Abstract
Objective
To investigate the diagnostic contribution of T2-w nerve lesions and of muscle denervation in peripheral motor neuropathies by magnetic resonance neurography (MRN).
Methods
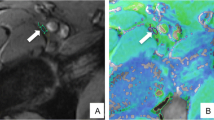
Fifty-one patients with peripheral motor neuropathies underwent high-resolution MRN by large coverage axial T2-w sequences of the upper arm, elbow, and forearm. Images were evaluated by two blinded readers for T2-w signal alterations of median, ulnar, and radial nerves, and for denervation in respective target muscle groups.
Results
All 51 patients displayed nerve lesions in at least one of three nerves, and 43 out of 51 patients showed denervation in at least one target muscle group of these nerves. In 21 out of 51 patients, the number of affected nerves matched the number of affected target muscle groups. In the remaining 30 patients, T2-w lesions were encountered more frequently than target muscle group denervation. In 153 nerve-muscle pairs, 72 showed denervation, but only one had increased muscle signal without a lesion in the corresponding nerve.
Conclusions
MRN-based diagnosis of peripheral motor neuropathies is more likely by visualization of peripheral nerve lesions than by denervation in corresponding target muscles. Increased muscular T2-w signal without concomitant nerve lesions should raise suspicion of an etiology other than peripheral neuropathy.
Key Points
• In peripheral neuropathy, T2-w nerve lesions are more frequent than muscle denervation.
• Muscle denervation almost never occurs without detectable lesions in corresponding nerves.
• MRN-aided diagnosis of peripheral motor neuropathy should focus primarily on nerve lesions.
• Increased muscular T2-w signal intensity without concomitant nerve lesions indicates other aetiology.





Similar content being viewed by others
References
Briani C, Cacciavillani M, Lucchetta M, Cecchin D, Gasparotti R (2013) MR neurography findings in axonal multifocal motor neuropathy. J Neurol 260:2420–2422
Kikuchi Y, Nakamura T, Takayama S, Horiuchi Y, Toyama Y (2003) MR imaging in the diagnosis of denervated and reinnervated skeletal muscles: experimental study in rats. Radiology 229:861–867
Polak JF, Jolesz FA, Adams DF (1988) Magnetic resonance imaging of skeletal muscle. Prolongation of T1 and T2 subsequent to denervation. Invest Radiol 23:365–369
Kim SJ, Hong SH, Jun WS et al (2011) MR imaging mapping of skeletal muscle denervation in entrapment and compressive neuropathies. Radiographics 31:319–332
Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D (2006) Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics 26:1267–1287
Yamabe E, Nakamura T, Oshio K, Kikuchi Y, Ikegami H, Toyama Y (2008) Peripheral nerve injury: diagnosis with MR imaging of denervated skeletal muscle —experimental study in rats. Radiology 247:409–417
Lisle DA, Johnstone SA (2007) Usefulness of muscle denervation as an MRI sign of peripheral nerve pathology. Australas Radiol 51:516–526
Thawait SK, Chaudhry V, Thawait GK et al (2011) High-resolution MR neurography of diffuse peripheral nerve lesions. Am J Neuroradiol 32:1365–1372
Stoll G, Bendszus M, Perez J, Pham M (2009) Magnetic resonance imaging of the peripheral nervous system. J Neurol 256:1043–1051
Andreisek G, Burg D, Studer A, Weishaupt D (2008) Upper extremity peripheral neuropathies: role and impact of MR imaging on patient management. Eur Radiol 18:1953–1961
Bendszus M, Stoll G (2005) Technology insight: visualizing peripheral nerve injury using MRI. Nat Clin Pract Neurol 1:45–53
Koltzenburg M, Bendszus M (2004) Imaging of peripheral nerve lesions. Curr Opin Neurol 17:621–626
Baumer P, Mautner VF, Baumer T et al (2013) Accumulation of non-compressive fascicular lesions underlies NF2 polyneuropathy. J Neurol 260:38–46
Bäumer P, Dombert T, Staub F, Kaestel T, Bartsch AJ, Heiland S, Bendszus M, Pham M (2011) Ulnar neuropathy at the elbow MR neurography–nerve T2 signal increase and caliber. Radiology 260
Pham M, Oikonomou D, Baumer P et al (2011) Proximal neuropathic lesions in distal symmetric diabetic polyneuropathy: findings of high-resolution magnetic resonance neurography. Diabetes Care 34:721–723
Pham M, Baumer P, Meinck HM et al (2014) Anterior interosseous nerve syndrome: fascicular motor lesions of median nerve trunk. Neurology 82:598–606
Baumer P, Weiler M, Ruetters M et al (2012) MR neurography in ulnar neuropathy as surrogate parameter for the presence of disseminated neuropathy. PLoS One 7:e49742
Vucic S, Black K, Chong PS, Cros D (2007) Multifocal motor neuropathy with conduction block: distribution of demyelination and axonal degeneration. Clin Neurophysiol 118:124–130
Suarez GA (2005) Chapter 102 - Immune Brachial Plexus Neuropathy. In: Dyck PJ, Thomas PK (eds) Peripheral Neuropathy (Fourth Edition). W.B. Saunders, Philadelphia, pp 2299–2308
Wilbourn AJ, Aminoff MJ (1998) AAEM minimonograph 32: the electrodiagnostic examination in patients with radiculopathies. Muscle Nerve 21:1612–1631
Aminoff MJ, Goodin DS, Parry GJ, Barbaro NM, Weinstein PR, Rosenblum ML (1985) Electrophysiologic evaluation of lumbosacral radiculopathies: electromyography, late responses and somatosensory evoked potentials. Neurology 35:1514–1518
McDonald CM, Carter GT, Fritz RC, Anderson MW, Abresch RT, Kilmer DD (2000) Magnetic resonance imaging of denervated muscle: comparison to electromyography. Muscle Nerve 23:1431–1434
Kastel T, Heiland S, Baumer P, Bartsch AJ, Bendszus M, Pham M (2011) Magic angle effect: a relevant artifact in MR neurography at 3 T? AJNR Am J Neuroradiol 32:821–827
Ferdinand BD, Rosenberg ZS, Schweitzer ME et al (2006) MR imaging features of radial tunnel syndrome: initial experience. Radiology 240:161–168
England JD, Asbury AK (2004) Peripheral neuropathy. Lancet 363:2151–2161
Viddeleer AR, Sijens PE, van Ooyen PM, Kuypers PD, Hovius SE, Oudkerk M (2012) Sequential MR imaging of denervated and reinnervated skeletal muscle as correlated to functional outcome. Radiology 264:522–530
Deroide N, Bousson V, Daguet E et al (2012) Muscle magnetic resonance imaging sensitivity does not decrease in chronic, mild, or proximal lower limb neuropathies. Muscle Nerve 45:659–667
Viallon M, Vargas MI, Jlassi H, Lovblad KO, Delavelle J (2008) High-resolution and functional magnetic resonance imaging of the brachial plexus using an isotropic 3D T2 STIR (Short Term Inversion Recovery) SPACE sequence and diffusion tensor imaging. Eur Radiol 18:1018–1023
Acknowledgments
The scientific guarantor of this publication is Dr. med. Philipp Bäumer, Department of Neuroradiology, Heidelberg University Hospital, Germany. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, diagnostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Clinical data for all patients. Detailed overview of clinical and demographic data of the patient collective. The functional specification of the symptom is followed by the respective MRC grading in brackets. Symptoms are listed in ascending MRC grading order. Muscles are abbreviated as follows: M. brachioradialis (BR), extensor carpi radialis (longus and brevis) (ECR), extensor digitorum communis (EDC), extensor indicis (EI), extensor carpi ulnaris (ECU), pronator teres (PT), flexor carpi ulnaris (FCU), flexor digitorum profundus (FDP), flexor carpi radialis (FCR), pronator quadratus (PQ), flexor pollicis longus (FPL), flexor pollicis brevis (FPB), abductor pollicis brevis (APB), opponens pollicis (OP), abductor digiti minimi (ADM), interosseous dorsalis (IDM). Electrophysiological abbreviations are: motor unit action potential (MUAP), compound muscle action potential (CMAP), sensory nerve action potential (SNAP), distal motor latency (dml), proximal motor latency (pml), sensory evoked potentials (SEP). The following (sixth) column states the corresponding diagnosis, and the seventh column lists the respective interval of time between onset of clinical symptoms and MR neurography. The penultimate column informs about additional MR sequences performed that were not routinely included in the protocol of the study. The last column shows the assigned group of every patient after evaluation of acquired images. At the bottom, the total numbers of male and female patients, the mean age, and the median and mean time delay between onset of clinical symptoms and MR neurography are given. (JPEG 4850 kb)
Rights and permissions
About this article
Cite this article
Schwarz, D., Weiler, M., Pham, M. et al. Diagnostic Signs of Motor Neuropathy in MR Neurography: Nerve Lesions and Muscle Denervation. Eur Radiol 25, 1497–1503 (2015). https://doi.org/10.1007/s00330-014-3498-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3498-x