Abstract
Purpose
To evaluate the influence of temporal resolution (TR) on cardiogenic artefacts at the level of bronchial walls.
Material and methods
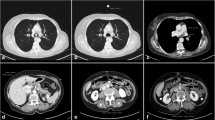
Ninety patients underwent a dual-source, single-energy chest CT examination enabling reconstruction of images with a TR of 75 ms (i.e., optimized TR) (Group 1) and 140 ms (i.e., standard TR) (Group 2). Cardiogenic artefacts were analyzed at the level of eight target bronchi, i.e., right (R) and left (L) B1, B5, B7, and B10 (total number of bronchi examined: n = 720).
Results
Cardiogenic artefacts were significantly less frequent and less severe in Group 1 than in Group 2 (p < 0.0001) with the highest scores of discordant ratings for bronchi in close contact with cardiac cavities: RB5 (61/90; 68 %); LB5 (66/90; 73 %); LB7 (63/90; 70 %). In Group 1, 78 % (560/720) of bronchi showed no cardiac motion artefacts, whereas 22 % of bronchi (160/720) showed artefacts rated as mild (152/160; 95 %), moderate (7/160; 4 %), and severe (1/160; 1 %). In Group 2, 70 % of bronchi (503/720) showed artefacts rated as mild (410/503; 82 %), moderate (82/503; 16 %), and severe (11/503; 2 %).
Conclusion
At 75 ms, most bronchi can be depicted without cardiogenic artefacts.
Key Points
• Quantitative CT helps analyze morphologic changes in COPD patients
• Cardiogenic artefacts may hamper precise analysis of bronchial dimensions
• Temporal resolution of CT acquisitions is an important parameter for bronchial imaging




Similar content being viewed by others
References
Diaz AA, Han MK, Come CE, Estepar RSJ, Ross JC, Kim V et al (2013) Effect of emphysema on CT scan measures of airway dimensions in smokers. Chest 143:687–693
Wielpütz MO, Eichinger M, Weinheimer O, Ley S, Mall MA, Wiebel M et al (2013) Automatic airway analysis on multidetector computed tomography in cystic fibrosis. J Thorac Imaging 28:104–113
Lederlin M, Laurent F, Portron Y, Ozier A, Cochet H, Berger P et al (2012) CT attenuation of the bronchial wall in patients with asthma: comparison with geometric parameters and correlation with function and histologic characteristics. AJR 199:1226–1233
Koschiuch J, Krenke R, Gorska K et al (2009) Relationships between airway wall thickness assessed by high-resolution comoted tomography and lung function in patients with asthma and chronic obstructive pulmonary disease. J Physiol Pharmacol 60(Suppl 5):71–76
Montaudon M, Berger P, de Dietrich G, Braquelaire A, Marthan R, Tunon-de-Lara JM et al (2007) Assessment of airways with three-dimensional quantitative thin-section CT: in vitro and in vivo validation. Radiology 242:563–572
Brillet PY, Fetita CI, Capderou A, Mitrea M, Dreuil S, Simon JM et al (2009) Variability of bronchial measurements obtained by sequential CT using two computer-based methods. Eur Radiol 19:1139–1147
Tacelli N, Remy-Jardin M, Flohr T, Faivre JB, Delannoy V, Duhamel A et al (2010) Dual-source chest CT angiography with high temporal resolution and high pitch modes: evaluation of image quality in 140 patients. Eur Radiol 20:1188–1196
Boyden EA (1955) Segmental anatomy of the lungs: a study of the patterns of the segmental bronchi and related pulmonary vessels. Mc Graw Hill, New York
Kelly DM, Hasegawa I, Borders R, Hatabu H, Boiselle PM (2004) High-resolution using MDCT: comparison of degree of motion artefact between volumetric and axial methods. AJR 182:757–759
Landis JR, Koch GG (1977) The measurement of interobserver agreement for categorical data. Biometrics 33:159–174
Montaudon M, Berger P, Cangini-Sacher A, de Dietrich G, Tunon-de-Lara JM, Marthan R et al (2007) Bronchial measurement with three-dimensional quantitative thin-section CT in patients with cystic fibrosis. Radiology 242:573–581
Nakano Y, Muller NL, King GG et al (2002) Quantitative assessment of airway remodelling using high-resolution CT. Chest 122:271S–275S
Berger P, Perot V, Desbarats P, Tunon-de-Lara JM, Marthan R, Laurent F (2005) Airway wall thickness in cigarette smokers: quantitative thin-section CT assessment. Radiology 235:1055–1064
Hasegawa M, Nasuhara Y, Onodera Y, Makita H, Nagai K, Fuke S et al (2006) Airflow limitation and airway dimensions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 173:1309–1315
Matsumoto H, Niimi A, Tabuena RP, Takemura M, Ueda T, Yamaguchi M et al (2007) Airway wall thickening in patients with cough variant asthma and nonasthmatic chronic cough. Chest 131:1042–1049
Yamashiro T, Matsuoka S, Estepar RSJ, Dransfield MT, Diaz A, Reilly JJ et al (2010) Quantitative assessment of bronchial wall attenuation with thin-section CT: an indicator of airflow limitation in chronic obstructive pulmonary disease. AJR 195:363–369
Brillet PY, Grenier PA, Fetita CI, Beigelman-Aubry C, Ould-Hmeidi Y, Ortner M et al (2013) Relationship between the airway wall area and asthma control score in moderate persistent asthma. Eur Radiol 23:1594–1602
Brillet PY, Fetita CI, Beigelman-Aubry C, Saragaglia A, Perchet D, Preteux F et al (2007) Quantification of bronchial dimensions at MDCT using dedicated software. Eur Radiol 17:1483–1489
Koyama H, Ohno Y, Nishio M et al (2014) Iterative reconstruction technique vs filtered back projection: utility for quantitative bronchial assessment on low-dose thin-section MDCT in patients with/without chronic obstructive pulmonary disease. Eur Radiol 24:1860–1867
Sasaki T, Takahashi K, Takada N, Ohsaki Y (2014) Ratios of peripheral-to-central airway lumen area and percentage wall area as predictors of severity of chronic obstructive pulmonary disease. AJR 203:78–84
Gupta S, Siddiqui S, Haldar P, Entwisle JJ, Mawby D, Wardlaw AJ et al (2010) Quantitative analysis of high-resolution computed tomography scans in severe asthma subphenotypes. Thorax 65:775–781
Takahashi M, Okada H, Oguni N, Maeda K, Segawa K, Nitta N et al (2011) How accurate is CT morphometry of airway? Phantom and clinical validation study. Eur J Radiol 80:e524–e530
Xie XQ, de Jong PA, Oudkerk M, Wang Y, Ten Hacken NHT, Miao J et al (2012) Morphological measurements in computed tomography correlate with airflow obstruction in chronic obstructive pulmonary disease: systematic review and meta-analysis. Eur Radiol 22:2085–2093
Deveci F, Murat A, Turgut T et al (2004) Airway wall thickness in patients with COPD and healthy non-smokers: assessment with high resolution computed tomographic scanning. Respiration 71:602–610
Kim SS, Seo JB, Lee HY, Nevrekar DV, Forssen AV, Crapo JD et al (2013) Chronic obstructive pulmonary disease: lobe-based visual assessment of volumetric CT by using standard images – Comparison with quantitative CT and pulmonary function test in the COPDGene study. Radiology 266:626–635
Yanagawa M, Tomiyama N, Sumikawa H, Inoue A, Daimon T, Honda O et al (2009) Thin-section CT of lung ECG gating: 64-detector row CT can markedly reduce cardiac motion artefact which can simulate lung lesions. Eur J Radiol 69:102–107
Pansini V, Remy-Jardin M, Tacelli N, Faivre JB, Flohr T, Deken V et al (2008) Screening for coronary artery disease in respiratory patients : comparison of single- and dual-source CT in patients with a heart rate above 70 bpm. Eur Radiol 16:2108–2119
Petersen J, Wille MM, Rakêt LL et al (2014) Effect of inspiration on airway dimensions measured at maximal inspiration CT images of subjects without airflow limitation. Eur Radiol 24:2319–2325
Montaudon M, Lederlin M, Reich S, Begueret H, Tunon-de-Lara JM, Marthan R et al (2009) Bronchial measurements in patients with asthma: comparison of quantitative thin-section CT findings with those in Healthy subjects and correlation with pathologic findings. Radiology 253:844–852
Flohr T, Leng S, Yu L, Aiimendinger T, Bruder H, Petersilka M et al (2009) Dual-source spiral CT with pitch up to 3.2 and 75 ms temporal resolution: Image reconstruction and assessment of image quality. Med Phys 36:5641–5653
Acknowledgments
The scientific guarantor of this publication is Martine Remy-Jardin, MD, PhD. The authors of this manuscript declare relationships with the following companies: Thomas Flohr, PhD, is a Siemens employee Jacques Remy, MD, is consultant for Siemens. Martine Remy-Jardin, MD, PhD, received technological support for clinical research. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
The authors state that this work has not received any funding. One of the authors, Alain Duhamel, PhD, Professor of Biomedical Statistics at the University Centre of Lille, has significant statistical expertise. He supervised statistical analyses and reviewed the manuscript. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
We reconstructed two different sets of CT images from the same CT raw data with an off-line reconstruction running on a separate PC (ReconCT version 8.5; Siemens Healthcare, Forchheim, Germany). The first reconstruction corresponded to the standard reconstruction implemented on the dual-source CT; the second one provided optimized temporal resolution. For image reconstruction of the dual-source CT data acquired at pitch 2, an angular range of 180° of CT raw data per measurement system (in parallel geometry) is available for each image close to the isocenter of the CT system [30]. In the standard filtered back-projection reconstruction, all scan data available per image contribute to the final image, i.e. the full angular range of 180°. This type of image reconstruction which we used to generate the first set of CT images is beneficial for complete utilization of the applied radiation dose, but it is sub-optimal with regard to optimized temporal resolution. A scan data range of 180° corresponds to a temporal resolution of 140 ms at 0.28 s gantry rotation time. We obtained the second set of images with an alternative off-line reconstruction which uses only the minimum scan data range of 90° (in parallel geometry) per measurement system for each image. By doing so, only a sub-range of the available CT data contributes to each image. This approach is sub-optimal with regard to dose utilization, but it provides images with the best possible temporal resolution of 75 ms. It is fully equivalent to the image reconstruction that would have been used on the scanner if the scan data had been acquired at a higher pitch of 3.2. Reconstructing both image data sets allows for an assessment of the effect of improved temporal resolution on bronchial wall imaging. Please note that the temporal resolution may vary with increasing distance from the iso-centre, but since we are looking at lung structures close to the heart, we think valid to only consider temporal resolution at iso-centre.
Rights and permissions
About this article
Cite this article
Hutt, A., Tacelli, N., Faivre, JB. et al. Is bronchial wall imaging affected by temporal resolution? comparative evaluation at 140 and 75 ms in 90 patients. Eur Radiol 26, 469–477 (2016). https://doi.org/10.1007/s00330-015-3819-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3819-8