Abstract
Purpose
This study was designed to investigate the safety and efficacy of endovascular intervention for the treatment of primary entire-inferior vena cava (IVC) occlusion.
Methods
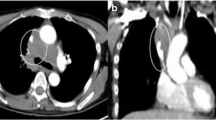
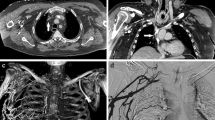
Endovascular interventions were performed in six patients for the treatment of primary entire-IVC occlusion. IVC and hepatic venography were performed via the jugular and femoral veins. Balloon angioplasty was used to revascularize the hepatic vein and IVC and a stent was placed in the IVC to maintain patency. Postoperative color Doppler ultrasonography was performed at 1, 3, 6, and 12 months, and then annually, to monitor the patency of the hepatic vein and IVC.
Results
The IVC and one or two hepatic veins were successfully revascularized in five patients. Revascularization was successful in the right and left hepatic veins in one patient; however, IVC patency could not be established in this patient. Eleven Z-type, self-expanding stents were placed into the IVCs of five patients (three stents in two patients, two stents in two patients, and one stent in one patient). There were no instances of postoperative bleeding or mortality. Follow-up was conducted for 18–90 months (42.8 ± 26.5 months). None of the five patients suffered restenosis of the IVC or hepatic veins. However, there was one of the six cases of right hepatic vein restenosis at 18 months postprocedure that was revascularized after a second balloon dilatation.
Conclusions
Endovascular intervention is safe and efficacious for the treatment of primary entire-IVC occlusion.


Similar content being viewed by others
References
Rikitake K, Itoh T, Natsuaki M, Katayama Y, Ohtsubo S, Kataoka H (2006) Surgical repair for entire inferior vena cava occlusion in Budd–Chiari syndrome. Asian Cardiovasc Thorac Ann 14(5):e88–e90
Lorenz JM, van Beek D, Funaki B, Van Ha TG, Zangan S, Navuluri R et al (2014) Long-term outcomes of percutaneous venoplasty and Gianturco stent placement to treat obstruction of the inferior vena cava complicating liver transplantation. Cardiovasc Intervent Radiol 37(1):114–124
Sato Y, Inaba Y, Yamaura H, Takaki H, Arai Y (2012) Malignant inferior vena cava syndrome and congestive hepatic failure treated by venous stent placement. J Vasc Interv Radiol 23(10):1377–1380
Kalva SP, Marentis TC, Yeddula K, Somarouthu B, Wicky S, Stecker MS (2011) Long-term safety and effectiveness of the “OptEase” vena cava filter. Cardiovasc Intervent Radiol 34(2):331–337
Tekbas G, Oguzkurt L, Gur S, Onder H, Andic C (2012) Endovascular treatment of veno-occlusive Behçet’s disease. Cardiovasc Intervent Radiol 35(4):826–831
Seijo S, Plessier A, Hoekstra J, Dell’era A, Mandair D, Rifai K et al (2013) Good long-term outcome of Budd–Chiari syndrome with a step-wise management. Hepatology 57(5):1962–1968
Robbins MR, Assi Z, Comerota AJ (2005) Endovascular stenting to treat chronic long-segment inferior vena cava occlusion. J Vasc Surg 41(1):136–140
Liu C, Zheng Y, Yang X, Shao J, Song X, Lu X et al (2011) Radical correction for Budd–Chiari syndrome through a transabdominal approach. Ann Vasc Surg 25(5):702–706
Haskal ZJ, Potosky DR, Twaddell WS (2014) Percutaneous endovascular creation of an inferior vena cava in a patient with caval agenesis, Budd–Chiari syndrome, and iliofemorocaval thrombosis. J Vasc Interv Radiol 25(1):63–69
Porter JM, Moneta GL (1995) Reporting standards in venous disease: an update. International Consensus Committee on Chronic Venous Disease. J Vasc Surg 21(4):635–645
Santise G, D’Ancona G, Baglini R, Pilato M (2010) Hybrid treatment of inferior vena cava obstruction after orthotopic heart transplantation. Interact CardioVasc Thorac Surg 11(6):817–819
McAree BJ, O’Donnell ME, Fitzmaurice GJ, Reid JA, Spence RA, Lee B (2013) Inferior vena cava thrombosis: a review of current practice. Vasc Med 18(1):32–43
Thompson CS, Cohen MJ, Wesley JM (2006) Endovascular treatment of obliterative hepatocavopathy with inferior vena cava occlusion and renal vein thrombosis. J Vasc Surg 44(1):206–209
McAree BJ, O’Donnell ME, Boyd C, Spence RA, Lee B, Soong CV (2009) Inferior vena cava thrombosis in young adults–a review of two cases. Ulster Med J 78(2):129–133
Jones VS, Shun A (2007) Is the inferior vena cava dispensable. Pediatr Surg In 23(9):885–888
Szkutnik M, Qureshi SA, Kusa J, Rosenthal E, Bialkowski J (2007) Use of the Amplatzer muscular ventricular septal defect occluder for closure of perimembranous ventricular septal defects. Heart 93(3):355–358
Zhang CQ, Fu LN, Xu L, Zhang GQ, Jia T, Liu JY et al (2003) Long-term effect of stent placement in 115 patients with Budd–Chiari syndrome. World J Gastroenterol 9(11):2587–2591
Jones DW, Schneider DB (2012) Endovascular management of chronic inferior vena cava and iliac vein obstruction. Vasc Dis Manag 9(3):E33–E38
te Riele WW, Overtoom TT, van den Berg JC, van de Pavoordt ED, de Vries JP (2006) Endovascular recanalization of chronic long-segment occlusions of the inferior vena cava: midterm results. J Endovasc Ther 13(2):249–253
Keshava SN, Moses V, Surendrababu NR (2009) Cannula-assisted and transabdominal ultrasound-guided hepatic venous recanalization in Budd Chiari syndrome: a novel technique to avoid percutaneous transabdominal access. Cardiovasc Intervent Radiol 32(6):1257–1259
Li T, Zhai S, Pang Z, Ma X, Cao H, Bai W et al (2009) Feasibility and midterm outcomes of percutaneous transhepatic balloon angioplasty for symptomatic Budd–Chiari syndrome secondary to hepatic venous obstruction. J Vasc Surg 50(5):1079–1084
Witz M, Korzets Z (2007) Renal vein occlusion: diagnosis and treatment. Isr Med Assoc J 9(5):402–405
Kapur S, Paik E, Rezaei A, Vu DN (2010) Where there is blood, there is a way: unusual collateral vessels in superior and inferior vena cava obstruction. Radiographics 30(1):67–78
Acknowledgments
This study was funded by Jiangsu Provincial Special Program of Medical Science (No. BL2014030).
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Q., Huang, Q., Shen, B. et al. Efficacy and Safety of Endovascular Intervention for the Management of Primary Entire-Inferior Vena Cava Occlusion. Cardiovasc Intervent Radiol 38, 665–671 (2015). https://doi.org/10.1007/s00270-014-0980-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-014-0980-4