Abstract
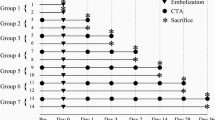
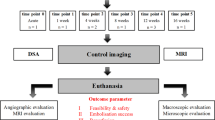
This study sought to compare the most frequently used embolic particles in an animal model. In 16 New Zealand white rabbits, right renal arteries were embolized using four different embolic particles (polyvinyl alcohol [PVA] particles, 150–250 μm; PVA microspheres [PVAMs], 150–300 μm; Tris-acryl gelatin microspheres [TGMs], 100–300 μm; expanding microspheres [EXMs], 50–100 μm). Quantity of embolic material used, embolization time, and angiographic patterns were documented. Fourteen days later, a control angiography was done to document angiographic recanalization and all animals were sacrificed. Histopathological specimens were analyzed for microscopic appearance and granulometric size of the particles, extravasation of the particles, perivascular inflammation, and neocapillarization. The volume of the infarct area in each kidney was calculated. Results revealed a significantly lesser amount of embolic material used in the EXM group (p = 0.020). The angiographic recanalization rate in the EXM group (100%), compared with the PVA (0%) and TGM (0%) groups, was found to be statistically significant (p = 0.014). Although 75% of the renal arteries embolized with PVAMs were recanalized, this was not found to be statistically significant (p = 0.071). Occlusion levels in the PVA group were more proximal than with any of the microspheres. While there was no extravasation in the TGM group, extravasation rates in the PVA, PVAM, and EXM groups were 50%, 25%, and 75%, respectively. A mild degree of inflammation was noted in the PVA, PVAM, and TGM groups. EXMs caused a moderate degree of inflammation in two kidneys (50%). There was neocapillarization in the vessel lumen in all kidneys in the PVA and PVAM groups. The difference was significant (p = 0.014) compared with the TGM and EXM groups, which did not have any neocapillarization. Regarding infarct area volumes, the difference among the groups was significant (p = 0.022). EXMs caused significantly (p = 0.021) less infarction than the other embolic agents. We conclude that EXMs are less efficient due to a high recanalization rate and lesser volume of infarct compared with the other embolic agents in the rabbit kidney model. The most efficient embolization was seen in kidneys embolized with TGMs.








Similar content being viewed by others
References
Siskin GP, Dowling K, Virmani R et al (2003) Pathologic evaluation of a spherical polyvinyl alcohol embolic agent in a porcine renal model. J Vasc Interv Radiol 14:89–98
Bendszus M, Klein R, Warmuth-Metz M et al (2000) Efficacy of trisacryl gelatin microspheres versus polyvinyl alcohol particles in the preoperative embolization of meningiomas. AJNR Am J Neuroradiol 21:255–261
Laurent A, Wassef M, Chapot R et al (2006) Arterial distribution of calibrated tris-acryl gelatin and polyvinyl alcohol microspheres in a sheep kidney model. Invest Radiol 41:8–14
Khankan AA, Osuga K, Hori S et al (2004) Embolic effects of superabsorbent polymer microspheres in rabbit renal model: comparison with tris-acryl gelatin microspheres and polyvinyl alcohol. Radiat Med 22:384–390
Osuga K, Hori S, Kitayoshi H et al (2002) Embolization of high flow arteriovenous malformations: experience with use of superabsorbent polymer microspheres. J Vasc Interv Radiol 13:1125–1133
Stampfl S, Bellemann N, Stampfl U et al (2008) Inflammation and recanalization of four different spherical embolization agents in the porcine kidney model. J Vasc Interv Radiol 20:936–945
Bilbao JI, de Luis E, García de Jalón JA et al (2008) Comparative study of four different spherical embolic particles in an animal model: a morphologic and histologic evaluation. J Vasc Interv Radiol 19:1625–1638
Link DP, Strandberg JD, Virmani R et al (1996) Histopathologic appearance of arterial occlusions with hydrogel and polyvinyl alcohol embolic material in domestic swine. J Vasc Interv Radiol 7:897–905
Derdeyn CP, Graves V, Salamat MS et al (1997) Collagen-coated acrylic microspheres for embolotherapy: in vivo and in vitro characteristics. AJNR Am J Neuroradiol 18:647–653
Osuga K, Hori S, Sugiura T et al (2008) Bland embolization of hepatocellular carcinoma using superabsorbent polymer microspheres. CardioVasc Interv Radiol 31:1108–1116
Kwak BK, Shim HJ, Han S et al (2005) Chitin based embolic materials in the renal artery of rabbits: pathologic evaluation of an absorbable particulate agent. Radiology 236:151–158
Konya A, Van Pelt CS, Wright KC (2004) Ethiodized oil-ethanol capillary embolization in rabbit kidneys: temporal histopathologic findings. Radiology 232:147–153
Fujiwara K, Hayakawa K, Hiraoka M et al (2000) Experimental embolization of rabbit renal arteries to compare the effects of poly L-lactic acid microspheres with and without epirubicin release against intraarterial injection of epirubicin. CardioVasc Interv Radiol 23:218–223
Chang D, Seo M, Choi H et al (2002) Application of transarterial embolization of renal artery in rabbits with experimental hydronephrosis. J Vet Med Sci 64:693–698
Stampfl S, Stampfl U, Rehnitz C et al (2007) Experimental evaluation of early and long-term effects of microparticle embolization in two different mini-pig models. Part I: Kidney. CardioVasc Interv Radiol 30:257–267
Klisch J, Yin L, Requejo F et al (2002) Liquid 2-poly-hydroxyethyl-metachrylate embolization of experimental arteriovenous malformations: feasibility study. AJNR Am J Neuroradiol 23:402–429
Gundersen HJ, Bendtsen TF, Korbo L et al (1988) Some new, simple and efficient stereological methods and their use in pathological research and diagnosis. APMIS 96:379–394
Turjman F, Massoud TF, Vinters HV et al (1995) Collagen microbeads: experimental evaluation of an embolic agent in the rete mirabile of the swine. AJNR Am J Neuroradiol 16:1031–1036
de Luis E, Bilbao JI, de Ciércoles JA et al (2008) In vivo evaluation of a new embolic spherical particle (hepasphere) in a kidney animal model. CardioVasc Interv Radiol 31:367–376
Pelage JP, Laurent A, Wassef M et al (2002) Uterine artery embolization in sheep: comparison of acute effects with polyvinyl alcohol particles and calibrated microspheres. Radiology 224:436–445
Derdeyn CP, Moran CJ, Cross DT III et al (1995) Polyvinyl alcohol particle size and suspension characteristics. Am J Neuroradiol 16:1335–1343
Manelfe C, Lasjaunias P, Ruscalleda J (1986) Preoperative embolization of intracranial meningiomas. Am J Neuroradiol 7:963–972
Wakhloo AK, Juengling FD, Velthoven Van et al (1993) Extended preoperative polyvinyl alcohol microembolization of intracranial meningiomas: assessment of two embolization techniques. Am J Neuroradiol 14:571–581
Handa J, Nakasu S, Matsuda I (1980) Facial nerve palsy following therapeutic embolization. Surg Neurol 14:377–380
Laurent A (2007) Microspheres and nonspherical particles for embolization. Tech Vasc Interv Radiol 10:248–256
Osuga K, Khankan AA, Hori S et al (2002) Transarterial embolization for large hepatocellular carcinoma with use of superabsorbent polymer microspheres: initial experience. J Vasc Interv Radiol 13:929–934
Grosso M, Vignali C, Quaretti P et al (2008) Transarterial chemoembolization for hepatocellular carcinoma with drug-eluting microspheres: preliminary results from an Italian multicentre study. CardioVasc Interv Radiol 31:1141–1149
Davidson GS, Terbrugge KG (1995) Histologic long-term follow-up after embolization with polyvinyl alcohol particles. Am J Neuroradiol 16:843–846
Tomashefski JF, Cohen AM, Doershuk CF (1988) Long-term histopathologic follow-up of bronchial arteries after therapeutic embolization with polyvinyl alcohol (Ivalon) in patients with cystic fibrosis. Hum Pathol 19:555–561
Fournier D, Terbrugge K, Rodesch G et al (1990) Revascularization of brain arteriovenous malformations after embolization with bucrylate. Neuroradiology 32:497–501
Gobin YP, Viñuela F, Vinters HV et al (2000) Embolization with radiopaque microbeads of polyacrylonitrile hydrogel: evaluation in swine. Radiology 214:113–119
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Senturk, C., Cakir, V., Yorukoglu, K. et al. Looking for the Ideal Particle: An Experimental Embolization Study. Cardiovasc Intervent Radiol 33, 336–345 (2010). https://doi.org/10.1007/s00270-009-9747-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-009-9747-8