. Pediatr Radiol 45:20–26
Kramer CM, Barkhausen J, Bucciarelli-Ducci C et al (2020) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 22:17
Saremi F, Grizzard JD, Kim RJ (2008) Optimizing cardiac MR imaging: practical remedies for artifacts. Radiographics 28:1161–1168
Chandrasekar H, Kaufman BD, Vasanawala S et al (2021) Abstract 10639: abbreviated cardiac magnetic resonance imaging versus echocardiography for interval assessment of systolic function in Duchenne muscular dystrophy: patient satisfaction, clinical utility and image quality. Circulation 144:A10639
Feng L, Benkert T, Block KT et al (2017) Compressed sensing for body MRI. J Magn Reson Imaging 45:966–987
Kocaoglu M, Pednekar AS, Wang H et al (2020) Breath-hold and free-breathing quantitative assessment of biventricular volume and function using compressed SENSE: a clinical validation in children and young adults. J Cardiovasc Magn Reson 22:54
Naresh NK, Malone L, Fujiwara T et al (2021) Use of compressed sensing to reduce scan time and breath-holding for cardiac cine balanced steady-state free precession magnetic resonance imaging in children and young adults. Pediatr Radiol 51:1192–1201
Masutani EM, Bahrami N, Hsiao A (2020) Deep learning single-frame and multiframe super-resolution for cardiac MRI. Radiology 295:552–561
Sandino CM, Lai P, Vasanawala SS, Cheng JY (2021) Accelerating cardiac cine MRI using a deep learning-based ESPIRiT reconstruction. Magn Reson Med 85:152–167
Zucker EJ, Sandino CM, Kino A et al (2021) Free-breathing accelerated cardiac MRI using deep learning: validation in children and young adults. Radiology 300:539–554
Lustig M, Pauly JM (2010) SPIRiT: iterative self-consistent parallel imaging reconstruction from arbitrary k-space. Magn Reson Med 64:457–471
Uecker M, Lai P, Murphy MJ et al (2014) ESPIRiT — an eigenvalue approach to autocalibrating parallel MRI: where SENSE meets GRAPPA. Magn Reson Med 71:990–1001
Ryu K, Sandino CM, Li Z et al (2021) Improving deep unrolled neural networks for radial cine cardiac image reconstruction using memory-efficient training, Conv-LSTM based network. International Society for Magnetic Resonance in Medicine (ISMRM) 29th annual meeting, 19 May 2021. https://www.ismrm.org/21/program-files/TeaserSlides/TeasersPresentations/0447-Teaser.html
Menchón-Lara RM, Simmross-Wattenberg F, Casaseca-de-la-Higuera P et al (2019) Reconstruction techniques for cardiac cine MRI. Insights Imaging 10:100
Antun V, Renna F, Poon C et al (2020) On instabilities of deep learning in image reconstruction and the potential costs of AI. Proc Natl Acad Sci U S A 117:30088–30095
Kellman P, Arai AE (2012) Cardiac imaging techniques for physicians: late enhancement. J Magn Reson Imaging 36:529–542
Viallon M, Jacquier A, Rotaru C et al (2011) Head-to-head comparison of eight late gadolinium-enhanced cardiac MR (LGE CMR) sequences at 1.5 tesla: from bench to bedside. J Magn Reson Imaging 34:1374–1387
van der Velde N, Hassing HC, Bakker BJ et al (2021) Improvement of late gadolinium enhancement image quality using a deep learning-based reconstruction algorithm and its influence on myocardial scar quantification. Eur Radiol 31:3846–3855
Burt JR, Zimmerman SL, Kamel IR et al (2014) Myocardial T1 mapping: techniques and potential applications. Radiographics 34:377–379
Captur G, Bhandari A, Brühl R et al (2020) T1 mapping performance and measurement repeatability: results from the multi-national T1 mapping standardization phantom program (T1MES). J Cardiovasc Magn Reson 22:31
Retson TA, Masutani EM, Golden D, Hsiao A (2020) Clinical performance and role of expert supervision of deep learning for cardiac ventricular volumetry: a validation study. Radiol Artif Intell 2:e190064
Blansit K, Retson T, Masutani E et al (2019) Deep learning-based prescription of cardiac MRI planes. Radiol Artif Intell 1:e180069
Bahrami N, Retson T, Blansit K et al (2019) Automated selection of myocardial inversion time with a convolutional neural network: spatial temporal ensemble myocardium inversion network (STEMI-NET). Magn Reson Med 81:3283–3291
Aziz M, Krishnam M, Madhuranthakam AJ, Rajiah P (2019) Update on MR imaging of the pulmonary vasculature. Int J Cardiovasc Imaging 35:1483–1497
Alley M (2022) Lucas Center research MRI: research imaging sequences: ‘mfast’ & ‘mm4dflow.’ Lucas MRI Service Center website. https://med.stanford.edu/lucasmri/research-psds.html. Accessed 1 Apr 2022
Henningsson M, Malik S, Botnar R et al (2022) Black-blood contrast in cardiovascular MRI. J Magn Reson Imaging 55:61–80
Stankovic Z, Allen BD, Garcia J et al (2014) 4D flow imaging with MRI. Cardiovasc Diagn Ther 4:173–192
Middione MJ, Oscanoa JA, Loecher M et al (2021) Deep learning-based ESPIRiT reconstruction for accelerated 2D phase contrast MRI: analysis of the impact of reconstruction induced phase errors. International Society for Magnetic Resonance in Medicine (ISMRM) 29th annual meeting, 19 May 2021. https://www.ismrm.org/21/program-files/TeaserSlides/TeasersPresentations/2658-Teaser.html
Warren JA, Middione MJ, Oscanoa JA et al (2021) Cross validation of a deep learning-based ESPIRiT reconstruction for accelerated 2D phase contrast MRI. International Society for Magnetic Resonance in Medicine (ISMRM) 29th annual meeting, 19 May 2021. https://www.ismrm.org/21/program-files/TeaserSlides/TeasersPresentations/2644-Teaser.html
Vasanawala SS, Nguyen KL, Hope MD et al (2016) Safety and technique of ferumoxytol administration for MRI. Magn Reson Med 75:2107–2111
Hanneman K, Kino A, Cheng JY et al (2016) Assessment of the precision and reproducibility of ventricular volume, function, and mass measurements with ferumoxytol-enhanced 4D flow MRI. J Magn Reson Imaging 44:383–392
Zucker EJ, Cheng JY, Haldipur A et al (2018) Free-breathing pediatric chest MRI: performance of self-navigated golden-angle ordered conical ultrashort echo time acquisition. J Magn Reson Imaging 47:200–209
Nguyen KL, Yoshida T, Kathuria-Prakash N et al (2019) Multicenter safety and practice for off-label diagnostic use of ferumoxytol in MRI. Radiology 293:554–564
Azarine A, Garçon P, Stansal A et al (2019) Four-dimensional flow MRI: principles and cardiovascular applications. Radiographics 39:632–648
Ma LE, Markl M, Chow K et al (2020) Efficient triple-VENC phase-contrast MRI for improved velocity dynamic range. Magn Reson Med 83:505–520
Feneis JF, Kyubwa E, Atianzar K et al (2018) 4D flow MRI quantification of mitral and tricuspid regurgitation: reproducibility and consistency relative to conventional MRI. J Magn Reson Imaging 48:1147–1158
Gabbour M, Schnell S, Jarvis K et al (2015) 4-D flow magnetic resonance imaging: blood flow quantification compared to 2-D phase-contrast magnetic resonance imaging and Doppler echocardiography. Pediatr Radiol 45:804–813
Jacobs KG, Chan FP, Cheng JY et al (2020) 4D flow vs. 2D cardiac MRI for the evaluation of pulmonary regurgitation and ventricular volume in repaired tetralogy of Fallot: a retrospective case control study. Int J Cardiovasc Imaging 36:657–669
Johnson JT, Robinson JD, Deng J, Rigsby CK (2016) Combined blood pool and extracellular contrast agents for pediatric and young adult cardiovascular magnetic resonance imaging. Pediatr Radiol 46:1822–1830
Acknowledgments
Portions of this work were presented at the Society for Pediatric Radiology (SPR) 2022 Improving Protocols course.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviated ferumoxytol/four-dimensional (4-D) flow cardiac MRI protocol in a 4-day-old boy with double outlet right ventricle (same boy and exam as in Fig. 13). Oblique sagittal reformatted cine images from a free-breathing, unsedated isotropic 4-D flow acquisition show the abnormal egress of both the aorta (Ao) and the main pulmonary artery (PA) from the right ventricle (RV). There is subaortic conus (arrow) causing stenosis. (MP4 1.89 MB)
Rights and permissions
About this article
Cite this article
Zucker, E.J. Compact pediatric cardiac magnetic resonance imaging protocols. Pediatr Radiol 53, 1336–1351 (2023). https://doi.org/10.1007/s00247-022-05447-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05447-y