Abstract
Rituximab is used as a standard of care for follicular lymphoma and is usually administered intravenously. A novel subcutaneous formulation recently showed non-inferior efficacy with similar pharmacokinetic and safety profiles compared to intravenous rituximab in patients with follicular lymphoma. This new approach is promising in terms of comfort for patients and time-saving for hospital staff. To evaluate the real-life economic impact of subcutaneous rituximab as maintenance therapy in patients with follicular lymphoma in real life, we conducted a cost-consequence analysis from the hospital’s point of view in three French teaching hospitals. Health-related quality of life (EQ-5D-3L) was investigated as well as patients’ and nurses’ perception. Compared to intravenous rituximab, subcutaneous administration showed an estimated cost-saving of €109.20 per patient per cycle (p < 0.001), 78.6% of which could be attributed to the rituximab cost. Health-related quality of life showed no significant difference between the two groups despite tendencies for greater pain in the subcutaneous group and greater anxiety in the intravenous group. Thus, subcutaneous rituximab had a favorable pharmacoeconomic profile, with clinical efficacy similar to that of intravenous rituximab. The subcutaneous form was preferred by almost all patients, but further consideration should be given to improve the patients’ experience: a dedicated day unit with trained medical, nursing, and pharmaceutical staff could be helpful.
Similar content being viewed by others
Introduction
Non-Hodgkin lymphoma is one of the most common hematologic malignancies and constitutes a heterogeneous group of diseases characterized by abnormal proliferation of lymphoid cells (B lymphocytes or T cells). Follicular lymphoma is one of the commonest forms (20–25% of all cases) [1, 2]. Median survival after diagnosis exceeds 15 years, with an initial 6 months’ induction treatment, based on a multidrug chemotherapy regimen including the chimeric monoclonal antibody rituximab [3,4,5]. The administration of rituximab maintenance monotherapy by intravenous (IV) rituximab (375 mg/m2 every 8 weeks for 2 years) after response to induction treatment improves progression-free survival (59.2 versus 42.7% after 6 years, p < 0.0001) [6,7,8].
To date, the IV route is standard for the administration of antineoplastic agents but places clinical and organizational demands on the patient. The subcutaneous (SC) route has so far been little used, due to the low injection volume tolerated. Recombinant human hyaluronidase was developed to solve this problem (by degrading temporarily the SC matrix), allowing SC delivery of larger molecules such as antibodies that might not otherwise be feasible [9].
The SC formulation, containing a fixed dose of 1400 mg rituximab, has recently come on the market as an alternative to IV treatment in patients with non-Hodgkin lymphoma [10]. The randomized phase III SABRINA study, performed on 127 patients, demonstrated non-inferior pharmacokinetics parameters for SC compared to IV rituximab in patients with previously untreated follicular lymphoma, during induction therapy [11, 12].The overall safety profile of SC rituximab was consistent with the known safety profile of IV treatment, except for local reactions including erythema, rash, and pruritus (grades 1–2). This new approach is promising in terms of comfort for patients and time-saving for hospital staff. Thus, the study by Rule et al. in the UK showed that SC rituximab was associated with reduced active healthcare professional (HCP) time (defined as the time dedicated to a specific task involving physical presence) and costs compared to IV rituximab [13].
Outcome in cancer therapy is traditionally evaluated on clinical and biological parameters. However, quality of life and the patient’s perception and preferences become relevant when treatment efficacy is equivalent, especially in oncology, where the goal is not only to cure or prolong survival but also to preserve quality of life [14].
The increasing use of SC rituximab requires assessment of the real-life impact on patient care in an economic context of restricted health resources. The objectives of the present study were therefore to evaluate the economic impact of using SC rituximab as maintenance therapy compared to usual patient care for follicular lymphoma and secondly to investigate health-related quality of life, patients’, and nurses’ perceptions and preferences, in the context of the French health service.
Materials and methods
Study design and objectives
A medico-economic observational cross-sectional comparative study was conducted in three French teaching hospitals: Lyon, Nantes, and Tours. The aim was to assess the economic impact of managing patients with follicular lymphoma treated by SC rituximab as maintenance therapy compared to the usual strategy using IV rituximab. It was assumed that the two strategies would prove equivalent in terms of efficacy; therefore, the evaluation consisted in a cost-consequence analysis from the hospital’s point of view, with a time horizon of 1 chemotherapy cycle [15, 16]. Health-related quality of life, pain following administration, and patients’ and nurses’ perceptions and preferences were also assessed.
One of the three participating centers constituted the SC cohort and the other two the IV cohort. Following SC rituximab’s referencing, it was decided to switch all patients in Hospices Civils de Lyon to subcutaneous formulation, apart from particular cases. Therefore, a comparative study versus IV formulation was avoided in this single center.
Study population
This real-life study was conducted in patients with follicular lymphoma receiving rituximab maintenance monotherapy. All patients agreeing to participate were included, over a 2-month period. The study respected the Helsinki Declaration, French regulations, and institutional guidelines; given the nature of this research, no ethics committee approval was needed. An information leaflet explaining the whole project was given to patient before interview.
Cost-consequence analysis
Identification and quantification of costs
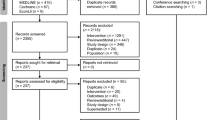
First, the specific tasks involved in the IV and SC rituximab processes were determined and possible differences between the two strategies were assessed (Fig. 1). The preliminary steps of supply and storage of pharmaceuticals products at pharmacy were similar for both formulations. It was assumed that the medical prescription, pharmaceutical validation, dispensing, and transport processes did not differ between the two strategies. Therefore, only resources related to drug preparation in the pharmaceutical unit and those to administration in the hematology day unit were collated, using micro-costing. This involves enumerating and costing out each resource used by a given patient. The following data for direct costs were collected: treatments and medical devices used in practice and active HCP time measured by stopwatch. Active HCP time was defined as the time dedicated to a given task, with the worker physically present either in the sterile workstation for the pharmacy technician or near the patient for the nurse.
Monetization
The various cost items were identified and quantified for monetization in Euros, from the hospital’s point of view. Drug and medical device consumption was quantified with the type and quantity used for 1 cycle of rituximab and monetized according to the 2016 prices. Active HCP time was quantified and monetized according to the 2016 hourly wage costs obtained from the human resources department: €31.8/h for a nurse and €30.6/h for a pharmacy technician (including gross annual salary and other employer expenses). Total cost per cycle of rituximab was calculated by summing costs for the rituximab drug, pre-medication, preparation, and administration. Results were presented in the form of “cost-saving”: difference between the total costs for the IV and SC formulations.
Data collection
Observations were collected during patients’ real-life clinical care by the pharmaceutical team in each center. In parallel, an individual semi-structured interview was conducted to assess patient perception. Additionally, the patient’s preference between the two formulations was assessed in the SC arm.
Health-related quality of life was evaluated on the French version of the self-administered EQ-5D-3L questionnaire, which assesses two indicators. The objective indicator includes 5 dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) with 3 levels on each (no complaints, mild complaints, severe complaints), which define 243 possible health states. The outcome is the EQ-5D score, ranging from − 0.529 to 1: 1 = the best health condition, 0 = death, and negative values = health condition worse than death [17]. The subjective indicator includes a visual analogue scale (EQ-VAS). The outcome is the EQ-5D VAS, with values ranging from 0 to 100: 0 = the worst health condition and 100 = the best health condition.
Pain following administration was evaluated on a 0–10 visual analogue scale. A self-administered questionnaire was designed to evaluate nurses’ perception and, in the SC arm, preference between the two formulations.
Data analysis
All data were analyzed with IBM SPSS Statistics 19 software. Missing data were replaced by a simple mean imputation. Descriptive data were expressed as mean (standard deviation [SD]) and median (range) for quantitative variables and as number of patients (percentage) for qualitative data. Comparisons between groups were analyzed using the chi-squared test (or Fisher’s exact test when the requirements for the chi-squared test was not met) for qualitative data and the Student’s t test (or Mann-Whitney U test when the normality requirement was not satisfied) for quantitative variables. EQ-5D index and the EQ-VAS data were expressed as mean [SD] and median and 25th and 75th percentiles. The effect of selected aspects of quality of life of patients was evaluated with analysis of variance (ANOVA). Statistical significance was defined as p < 0.05.
Univariate sensitivity analysis was performed to determine the robustness of results, on variables with significant weight in terms of cost according to our results or for which there was a large difference between the two management strategies. It was performed with minimum and maximum as variation interval for each parameter and with a decrease of 20% in the purchase price of IV rituximab, on the hypothesis that rituximab biosimilars will be introduced following patent expiration. This percentage corresponds to the minimal price advantage provide by biosimilars compared to original, varying between 20 and 40% in European countries [18].
Results
Data were collected from the three participating centers between February and April 2016. In all, 31 observations were recorded for IV and 42 for SC rituximab. Patient characteristics are shown in Table 1. Most were in first line (72.6%) and had received 6 to 8 cycles of R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) as induction therapy. In average, patients in SC group had received six IV rituximab infusions before switched to SC form. IV rituximab was dosed according to individual body surface area (BSA) (375 mg/m2, BSA capped at 2 m2); SC rituximab was a fixed 1400 mg dose, in accordance with the market authorization. Mean BSA was similar in the two groups.
Costs
Total estimated cost-saving per cycle was €109.20 (Table 2), including cost-saving component for drugs (rituximab and premedication) of €86.70 in the SC versus the IV arm, €85.80 of which was for the rituximab. Prophylactic medication comprised corticosteroids, antihistamines, and antipyretics. Choice of pre-medication and medical devices depended on the patient’s individual characteristics, rituximab formulation, and center procedures. In center 1, IV rituximab was administered through an implantable port (45.5%) or a peripheral vein (54.5%), whereas in center 2, all patients (n = 20) received IV rituximab by a port. The estimated mean cost-saving for medical devices was €10.50, of which €2.40 concerned the preparation and €8.10 the administration of rituximab. The mean active HCP time saved by using SC instead of IV rituximab was 5.6 min per preparation and 11.1 min per administration, for a total mean-cost saving of €12.00, comprising €5.70 for two pharmacy technicians (manipulator and manipulator support) and €6.30 for nurses. Sensitivity analysis showed that it would be less expensive for the hospital to use the IV formulation in two cases: (i) for people with small body surface area (< 1.7 m2) and (ii) if the purchase price of IV rituximab further decreases, as expected with the advent of biosimilar forms. Among the SC cohort, 12 patients had a body surface area under 1.7 m2. If these patients had been treated by IV rituximab, a mean of €226 could be saved pro cycle [min €79; max €451].
Quality of life
Health-related quality of life was assessed on the EQ-5D-3L. Of the five dimensions, follicular lymphoma patients treated with IV or SC rituximab most often reported either moderate anxiety/depression (41.9 and 34.1%, respectively) or moderate pain/discomfort (38.7 and 46.3%, respectively). The dimension with least problems was self-care, with no problem for 96.8% of patients with IV rituximab and 90.2% with SC rituximab (Table 3). Mean EQ-5D VAS score was 70.6 for IV rituximab and 71.0 for SC rituximab (p = 0.973). Mean EQ-5D score was 0.8 for IV rituximab and 0.7 for SC rituximab (p = 0.305) (Table 4). Analysis of variance showed no significant correlations between age, gender, and number of chemotherapy cycle and EQ-5D or EQ-VAS score.
Patient’s perception
The semi-structured interviews addressed several dimensions (Table 5). Concerning knowledge, the majority of patients reported that they had been sufficiently informed about the mode of action of rituximab, warnings signs, and possible side effects.
Rituximab tolerance
Treatment tolerance was “good” in 77.4% (n = 24) and 83.3% (n = 35) of patients with IV and SC rituximab, respectively (p = 0.790). Nevertheless, 54.8% (n = 17) of IV patients reported at least one injection-related adverse reaction: mainly hypersensitive reaction (flushing, throat itch, etc.), digestive disorder, and fatigue; in comparison, 47.6% (n = 20) of SC patients reported predominantly local reactions (redness, pain, hematoma, etc.). SC patients (76.2%; n = 32) still had a port versus 83.9% (n = 26) in the IV arm. Side effects comprised local reactions (inflammation, itching, discomfort, and pain), infection, and obstruction of the port. Mean VAS pain score following rituximab administration was 0.71 for the IV arm and 1.10 for the SC arm (p = 0.447).
Hematology day unit stay
Mean hematology day unit stay, from arrival to departure, was 3.16 h (SD = 0.62) for the SC group and 3.58 h (SD = 0.91) for the IV group (p = 0.105). This duration was estimated by the patients as 4.10 h in the SC group and 3.75 h in the IV group (p = 0.046).
Patient preference
All patients in the SC arm had history of IV rituximab. Most (n = 29; 69.0%) preferred the SC route, and only 2 (4.8%) the IV route, while 11 (26.2%) had no preference. Time-saving was the mean reason (22 patients; 52.4%). Other reasons were “making cancer less alarming: with no IV port hanging out, it seems less serious,” “less technical procedure,” “a simple SC injection is less bothersome, and less scary,” and “the port can be removed”. Those who preferred the IV route stressed the absence of local adverse reactions (pain, etc.) in contrast to SC administration.
Nursing survey
Twenty-six nurses completed the perception questionnaire: 9 (34.6%) in the SC center and 17 (65.4%) in the IV centers. On a Likert scale, 15 nurses (58.8%) in the IV group “somewhat agreed” that both formulations are equally effective whereas 7 nurses (77.8%) in the SC center did not know. In both cohorts, most (77%) agreed that SC rituximab was better tolerated than the IV form and that it reduced day unit stay and consumable use. However, nurses in the SC group reported no difference in terms of pharmacy preparation time or day unit stay. In the SC center, four of the eight nurses (50%) preferred administering IV rituximab, two (25%) preferred SC rituximab, and two (25%) did not have any preference.
Discussion
The objective of this real-life study in patients with follicular lymphoma was to evaluate hospital costs of the new SC formulation of rituximab as maintenance therapy, compared to the standard IV formulation. Considering total estimated cost, use of SC rituximab saved €109.20 compared to IV administration (p = 0.001), of which €85.80 (78.6%) was due to the rituximab itself. Only €10.50 (9.6%) of the savings was related to medical devices and €12.00 (11.0%) to active HCP time. Time-saving for nurses was not significantly different as expected, because in IV administration, a nurse can take care of several patients at a time and need not necessarily be physically present with a given patient throughout, in contrast to SC administration. It is important to emphasize that the steps of prescription, pharmaceutical validation, dispensation, and transport of rituximab to the hematology unit were not included in this assessment, as costs were assumed to be identical for the two formulations. A study of trastuzumab, a monoclonal antibody used in patients with breast cancer, showed that the SC formulation provided non-significant time savings of 1.25 min for medical prescription and 0.25 min for pharmaceutical validation compared to the IV formulation [19].
Sensitivity analysis showed that it would be less expensive for the hospital to use the IV formulation in some specific situations. Firstly, in case of small body surface area (< 1.7 m2), IV rituximab would be less expensive because dose is directly related to body surface area. Moreover, the pharmacy technicians use all the contents of the vials, including residues from IV rituximab vials for the further preparations, thus generating savings, which is not possible with the SC rituximab vial. In our study, those potential savings were not taken into account, and the cost of IV rituximab was calculated as price per milligram. Secondly, the price of IV rituximab is expected to decrease by about 20% once biosimilars come onto the market as it was described with biosimilar trastuzumab [20]. A reduction at least 6% to the price of IV rituximab would just compensate the efficiency advantage of SC rituximab. However, because of the advantages of and patients’ preference for the SC route, it may be difficult to go back to the IV formulation.
Apart from the economic aspect, SC rituximab was developed to improve patient comfort. The PrefMab study compared patient preference and satisfaction between the two formulations. Patients with non-Hodgkin lymphoma previously untreated received one IV rituximab cycle (375 mg/m2) followed by either SC rituximab (for 1400 mg, × 3) then IV rituximab (× 4) or IV rituximab (× 3) then SC rituximab (× 4), with chemotherapy. Patient preference was evaluated at cycles 6 and 8 using Patient Preference Questionnaire. Satisfaction was evaluated with the validated Cancer Therapy Satisfaction Questionnaire (CTSQ) and Rituximab Administration Satisfaction Questionnaire (RASQ) at cycles 4 and 8. At cycle 8, 81% preferred rituximab SC, independently to treatment sequence or disease type. The most common reason for preference was “require less time in the clinic.” Satisfaction was higher for SC with RASQ questionnaire and similar between the two formulations with CTSQ questionnaire [21]. In the present study, preference for SC rituximab was lower (69%), and 26.2% of patients had no preference.
Although the two formulations have the same efficacy, a cost-utility analysis could still have been performed. However, the evaluation of health-related quality of life on the EQ-5D-3L questionnaire revealed no significant difference between the two groups. Thus, as both efficacy and utility were similar, a cost-consequence analysis seemed more relevant. Nevertheless, cost-utility analyses of IV rituximab have been performed. Deconinck et al. examined the long-term cost-effectiveness of IV rituximab maintenance therapy after induction chemotherapy, compared with observation, in patients with relapsed follicular lymphoma. The authors concluded that rituximab was cost-effective from the point of view of the French National Health Service. Expected QALYs (quality-adjusted life years) were 4.7177 with rituximab and 3.6794 with observation [22].
The present results suggested certain trends: patients tended to experience more anxiety and depression with the IV formulation and more pain and discomfort with the SC formulation. It is conceivable that SC injection is more painful and stressless than using a port. A further study should investigate such trends. Several studies assessed the quality of life of patients with follicular lymphoma treated by rituximab in comparison to no treatment, but none compared IV and SC rituximab. Studies reported that IV rituximab had no harmful effect on patients’ quality of life [23]. In this present real-world study, patients’ experience shows that all tolerated rituximab well. Adverse effects were generally hypersensitive reactions in the IV group and local reactions in the SC group.
The expected improvement in patient comfort with SC rituximab was mainly based on time-saving in administration: 1 h 30 min for IV versus 5 min for SC, according to the summary of products characteristics. Nevertheless, the summary of product characteristics for the SC formulation recommends 15-min post-administration monitoring, increasing overall time to 20 min, whereas there is no such recommendation for the IV form, and in practice, no post-injection monitoring is performed for IV rituximab. Time-saving was the main reason for preferring the SC formulation, findings also observed in PrefMab [21]. Although patients highlighted the bother of having to go to the hospital for “a simple injection,” they also thought that they received better medical care in the day unit than at home. Like in the IV arm, most patients in the SC arm had a port, for induction polychemotherapy. It would be interesting to assess the benefit of early port ablation in patients receiving SC rituximab. When associated to other chemotherapy, the SC form loses a certain advantage, due to the duration of stay in the day unit. As polychemotherapy could induce a bias, only patients receiving monotherapy were included in this study.
Over time, cycles were considered similar in terms of cost, and assessment was therefore made at a single time point. However, it would be interesting to take account of the full course of cycles, notably to evaluate quality of life. To date, few economic studies have been conducted on the impact of the SC formulation of rituximab in real life. The study by Rule et al., in the UK, compared costs associated with the active HCP time (nurse, pharmaceutical staff) for the preparation and administration of SC and IV rituximab under several scenarios, without taking account of the cost of the drug and medical devices. The authors reported a gain of 174.8 min and £115.17 (€134) per cycle for SC rituximab. However, when only the active presence of nurses was taken into account, the gain fell to 30.9 min and £15.22 (€17) [13]. This is in line with the present results (gain of 17.1 min and €12 with SC rituximab). The international study by De Cock et al., conducted in 30 day oncology units, showed a mean savings of 11.3 min (32%) in active HCP time for SC versus IV rituximab, ranging from 27 to 58% in European countries. The mean time-saving in France was 18.2 min (43%), which is consistent with the present results [24]. With a study design similar to ours, Mihajlovic et al. recently showed in the Netherlands a difference of €265.17 between the two formulations in terms of direct costs [25]. A similar comparison between IV and SC trastuzumab showed equivalent results, findings a medical cost reduction of €101 (drug, materials, and nurse time), and a majority of patients preferring SC over IV administration [26]. Although those European studies cannot be directly compared to our results, similar trends have been observed.
The SC formulation saves time for patients, as previously noted. However, the present study underlined the lack of dedicated organization in day units and pharmaceutical preparation units for the SC route. Unlike in clinical trials, mean day unit stay was as long for patients with SC rituximab as with the IV form in clinical practice. This was confirmed in the nurses’ interviews. With the SC form, patients expected to be treated faster, that is why wait times seemed longer. In this real-life study, no specific process dedicated to the SC formulation had been set up in the SC center, whereas one of the two IV hospitals had developed anticipated chemotherapy preparations of IV rituximab (i.e., realization of the preparation before the patient is hospitalized). To improve patient care, SC formulations have to be associated to a change in the organization of care. To minimize the waiting period, patient pathway should be optimized: doctor’s visit on arrival, anticipated preparation of chemotherapy, and dedicated nurses for outpatients with SC drugs. Thus, although SC formulation is an innovation, its use should be optimized in the real life.
There are several limitations to the present study. Following the referencing of SC rituximab in Lyon hospital, almost all patients with rituximab prescriptions had switched to the SC formulation, making it impossible to set up a control group within this hospital; the control group was therefore constituted with patients from two other centers. This design cannot exclude potential bias related to organizational differences between centers: e.g., active HCP time may vary depending on the hospital and equipment (hoods or isolators), how busy the staffs are, and patient characteristics. The demographic characteristics of patients in both cohorts were similar to those of the general population of patients with follicular lymphoma (between 50 and 60 years old and predominantly male), although there were more men and more patients in second-line treatment in the IV than in the SC group, which may have affected results for patients’ perception. Data collection was not performed by the same person in the three institutions, but the beginning and end of each task were defined before the start of the study and specified clearly to all centers. Larger patient recruitment would have increased the power of the results. On the other hand, data were collected on an individual basis, which strengthened the quality of the results. Nevertheless, these pharmacoeconomic results should be translated carefully to another country as drugs costs differ in Europe.
Conclusion
This cost-consequence analysis showed an economic gain from the hospital’s point of view for SC rituximab as maintenance monotherapy as compared to IV rituximab in patients with follicular lymphoma. Thus, taking account of their similar clinical efficacy, SC rituximab has a favorable pharmacoeconomic profile. Even though the subcutaneous form was preferred by almost all patients, consideration must be given to further optimizing the procedure for patients: a dedicated day unit with trained medical, nursing, and pharmaceutical staff could be advantageous.
References
Monnereau A, Remontet L, Maynadié M, et al (2013) Lymphome folliculaire. In: Estim. Natl. L’incidence Cancers En Fr. Entre 1980 2012 Partie 2—Hémopathies Malignes. Institut de Veille Sanitaire, Saint Maurice (Fra), p 24–27
Sant M, Allemani C, Tereanu C et al (2010) Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood 116:3724–3734
Tan D, Horning SJ, Hoppe RT et al (2013) Improvements in observed and relative survival in follicular grade 1-2 lymphoma during 4 decades: the Stanford University experience. Blood 122:981–987
Zinzani PL, Marchetti M, Billio A et al (2013) SIE, SIES, GITMO revised guidelines for the management of follicular lymphoma. Am J Hematol 88:185–192
Dreyling M, Ghielmini M, Rule S et al (2016) Newly diagnosed and relapsed follicular lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 27:v83–v90
Salles G, Seymour JF, Offner F et al (2011) Rituximab maintenance for 2 years in patients with high tumour burden follicular lymphoma responding to rituximab plus chemotherapy (PRIMA): a phase 3, randomised controlled trial. Lancet Lond Engl 377:42–51
Vidal L, Gafter-Gvili A, Salles G et al (2011) Rituximab maintenance for the treatment of patients with follicular lymphoma: an updated systematic review and meta-analysis of randomized trials. J Natl Cancer Inst 103:1799–1806
Salles GA, Seymour JF, Feugier P, et al (2013) Updated 6 year follow-up of the PRIMA study confirms the benefit of 2-year rituximab maintenance in follicular lymphoma patients responding to frontline immunochemotherapy. In: Blood. New Orleans, p 21
Shpilberg O, Jackisch C (2013) Subcutaneous administration of rituximab (MabThera) and trastuzumab (Herceptin) using hyaluronidase. Br J Cancer 109:1556–1561
F. Hoffmann-La Roche RCP MabThera SC. https://www.roche.fr/content/dam/roche_france/fr_FR/doc/Produits/Mabthera/MABTH1400IN_160526rcp.pdf. Accessed 11 Aug 2016
Davies A, Mihaljevi B, Marcadal S, et al (2015) Comparison of subcutaneous and intravenous rituximab in the maintenance setting: updated safety results of the phase III SABRINA study in patients with follicular lymphoma. EHA Learning Center. https://learningcenter.ehaweb.org/eha/2015/20th/100828. Accessed 4 Jan 2016
Davies A, Merli F, Mihaljevic B et al (2014) Pharmacokinetics and safety of subcutaneous rituximab in follicular lymphoma (SABRINA): stage 1 analysis of a randomised phase 3 study. Lancet Oncol 15:343–352
Rule S, Collins GP, Samanta K (2014) Subcutaneous vs intravenous rituximab in patients with non-Hodgkin lymphoma: a time and motion study in the United Kingdom. J Med Econ 17:459–468
Brédart A, Dolbeault S (2005) Évaluation de la qualité de vie en oncologie: I—Définitions et objectifs. Rev Francoph Psycho-Oncol 4:7–12
Department of Economics and Public Health Assessment (2012) Choices in methods for economic evaluation. https://www.has-sante.fr. Accessed 25 Sept 2015
Collège des économistes de la santé (CES) (2004) French guidelines for the economic evaluation of healthcare technologies: methodological recommendations 1–90
Chevalier J, de Pouvourville G (2013) Valuing EQ-5D using time trade-off in France. Eur J Health Econ HEPAC Health Econ Prev Care 14:57–66
Rovira J, Espín J, García L, Olry de Labry A (2011) The impact of biosimilars’ entry in the EU market. Andal Sch Pub Health 30:1–83
Lieutenant V, Toulza É, Pommier M, Lortal-Canguilhem B (2015) Herceptin® (trastuzumab) par voie sous-cutanée : une mini révolution ? Étude pharmaco-économique. Bull Cancer (Paris) 102:270–276
Cesarec A, Likić R (2017) Budget Impact Analysis of Biosimilar Trastuzumab for the Treatment of Breast Cancer in Croatia. Appl Health Econ Health Policy 15:277-286. https://doi.org/10.1007/s40258-016-0285-7
Rummel M, Kim TM, Aversa F et al (2017) Preference for subcutaneous or intravenous administration of rituximab among patients with untreated CD20+ diffuse large B-cell lymphoma or follicular lymphoma: results from a prospective, randomized, open-label, crossover study (PrefMab). Ann Oncol 28:836–842
Deconinck E, Miadi-Fargier H, Pen CL, Brice P (2010) Cost effectiveness of rituximab maintenance therapy in follicular lymphoma: long-term economic evaluation. PharmacoEconomics 28:35–46
Witzens-Harig M, Reiz M, Heiss C et al (2009) Quality of life during maintenance therapy with the anti-CD20 antibody rituximab in patients with B cell non-Hodgkin’s lymphoma: results of a prospective randomized controlled trial. Ann Hematol 88:51–57
Cock ED, Kritikou P, Tao S et al (2013) Time savings with rituximab subcutaneous (SC) injection vs rituximab intravenous (IV) infusion: final analysis from a time-and-motion study in 8 countries. Blood 122:1724–1724
Mihajlović J, Bax P, van Breugel E et al (2017) Microcosting study of rituximab subcutaneous injection versus intravenous infusion. Clin Ther 39:1221–1232.e4. https://doi.org/10.1016/j.clinthera.2017.05.342
Olofsson S, Norrlid H, Karlsson E et al (2016) Societal cost of subcutaneous and intravenous trastuzumab for HER2-positive breast cancer—an observational study prospectively recording resource utilization in a Swedish healthcare setting. Breast Edinb Scotl 29:140–146
Acknowledgements
We would like to acknowledge the medical, pharmaceutical, and nursing teams of the three centers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This study was carried out in line with the Declaration of Helsinki, French regulations, and institutional guidelines; given the nature of this research, no ethics committee approval was needed.
Informed consent
For this type of study, formal consent is not required. An information note, in which the whole project was explained, was given and explained to patients before interview.
Rights and permissions
About this article
Cite this article
Fargier, E., Ranchon, F., Huot, L. et al. SMABcare study: subcutaneous monoclonal antibody in cancer care: cost-consequence analysis of subcutaneous rituximab in patients with follicular lymphoma. Ann Hematol 97, 123–131 (2018). https://doi.org/10.1007/s00277-017-3147-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-017-3147-y