Abstract
Objective
A complete toxicity profile, toxicity profile, and safety ranking of immune checkpoint inhibitors (ICIs) for treatment of advanced non-small cell lung cancer (NSCLC) will be provided in this network meta-analysis.
Methods
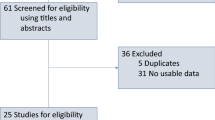
We searched 14 randomized clinical trials (RCTs) including 9572 NSCLC patients by PubMed, EMBASE, Cochrane, and ClinicalTrials.gov. Randomized pairwise and network meta-analyses were used to compare the incidence of severe immune-related adverse events (irAEs) across different ICIs-based treatments using risk ratios (RRs) and 95% confidence intervals (CI).
Results
For severe dermatologic irAEs, the corresponding ranking of incidences of the nine groups from high to low was: nivolumab + ipilimumab + platinum (79.1%), pembrolizumab (75.2%), nivolumab + ipilimumab (72.9%), camrelizumab + platinum (64.9%), atezolizumab + platinum (47.4%), nivolumab (44.2%), durvalumab (40.5%), pembrolizumab + platinum (15.5%), platinum-based chemotherapy (10.3%). For severe colitis, the corresponding ranking of incidences of the seven groups from high to low was: nivolumab + ipilimumab + platinum (72.4%), nivolumab (63.1%), atezolizumab + platinum (56.9%), durvalumab (56.6%), pembrolizumab (54.9%), pembrolizumab + platinum (38.6%), platinum-based chemotherapy (7.4%). For severe endocrine irAEs, the corresponding ranking of incidences of the nine groups from high to low was: durvalumab (74.3%), atezolizumab + platinum (54.5%), nivolumab + ipilimumab (54.0%), camrelizumab + platinum (51.7%), nivolumab + ipilimumab + platinum (51.6%), pembrolizumab + platinum (49.8%), pembrolizumab (49.2%), nivolumab (46.3%), platinum-based chemotherapy (18.6%). For severe pneumonitis, the corresponding ranking of incidences of the nine groups from high to low was: nivolumab (84.3%), pembrolizumab (84.1%), durvalumab (66.1%), camrelizumab + platinum (61.4%), atezolizumab + platinum (50%), pembrolizumab + platinum (43.4%), platinum-based chemotherapy (16.2%), atezolizumab (6.2%). For severe hepatitis, the corresponding ranking of incidences of the eight groups from high to low was: pembrolizumab (68.8%), nivolumab + ipilimumab + platinum (65%), pembrolizumab + platinum (64.6%), durvalumab (57.9%), nivolumab (47.1%), atezolizumab + platinum (43.4%), camrelizumab + platinum (42%), platinum-based chemotherapy (11.2%).
Conclusions
In addition to platinum-based chemotherapy, pembrolizumab + platinum for severe dermatologic irAEs and colitis, nivolumab for severe endocrine irAEs, atezolizumab for severe pneumonitis, camrelizumab + platinum for severe hepatitis may be associated with lower rates of irAEs than other immune-based regimens.






Similar content being viewed by others
Availability of data and material
The data of this paper came from articles of various large RCTs and Clinical Trails.gov. I’m ready to provide the data if needed.
Code availability
Stata13.0, R (version 4.0.1) (CoreTeam 2019, Vienna, Austria) and JAGS (version 4.3.0).
Abbreviations
- 95% CI:
-
95% Confidence interval
- CTLA4:
-
Cytotoxic T lymphocyte-associated antigen-4
- ICI:
-
Immune checkpoint inhibitor
- ICIs:
-
Immune checkpoint inhibitors
- irAEs:
-
Immune-related adverse events
- MCMC:
-
Markov chain Monte Carlo
- NMA:
-
Network meta-analysis
- NSCLC:
-
Non-small cell lung cancer
- PD-1:
-
Programmed cell death receptor 1
- PD-L1:
-
Programmed cell death ligand-1
- PD-L2:
-
Programmed cell death ligand-2
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
- RCTs:
-
Randomized clinical trials
- RRs:
-
Risk ratios
- SUCRA:
-
Surface under the cumulative ranking curve
References
World Health Organization (2018) Cancer fact sheet. https://www.who.int/news-room/fact-sheets/detail/cancer
Goldstraw P, Chansky K, Crowley J (2016) The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11(1):39–51
Torre L, Siegel R, Jemal A (2016) Lung cancer statistics. Adv Exp Med Biol 893:1–19
Molina J, Yang R, Cassivi P et al (2008) Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin 83:584–594
Bironzo P, Di M (2018) A review of guidelines for lung cancer. J Thorac Dis 10(Suppl. 13):S1556–S1663
Lindeman NI et al (2013) Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol 8:823–859
Khozin S et al (2014) U.S. Food and Drug Administration approval summary: erlotinib for the first-line treatment of metastatic non-small cell lung cancer with epidermal growth factor receptor exon 19 deletions or exon 21 (L858R) substitution mutations. Oncologist 19:774–779
Boumahdi S, de Sauvage FJ (2020) The great escape: tumour cell plasticity in resistance to targeted therapy. Nat Rev Drug Discov 19:39–56
Sandler A, Gray R, Perry MC et al (2006) Paclitaxel–carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355:2542–2550
Scagliotti, Parikh, Pawel et al (2008) Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 26:3543–3551
Ettinger, Wood, Aisner et al (2017) Non-small cell lung cancer, Version 5.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:504–535
Pedoeem A, Azoulay AI, Strazza M et al (2014) Programmed death-1 pathway in cancer and autoimmunity. Clin Immunol 153(1):145–152
Carbone DP, Reck M, Paz-Ares L (2017) First-line Nivolumab in stage IV or recurrent non–small-cell lung cancer. N Engl J Med 376:2415–2426
Naiyer A, Byoung C, Niels R (2020) Durvalumab with or without tremelimumab versus standard chemotherapy in first-line treatment of metastatic non–small cell lung cancer. JAMA Oncol 6(5):237–251
Paz-Ares L, Luft A, Vicente D (2018) Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med 379:2040–2051
Gandhi L, Rodríguez-Abreu D, Gadgeel S (2018) Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378:2078–2092
Tony SK, Yi-Long W, Iveta K (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. The Lancet 6736:32409–32421
Reck M, Rodríguez-Abreu D (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375:1823–1833
Corey JL, Shirish MG, Hossein B (2016) Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. The Lancet 17(11):30498–30510
Barlesi F, Nishio M, Cobo M (2018) Efficacy of atezolizumab (atezo) 1 carboplatin (carbo)/cisplatin (cis) 1 pemetrexed (pem) as 1L treatment in key subgroups with stage IV non-squamous non-small cell lung cancer (NSCLC). Ann Oncol 29:743–744
Robert J, Federico C, Ihor V (2020) Atezolizumab in combination with carboplatin and nab-paclitaxel in advanced squamous NSCLC (IMpower131): results from a randomized phase III trial. J Thorac Oncol 3:28–38
Howard W, Michael M, Maen H (2019) Atezolizumab in combination with carboplatin plusnab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 20:924–937
Roy SH, Giuseppe G, Filippo DM (2020) Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med 383:1328–1339
Hellmann MD, Paz-Ares L, Bernabe R (2019) Nivolumab plus ipilimumab in advanced non-small-cell lung cancer. N Engl J Med 381:2020–2031
Zhou C, Chen G, Huang Y (2020) Camrelizumab plus carboplatin and pemetrexed versus chemotherapy alone in chemotherapy-naive patients with advanced non-squamous non-small-cell lung cancer (CameL): a randomised, open-label, multicentre, phase 3 trial. Lancet Respir Med 12:18
Paz-Ares L, Ciuleanu T-E, Cobo M (2021) First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol 22:198–211
Postow MA, Sidlow R, Hellmann MD (2018) Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 378:158–168
Greten TF, Sangro B (2017) Targets for immunotherapy of liver cancer. J Hepatol 68:157–166
Wang P-F, Chen Y, Song S-Y, Wang T-J, Ji W-J, Li S-W et al (2017) Immune-related adverse events associated with anti-PD-1/PD-L1 treatment for malignancies: a meta-analysis. Front Pharmacol 8
Remon J, Passiglia F, Ahn M-J et al (2020) Immune checkpoint inhibitors in thoracic malignancies: review of the existing evidence by an IASLC expert panel and recommendations. J Thorac Oncol 15:914–947
Wang DY, Salem JE, Cohen JV et al (2018) Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 4:1721–1728
National Cancer Institute (2019) Common Terminology Criteria for Adverse Events (CTCAE) v5.0. Updated May27, 2017. Accessed 12 July 2019
Wang Y, Zhou S, Yang F et al (2019) Treatment-related adverse events of PD-1 and PD-L1 inhibitors in clinical trials: a systematic review and meta analysis. JAMA Oncol 5:1008e1019
Chen TW, Razak AR, Bedard PL et al (2015) A systematic review of immune-related adverse event reporting in clinical trials of immune checkpoint inhibitors. Ann Oncol 00:1–6
Weber J, Thompson JA, Hamid O (2009) A randomized, double-blind, placebo-controlled, phase II study comparing the tolerability and efficacy of ipilimumab administered with or without prophylactic budesonide in patients with unresectable Stage III or IV melanoma. Clin Cancer Res 15(17):5591–5598
Liberati A, Altman DG, Tetzlaff J (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Hutton B, Salanti G, Caldwell DM (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162:777–784
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions Version 5.1. 0. The Cochrane Collaboration. Confidence intervals
Basch, Iasonos, McDonough (2016) Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol 7(11):903–909
Salanti G, Higgins JPT, Ades AE et al (2008) Evaluation of networks of randomized trials. Stat Methods Med Res 17:279–301
Sutton A, Ades AE, Cooper N, Abrams K (2008) Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics 26:753–767
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Salanti G, Ades AE, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64:163–171
Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR (2012) Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods 3:98–110
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944
Furukawa TA, Salanti G, Atkinson LZ et al (2016) Comparative efficacy and acceptability of first-generation and second-generation antidepressants in the acute treatment of major depression: protocol for a network meta-analysis. BMJ Open 6:e010919
Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J Clin Epidemiol 54:1046–1055
He J, Hu Y, Hu M et al (2015) Development of PD-1/PD-L1·pathway in tumor immune microenvironment and treatment for non-small cell lung cancer. Sci Rep 5:13100
Wang Y, Zhou S, Yang F et al (2019) Treatment-related adverse events of PD-1 and PD-L1 inhibitors in clinical trials: a systematic review and meta-analysis. JAMA Oncol 5:1008–1019
Kazandjian D, Suzman DL, Blumenthal G (2016) FDA approval summary: nivolumab for the treatment of metastatic non-small cell lung cancer with progression on or after platinum-based chemotherapy. Oncologist 21:634–642
Pai-Scherf L, Blumenthal GM, Li H (2017) FDA approval summary: pembrolizumab for treatment of metastatic non-small cell lung cancer: first-line therapy and beyond. Oncologist 22:1392–1399
Weinstock C, Khozin S, Suzman DUS (2017) Food and Drug Administration approval summary: atezolizumab for metastatic non-small cell lung cancer. Clin Cancer Res 23:4534–4539
Antonia SJ, Villegas A, Daniel D (2017) Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med 377:1919–1929
Slater LM, Stupecky M, Sweet P, Osann KE (2002) Enhancement of leukemia rejection by mice successfully treated for L1210 leukemia due to low dose compared to high dose VP-16. Leuk Res 26:205–208
Li M, Hou X, Chen J et al (2021) Comparing organ-specific immune-related adverse events for immune checkpoint inhibitors: a Bayesian network meta-analysis. Clin Transl Med 11:e291
Xu C, Chen Y-P, Du X-J (2018) Comparative safety of immune checkpoint inhibitors in cancer: systematic review and network meta-analysis. BMJ 363:k4226
Huang Y-F, Xie W-J, Fan H-y et al (2019) Comparative safety of PD-1/PD-L1 inhibitors for cancer patients: systematic review and network meta-analysis. Front Oncol 9:972
Zhong Li, Qing Wu, Chen F et al (2021) Immune-related adverse events: promising predictors for efficacy of immune checkpoint inhibitors. Cancer Immunol Immunother 70(4):2559–2576
Schindler K et al (2014) Correlation of absolute and relative eosinophil counts with immune-related adverse events in melanoma patients treated with ipilimumab. ASCO Meet Abstr 32
Callahan MK et al (2011) Evaluation of serum IL-17 levels during ipilimumab therapy: correlation with colitis. ASCO Meet Abstr 29
Shahabi V et al (2013) Gene expression profiling of whole blood in ipilimumab-treated patients for identification of potential biomarkers of immune-related gastrointestinal adverse events. J Transl Med 11:75
Funding
This research received no funding.
Author information
Authors and Affiliations
Contributions
WZ gave substantial contributions to the conception or the design of the manuscript, JG and LS helped in acquisition, analysis, and interpretation of the data. XJ, JW, XZ, and HC have participated in the data collection of this article. All authors have participated to drafting the manuscript, WZ revised it critically. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no financial or personal relationships with other people or organizations that could inappropriately influence our work; there is no professional or other personal interest of any nature or kind in any product, service, or company.
Consent for publication
All the authors agreed to publish.
Ethical standards
This network meta-analysis is a data reintegration based on the original data, which does not involve ethics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gu, J., Shi, L., Jiang, X. et al. Severe immune-related adverse events of immune checkpoint inhibitors for advanced non-small cell lung cancer: a network meta-analysis of randomized clinical trials. Cancer Immunol Immunother 71, 2239–2254 (2022). https://doi.org/10.1007/s00262-022-03140-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-022-03140-5