Abstract
Purpose
PSMA-targeted PET in patients with prostate cancer (PCa) has a significant impact on treatment decisions. By far the most frequently used PSMA ligand is 68Ga-labelled PSMA-11. However, due to the availability of larger amounts of activity, 18F-labelled PSMA ligands are of major interest. The aim of the present study was to evaluate the biodistribution and performance of the novel 18F-labelled ligand PSMA-1007 at two different time points.
Methods
This retrospective analysis included 40 consecutive patients (mean age 68.7 ± 8.1 years) referred for PSMA PET/CT. 18F-PSMA-1007 PET/CT was performed for localization of biochemical relapse, primary staging or therapy follow-up. Circular regions of interest were placed on representative slices of the liver, spleen, kidney, abdominal aortic blood pool, bone marrow (fourth lumbar vertebral body), urinary bladder and gluteus muscle at 60 and 120 min after injection. In malignant lesions the maximum standardized uptake (SUVmax) was measured within volumes of interest at both time points. All SUVs at 60 min were compared with those at 120 min after injection.
Results
The activity in the blood pool, urinary bladder and gluteus muscle was very low and decreased significantly over time (P < 0.001). Uptake in the liver, spleen and kidney showed a significant increase over time and uptake in the bone marrow remained stable. Overall, 135 PCa lesions were detected at 60 min and 136 lesions at 120 min after injection. The median SUVmax increased significantly (P < 0.001) from 10.98 to 15.51 between 60 and 120 min.
Conclusion
PCa lesions show a significant increase in 18F-PSMA-1007 uptake at 120 min compared with 60 min after injection. In addition, accumulation of the tracer in the urinary bladder was very low leading to improved contrast of adjacent PCa lesions. Increasing accumulation in the liver may limit the sensitivity of the tracer in detecting liver metastases.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. https://doi.org/10.3322/caac.21254.
Israeli RS, Powell CT, Corr JG, Fair WR, Heston WD. Expression of the prostate-specific membrane antigen. Cancer Res. 1994;54(7):1807–11.
Sweat SD, Pacelli A, Murphy GP, Bostwick DG. Prostate-specific membrane antigen expression is greatest in prostate adenocarcinoma and lymph node metastases. Urology. 1998;52(4):637–40.
Wright GL Jr, Grob BM, Haley C, Grossman K, Newhall K, Petrylak D, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48(2):326–34.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(4):486–95. https://doi.org/10.1007/s00259-012-2298-2.
Sheikhbahaei S, Afshar-Oromieh A, Eiber M, Solnes LB, Javadi MS, Ross AE, et al. Pearls and pitfalls in clinical interpretation of prostate-specific membrane antigen (PSMA)-targeted PET imaging. Eur J Nucl Med Mol Imaging. 2017;44(12):2117–36. https://doi.org/10.1007/s00259-017-3780-7.
Backhaus P, Noto B, Avramovic N, Grubert LS, Huss S, Bogemann M, et al. Targeting PSMA by radioligands in non-prostate disease-current status and future perspectives. Eur J Nucl Med Mol Imaging. 2018. https://doi.org/10.1007/s00259-017-3922-y.
Afshar-Oromieh A, Holland-Letz T, Giesel FL, Kratochwil C, Mier W, Haufe S, et al. Diagnostic performance of 68Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients. Eur J Nucl Med Mol Imaging. 2017;44(8):1258–68. https://doi.org/10.1007/s00259-017-3711-7.
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42(2):197–209. https://doi.org/10.1007/s00259-014-2949-6.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56(5):668–74. https://doi.org/10.2967/jnumed.115.154153.
Rahbar K, Weckesser M, Huss S, Semjonow A, Breyholz HJ, Schrader AJ, et al. Correlation of intraprostatic tumor extent with 68Ga-PSMA distribution in patients with prostate cancer. J Nucl Med. 2016;57(4):563–7. https://doi.org/10.2967/jnumed.115.169243.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41(1):11–20. https://doi.org/10.1007/s00259-013-2525-5.
Mease RC, Dusich CL, Foss CA, Ravert HT, Dannals RF, Seidel J, et al. N-[N-[(S)-1,3-Dicarboxypropyl]carbamoyl]-4-[18F]fluorobenzyl-L-cysteine, [18F]DCFBC: a new imaging probe for prostate cancer. Clin Cancer Res. 2008;14(10):3036–43. https://doi.org/10.1158/1078-0432.CCR-07-1517.
Szabo Z, Mena E, Rowe SP, Plyku D, Nidal R, Eisenberger MA, et al. Initial evaluation of [(18)F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol. 2015;17(4):565–74. https://doi.org/10.1007/s11307-015-0850-8.
Giesel FL, Kesch C, Yun M, Cardinale J, Haberkorn U, Kopka K, et al. 18F-PSMA-1007 PET/CT detects micrometastases in a patient with biochemically recurrent prostate cancer. Clin Genitourin Cancer. 2017;15(3):e497–9. https://doi.org/10.1016/j.clgc.2016.12.029.
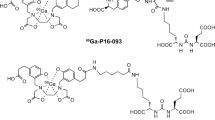
Cardinale J, Schafer M, Benesova M, Bauder-Wust U, Leotta K, Eder M, et al. Preclinical evaluation of 18F-PSMA-1007, a new prostate-specific membrane antigen ligand for prostate cancer imaging. J Nucl Med. 2017;58(3):425–31. https://doi.org/10.2967/jnumed.116.181768.
Afshar-Oromieh A, Hetzheim H, Kratochwil C, Benesova M, Eder M, Neels OC, et al. The theranostic PSMA ligand PSMA-617 in the diagnosis of prostate cancer by PET/CT: biodistribution in humans, radiation dosimetry, and first evaluation of tumor lesions. J Nucl Med. 2015;56(11):1697–705. https://doi.org/10.2967/jnumed.115.161299.
Rahbar K, Weckesser M, Ahmadzadehfar H, Schafers M, Stegger L, Bogemann M. Advantage of (18)F-PSMA-1007 over (68)Ga-PSMA-11 PET imaging for differentiation of local recurrence vs. urinary tracer excretion. Eur J Nucl Med Mol Imaging. 2018; https://doi.org/10.1007/s00259-018-3952-0.
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2017;44(4):678–88. https://doi.org/10.1007/s00259-016-3573-4.
Afshar-Oromieh A, Hetzheim H, Kubler W, Kratochwil C, Giesel FL, Hope TA, et al. Radiation dosimetry of (68)Ga-PSMA-11 (HBED-CC) and preliminary evaluation of optimal imaging timing. Eur J Nucl Med Mol Imaging. 2016;43(9):1611–20. https://doi.org/10.1007/s00259-016-3419-0.
Afshar-Oromieh A, Sattler LP, Mier W, Hadaschik BA, Debus J, Holland-Letz T, et al. The clinical impact of additional late PET/CT imaging with 68Ga-PSMA-11 (HBED-CC) in the diagnosis of prostate cancer. J Nucl Med. 2017;58(5):750–5. https://doi.org/10.2967/jnumed.116.183483.
Herrmann K, Bluemel C, Weineisen M, Schottelius M, Wester HJ, Czernin J, et al. Biodistribution and radiation dosimetry for a probe targeting prostate-specific membrane antigen for imaging and therapy. J Nucl Med. 2015;56(6):855–61. https://doi.org/10.2967/jnumed.115.156133.
Acknowledgments
We thank the Radiochemistry Group at the Department of Nuclear Medicine for their highly reliable production of 18F-PSMA-1007, as well as the technologists for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The University of Münster received consulting fees from ABX GmbH, Radeberg, Germany for K.R. and M.B. Additionally K.R. is scientific consultant/advisor of ABX GmbH. The authors declare they have no conflict of interest according to the subject and matter of the present article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This article does not describe any studies with animals performed by any of the authors. According to data protection guidelines, formal ethical approval for retrospective studies is not necessary.
Rights and permissions
About this article
Cite this article
Rahbar, K., Afshar-Oromieh, A., Bögemann, M. et al. 18F-PSMA-1007 PET/CT at 60 and 120 minutes in patients with prostate cancer: biodistribution, tumour detection and activity kinetics. Eur J Nucl Med Mol Imaging 45, 1329–1334 (2018). https://doi.org/10.1007/s00259-018-3989-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-3989-0