Abstract
Purpose
Variations in hospital length of stay (LOS) and function are present after hip or knee arthroplasty. Comorbidity and performance measures have been associated with post-operative outcomes. It is however not known if both independently contribute to outcome prediction. The objective of this study was to evaluate the combined predictive ability of comorbidity scores (American Society of Anesthesiologists classification system (ASA), Charlson comorbidity index (CCI), 2008 version of the CCI (CCI08)) and a performance measure (Timed-Up-and-Go (TUG)) on LOS and short-term function in patients undergoing knee or hip arthroplasty.
Methods
One hundred eight patients undergoing hip or knee arthroplasty were assessed preoperatively with the ASA, CCI, CCI08, and TUG. LOS was determined through administrative data. The Older Americans Resources and Services ADL questionnaire (OARS) was used to assess function two and six weeks after surgery. Logistic regression was used to assess the relationship between pre-operative assessments and LOS and OARS scores.
Results
Both the ASA and TUG significantly contributed to LOS prediction. Odds ratio (OR) was 3.57 (95% confidence interval (CI) 1.26–10.07) for the ASA, and 2.18 (95% CI 1.67–4.15) for a one-standard deviation (SD) increase of 4.45 s of the TUG. Only the TUG was predictive of two weeks function and trending towards significance for six weeks function. One SD TUG increase yielded an OR of 2.14 (95% CI 1.53–3.79) for two week function.
Conclusions
The TUG and ASA can be used pre-operatively in combination to predict LOS, and TUG can also be used to predict short-term post-operative function.
Similar content being viewed by others
Introduction
Following hip or knee arthroplasty, patients experience variations with regards to hospital length of stay (LOS), hospital discharge destination, and functional outcomes. A minority of patients experience prolonged hospital length of stay and reduced short- and long-term function [1]. Although these patients represent the minority, they incur substantial use of resources and costs, both in the hospital and community [2]. Identifying these patients pre-operatively using valid criteria allows to plan post-operative resources accordingly. For research purposes, having valid case-mix criteria predictive of poorer outcomes allows to control for these in trials, either through stratified sampling or multivariate analyses. Pre-operative and peri-operative intervention trials targeting these patients can also be developed, in order to improve post-surgical outcomes. A thorough understanding of these parameters would also allow clinicians and hospital administrators to establish pre-operatively resources potentially needed post-operatively with greater confidence.
Several studies have identified factors predictive of poorer outcomes following hip or knee arthroplasty, which have been summarized in systematic reviews [3, 4]. Among these, comorbidities have constantly been shown to strongly predict poorer post-operative outcomes [3, 4]. The comorbidity measure most often demonstrated to predict knee or hip arthroplasty outcomes has been the American Society of Anesthesiologists physical status classification system (ASA) [3, 4]. The Charlson Comorbidity Index (CCI) is also frequently used, but its predictive validity is less clear [3, 4]. A revised version of the CCI was developed in 2008 (CCI08), in order to make it more responsive to chronic conditions [5].
A newer category of data that has been shown in recent studies to predict post-operative outcomes following knee or hip arthroplasty is performance measures. In these, the patient is asked to perform a standardized task and is assessed on his/her capacity to do the task. Several performance measures have been developed, including the ability to walk certain distances, ambulatory transitions, or stair negotiation. Of these, the Timed-Up-and-Go (TUG) assessed pre-operatively has been shown to predict post-operative outcomes following knee or hip arthroplasty, including LOS, short- and long-term function [6,7,8,9,10]. In the TUG, the patient is asked to get up from a chair with armrests, walk three metres, turn around, and sit back down. The patient is scored on the time it took to perform the task [11].
Although both ASA and TUG measures have been shown to predict post-surgical outcomes following hip or knee arthroplasty, they have not to our knowledge been assessed in the same population at the same time, using multivariate analyses. It is therefore not known if they relate to one another, or if they both independently contribute to post-operative outcomes prediction. If they are related or do not independently contribute to outcome prediction, then assessing both would be unnecessary, especially since the TUG requires time and resources to complete. Conversely, if comorbidity and performance measures both independently predict outcomes, this would suggest that both should be assessed pre-operatively in order to better predict post-operative outcomes. The objective of this study is to evaluate the combined predictive ability of the ASA, CCI, CCI08, and TUG of post-operative outcomes in patients undergoing knee or hip arthroplasty, using multivariate analyses.
Methods
Participants
Patients scheduled for unilateral primary knee or hip arthroplasty for osteoarthritis (OA) in a university-affiliated hospital in a university-affiliated hospital in Ottawa, Canada, were invited to participate in the study between March and October 2013. The following exclusion criteria were applied: knee or hip arthroplasty in the month preceding surgery; revision arthroplasty; diagnosed neurological or musculoskeletal disease (excluding OA) adversely affecting gait; unable to read and/or understand English; documented cognitive impairment precluding questionnaire completion; under 18 years of age. All patients received the standardized care map used at the Ottawa Hospital for joint arthroplasty, including anesthesia protocol and post-operative rehabilitation. For five independent variables in the multivariate regression model and an event rate of 50% in the dependant variable (using LOS data with the cutoff median of 3 days) [12], the minimum sample size is 100 using the formula N = 10 × number of covariates/event rate [13]. Taking into account possible drop-outs, 108 patients were recruited, with half undergoing hip arthroplasty (n = 54) and the other half knee arthroplasty.
Study design and setting
The TUG was administered pre-operatively by trained physical therapists blinded to other outcomes. Patients were blinded to TUG scores. ASA was completed pre-operatively by the anesthesiologist anticipated to be involved in the surgery, using patient interviews and charts. CCI was completed by an orthopaedic resident retrospectively using patient charts. Two versions of the CCI were calculated: the original version and the revised 2008 version. LOS was determined using administrative data. To assess short-term function after discharge, the Older Americans Resources and Services (OARS) ADL scale was used. It is composed of 14 questions that assess the patient’s perceived capacity to perform basic ADLs at home, such as bathing, dressing, getting in and out of bed, housekeeping, and getting around [14]. It has been validated to assess basic function at home following surgery and used to follow patients after arthroplasty [15,16,17]. The OARS was completed by patients two and six weeks after surgery. Demographic variables, including age, gender, BMI, and the Western Ontario and McMaster Osteoarthritis Index (WOMAC) score were also collected before surgery. WOMAC was not assessed shortly after surgery since it has been shown to be less responsive to change for that time period [18].
Statistical analysis
Relationships between preoperative measures (ASA, CCI, CCI08, and TUG) were assessed using bivariate analyses (t tests or chi-square). ASA was dichotomized using a cutoff of 1–2 vs 3–4, since this cutoff has been shown to be related to LOS, and scores of 1 or 4 are rare in patients undergoing TJA [3, 4]. Bivariate analyses were also used to study the relationship between pre-operative measures (TUG, ASA, CCI, CCI08) and post-operative outcome measures (LOS, 2 and 6 weeks OARS). Only the variables with a p value < .20 in the bivariate analyses were included in the multivariate logistic regression (Enter procedure). Separate logistic regressions were completed for each post-operative outcome measure as the dependent variable. Prolonged LOS was defined as three days or more, corresponding to the sample median and the US national average [12]. A cutoff of 19 out of 22 for the OARS was used at two weeks, as a reduction of three points in the OARS is considered to be a clinically significant decrease in function [19]. OARS at six weeks was dichotomized as 22 out of 22 (complete basic function) vs under 22. Surgery site (knee vs hip), age, gender, and BMI were also assessed as covariates. Explained variance of the regression models was assessed with Nagerkelke R2. All statistical analyses were performed using SPSS version 23 (SPSS Inc., Chicago, Illinois). A two-tailed level of significance of p < .05 was used in the logistic regressions.
Results
During recruitment, 17 knee and 6 hip patients were excluded because they suffered from a diagnosed neurological or musculoskeletal disease, in addition to OA, adversely affecting gait. These included rheumatoid arthritis, ankylosing spondylitis, spina bifida, spinal stenosis, hip dysplasia, Meniere’s disease, multiple sclerosis, Parkinson’s disease, or fibromyalgia. Of the final 108 participants, 54 were women (50%). The average age was 64 years (SD = 12.5 years), while the average body mass index (BMI) was 30.4 (SD = 6.2). The average pre-operative WOMAC function score was 50.3/100 (SD = 19.5). Half underwent hip arthroplasty. Fifty patients (46.3%) were hospitalized for one or two days, 41 (38%) for three days, and 17 (15.7%) for four or more days. For discharge destination, 98 patients were discharged home and ten were discharged elsewhere. Table 1 provides outcome measure data. Forty-six patients (44.7%) had an OARS score above 19 at two weeks, and 54 patients (51.9%) had complete basic function at six weeks.
When looking at the proportion of patients without comorbidities, this varied according to the instrument: ASA score of 1 = 4.6% of patients; ASA score of 1 or 2 = 52.8% of patients; CCI score of 0 = 61.1%; CCI08 score of 0 = 39.8%. Both CCI (p < .001) and CCI08 (p < .001) scores were significantly related to ASA scores. The average pre-operative TUG time was 11.4 s (SD of 4.4 s). None of the comorbidity scores were significantly related to TUG scores as follows: ASA (p = .29), CCI (p = .16), and CCI08 (p = .09).
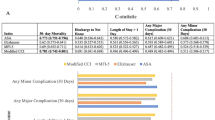
Bivariate analyses of pre-operative measures with LOS found that ASA (p < .01), TUG (p < .01), surgery site (p < .01), age (p = .02), gender (p < .01), BMI (p < .01), and CCI08 (p = .09) were significantly related to LOS, while CCI (p = .35) was not. Table 2 describes the regression results concerning LOS. Following regression, ASA, TUG, and gender significantly contributed to LOS prediction, while age, BMI, CCI08, and surgery site did not. The Nagerkelke R2 for the regression was 46.2%. The odds ratio (OR) for one SD increase of the TUG (4.45 s) was 2.18 (95% C.I. 1.67–4.15). Using a previously validated TUG cutoff of 10 s [6, 7, 20], patients with an ASA score of 3 or 4 AND a TUG of more than 10 s (representing 23.1% of patients) had an OR of prolonged LOS of 6.54 (95% C.I. 1.75–24.50).
Bivariate analyses of pre-operative measures with 2-week OARS scores found that TUG (p = .01), ASA (p = .12), and BMI (p = .05) were significantly related, while CCI (p = .23), CCI08 (p = .22), surgery site (p = .76), age (p = .51), and gender (p = .38) were not. Table 3 provides regression results related to 2-week OARS function. TUG and BMI significantly contributed to 2-week OARS prediction following the regression analysis, while ASA did not. The Nagerkelke R2 was 25.7% for the 2-week OARS regression. The OR for one SD TUG increase was 2.14 (95% C.I. 1.53–3.79).
Bivariate analyses of pre-operative measures with 6-week OARS scores demonstrated that the TUG (p = .03), BMI (p = .04), and gender (p = .06) were significantly related, while ASA (p = .57), CCI (p = .81), CCI08 (p = .78), surgery site (p = .55), and age (p = .30) were not. Table 4 provides regression results related to 6-week OARS function. Following regression analyses, the TUG and BMI were trending towards significance for 6-week OARS prediction, while gender did not significantly contribute. The Nagerkelke R2 was 13.8% for the six week OARS regression.
Discussion
Arthroplasty incurs substantial costs, with these costs associated with hospitalization and post-discharge recovery resources among others. Pre-operatively predicting LOS and post-operative function allows for estimation of the level of resources that patients will possibly require during hospitalization and after discharge, allowing healthcare organizations to plan accordingly based on the pre-operative characteristics of their clientele. Patients with worse pre-operative outcome scores would be expected to require additional resources, whereas those having better scores could be targeted for fast-tracking or same-day surgery.
Results confirm the predictive ability of the ASA score with regards to LOS. The cutoff found in other studies was also confirmed (1–2 vs 3–4), meaning that the ASA can be dichotomized [3, 4]. As with other cohorts, ASA scores of 1 and 4 were very rare, further justifying the dichotomization. Alternatively, both CCI and CCI08 were not predictive of any of the outcomes studied. The CCI was developed mainly to predict mortality associated with surgery [21], which is somewhat rare in the context of arthroplasty. The outcomes of this study were functional, with function being a core outcome following arthroplasty and applying to all patients. The CCI08 was developed in order to make it more responsive to chronic diseases. However, both the CCI and CCI08 score comorbidities based on the presence or absence of diseases, notwithstanding their impact on function. The ASA assesses the impact of comorbidities on function, since a score of 2 indicates “mild diseases only without functional limitations”, and a score of 3 is “substantive functional limitations; one or more moderate to severe diseases” [22]. Since LOS is partly determined by patient function, this possibly explains why ASA was predictive of LOS, while CCI and CCI08 were not. As with other studies, this study result questions the utility of the CCI/CCI08 when the objective is to predict LOS. If on the other hand the objective is to predict mortality, then the CCI/CCI08 could potentially be appropriate. The ASA is often considered more subjective than the CCI, but the subjective perception of the anesthesiologist appears to be a valid predictor of LOS. While the ASA was predictive of LOS, it was not of the other functional outcomes. LOS is dependent on the patient’s capacity to recover basic independent function after surgery [23], which appears to be reflected in the ASA score. However, more advanced function attained after hospital discharge does not appear to be captured with the ASA. If the objective is to predict functional outcomes beyond LOS, the ASA appears insufficient.
This study also confirms the independent contribution of the TUG to predict LOS, and the TUG and ASA were not statistically related to one another. This seems to confirm that these tools measure different dimensions while independently contributing to LOS, with the ASA being a general health index and the TUG a functional measure. LOS appears to be determined by different factors, with patient function (TUG) and general health (ASA) being two of them. Explained variance of LOS was also quite at high at 46.2%. Patients with a TUG of more than ten seconds and an ASA of 3 or 4 were more than 6 times at risk of prolonged LOS. Assessing patients pre-operatively with only two relatively simple tools (ASA and TUG) could help in determining who is at risk of needing further resources during hospitalization, or conversely who could be fast-tracked.
As for short-term basic function after hospital discharge, only the TUG was predictive of two weeks post-operative function and trending towards significance for six weeks post-operative function. Thus, pre-operative TUG was the tool most consistently predictive of all post-operative outcomes. The pre-operative TUG has also been shown to predict post-operative function for other health diseases, such as cardiac problems [24], showing the importance of basic pre-operative function irrespective of the disease or surgical intervention. The TUG is a measurement that combines basic functional tasks needed for everyday life, such as chair transfer and walking. The TUG takes minimal resources and time to accomplish, and has been shown to be one of the most widely used outcome measures in rehabilitation for arthroplasty [25]. Since explained variance (R2) decreased with time, function appears more complex the further the time period from surgery. In the longer term, perceived post-operative function can be influenced by numerous factors including patient expectations and needs, available resources such as caregivers, and living environment [26]. Other tools in addition to the TUG appear needed if the objective is to pre-operatively predict longer-term function with greater accuracy. Both the pre-operative TUG and ASA have been demonstrated as predictive of long-term function [27, 28], but not with the same population.
The study results are however limited by several factors. A number of patients were excluded because they suffered from a diagnosed neurological or musculoskeletal comorbidity impairing their ability to accomplish the TUG test. Even if the excluded subjects would have been included, it is doubtful this would have changed results since they would have scored a 3 or 4 on the ASA, and a poorer TUG performance would have been more likely. All the excluded cases actually had a LOS of three or more days. Also, the average pre-operative WOMAC function score of the participants is also comparable to the general OA population undergoing arthroplasty [29], and close to half of the sample was still suffering from comorbidities according to the various tools. Assessments are especially useful for cases that are less clear, in order to help in decision-making. The present study results therefore demonstrate the utility of the pre-operative TUG and ASA in patients with less clear outcomes. Study results were also limited to a six week follow-up. However, most of the recovery and variability between patients occur in the first month following arthroplasty [29], and early post-operative function is predictive of long-term function [30]. The limited predictive ability of the TUG for six weeks post-operative function is probably related to the use of the OARS, as it assesses only basic function, with the majority of patients showing perfect basic function at six weeks. A questionnaire assessing more advanced activities, such as the HOOS or WOMAC, would probably have been preferable for the six week post-operative period. Another study using the WOMAC has already demonstrated the predictive ability of the TUG for longer-term function [6].
References
Bitar YFE, Illingworth KD, Scaife SL et al (2015) Hospital length of stay following primary total knee arthroplasty: data from the nationwide inpatient sample database. J Arthroplast 30:1710–1715
Pugely AJ, Martin CT, Gao Y et al (2014) Comorbidities in patients undergoing total knee arthroplasty: do they influence hospital costs and length of stay? Clin Orthop Relat Res 472:3943–3950. https://doi.org/10.1007/s11999-014-3918-x
Olthof M, Stevens M, Bulstra SK, van den Akker-Scheek I (2014) The association between comorbidity and length of hospital stay and costs in total hip arthroplasty patients: a systematic review. J Arthroplast 29:1009–1014. https://doi.org/10.1016/j.arth.2013.10.008
Elings J, Hoogeboom TJ, van der Sluis G, van Meeteren NL (2015) What preoperative patient-related factors predict inpatient recovery of physical functioning and length of stay after total hip arthroplasty? A systematic review. Clin Rehabil 29:477–492. https://doi.org/10.1177/0269215514545349
Charlson ME, Charlson RE, Peterson JC et al (2008) The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 61:1234–1240. https://doi.org/10.1016/j.jclinepi.2008.01.006
Nankaku M, Tsuboyama T, Akiyama H et al (2013) Preoperative prediction of ambulatory status at 6 months after total hip arthroplasty. Phys Ther 93:88–93. https://doi.org/10.2522/ptj.20120016
Poitras S, Wood KS, Savard J et al (2015) Predicting early clinical function after hip or knee arthroplasty. Bone Joint Res 4:145–151. https://doi.org/10.1302/2046-3758.49.2000417
Petis SM, Howard JL, Lanting BA et al (2016) Peri-operative predictors of length of stay following total hip arthroplasty. J Arthroplast (January 22)
Toner A, Wallace G, Rowe J et al (2014) The relationship between pre-operative “timed get up and go”and length of stay in primary elective hip and knee arthroplasty patients. Osteoarthr Cartil 22:S380–S381
Sharareh B, Le NB, Hoang MT, Schwarzkopf R (2014) Factors determining discharge destination for patients undergoing total joint arthroplasty. J Arthroplast 29:1355–1358.e1. https://doi.org/10.1016/j.arth.2014.02.001
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Steiner C, Andrews R, Barrett M, Weiss A (2012) HCUP projections: mobility/orthopedic procedures 2003 to 2012. US Agency for Healthcare Research and Quality, US Agency for Healthcare Research and Quality
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Fillenbaum GG, Smyer MA (1981) The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J Gerontol 36:428–434
Haywood KL, Garratt AM, Fitzpatrick R (2005) Older people specific health status and quality of life: a structured review of self-assessed instruments. J Eval Clin Pract 11:315–327
George LK, Ruiz Jr D, Sloan FA (2008) The effects of total hip arthroplasty on physical functioning in the older population. J Am Geriatr Soc 56:1057–1062. https://doi.org/10.1111/j.1532-5415.2008.01685.x
George LK, Ruiz Jr D, Sloan FA (2008) The effects of total knee arthroplasty on physical functioning in the older population. Arthritis Rheum 58:3166–3171. https://doi.org/10.1002/art.23888; 10.1002/art.23888
Stratford PW, Kennedy DM, Riddle DL (2009) New study design evaluated the validity of measures to assess change after hip or knee arthroplasty. J Clin Epidemiol 62:347–352. https://doi.org/10.1016/j.jclinepi.2008.06.008
Hustey FM, Mion LC, Connor JT et al (2007) A brief risk stratification tool to predict functional decline in older adults discharged from emergency departments. J Am Geriatr Soc 55:1269–1274. https://doi.org/10.1111/j.1532-5415.2007.01272.x
Oosting E, Hoogeboom TJ, Appelman-de Vries SA et al (2016) Preoperative prediction of inpatient recovery of function after total hip arthroplasty using performance-based tests: a prospective cohort study. Disabil Rehabil 38:1243–1249. https://doi.org/10.3109/09638288.2015.1076074
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
American Society of Anaesthesiologists (2014) ASA physical status classification system
Harrison JD, Greysen RS, Jacolbia R, et al (2016) Not ready, not set… discharge: patient-reported barriers to discharge readiness at an academic medical center. J Hosp Med April 15:
Partridge JS, Fuller M, Harari D et al (2015) Frailty and poor functional status are common in arterial vascular surgical patients and affect postoperative outcomes. Int J Surg 18:57–63. https://doi.org/10.1016/j.ijsu.2015.04.037
McAuley C, Westby MD, Hoens A, et al (2014) A survey of physiotherapists’ experience using outcome measures in total hip and knee arthroplasty. Physiother CanadaPhysiotherapie Canada 66:274–285. doi: https://doi.org/10.3138/ptc.2013-34
Barsoum WK, Murray TG, Klika AK, et al (2010) Predicting patient discharge disposition after total joint arthroplasty in the United States. J Arthroplast 25:885–892. doi: 10.1016/j.arth.2009.06.022
Bade MJ, Kohrt WM, Stevens-Lapsley JE (2010) Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther 40:559–567. https://doi.org/10.2519/jospt.2010.3317
Lubbeke A, Katz JN, Perneger TV, Hoffmeyer P (2007) Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol 34:394–400
Kennedy DM, Stratford PW, Hanna SE et al (2006) Modeling early recovery of physical function following hip and knee arthroplasty. BMC Musculoskelet Disord 7:100. https://doi.org/10.1186/1471-2474-7-100
Jr JAZ, Snyder-Mackler L (2010) Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther 90:43–54
Acknowledgements
We would like to acknowledge the contribution of Jae-Jin Ryu for the study coordination, Gillian Parker and Sarah Plamondon for patient recruitment and data collection, Lyne Cuerrier, Jennifer Forget, Yvonne Kossen, Chantale Pryor and Olena Tonkyhk for data collection.
Funding
This work was supported by a grant from The Ottawa Hospital Academic Medical Organization (TOHAMO).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained from The Ottawa Hospital ethical review board. All patients gave their informed written consent for participation in the study.
Electronic supplementary material
ESM 1
(DOCX 62 kb)
Rights and permissions
About this article
Cite this article
Poitras, S., Au, K., Wood, K. et al. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: are both performance and comorbidity measures useful?. International Orthopaedics (SICOT) 42, 2295–2300 (2018). https://doi.org/10.1007/s00264-018-3833-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3833-y