Abstract
Objectives
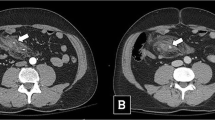
To evaluate the performance of an early repeated computed tomography (rCT) in initially non-operated patients with blunt bowel and mesenteric injuries (BBMI).
Methods
This was a monocentric retrospective observational study from 2009 to 2017 of patients with a BBMI on initial CT (iCT). Patients initially non-operated on were scheduled for a rCT within 48 h. Initial CT and rCT diagnostic performance were compared based on a surgical injury prediction score previously described. For statistical analysis, we used the chi-square analyses for paired data (McNemar test).
Results
Eighty-four patients (1.9% of trauma) had suspected BBMI on iCT. Among these patients, 22 (26.2%) were initially operated on, 18 (21.4%) were later operated on, and 44 (52.4%) were not operated on. The therapeutic laparotomy rate was 85%. Thirty-four patients initially non-operated on had a rCT. The absolute value of the CT scan score increased for 15 patients (44.1%). The early rCT diagnostic performance, compared with iCT, showed an increase in sensitivity (from 63.6 to 91.7%), in negative predictive value (from 77.4 to 94.7%), and in AUC (from 0.77 to 0.94).
Conclusion
In initially non-operated patients with BBMI lesions, the performance of an early rCT improved the sensitivity of lesion detection requiring surgical repair and the security of patient selection for non-operative treatment.
Key Points
• Selective non-operative treatment for hemodynamically stable patients with blunt bowel and/or mesenteric injuries on CT is developing but remains controversial.
• An early repeated CT improved the sensitivity of lesion detection requiring surgical repair and the security of patient selection for conservative treatment.




Similar content being viewed by others
Abbreviations
- −LR:
-
Negative likelihood ratio
- +LH:
-
Positive likelihood ratio
- AIS:
-
Abbreviated injury scale
- AUC:
-
Area under the curve
- BBMI:
-
Blunt bowel and/or mesenteric injury
- BIPS:
-
Bowel injury prediction score
- FOV:
-
Field of view
- iCT:
-
Initial computed tomography
- IQR:
-
Interquartile range
- ISS:
-
Injury severity score
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- rCT:
-
Early repeated computed tomography
- ROC:
-
Receiver operating characteristic
- Se:
-
Sensibility
- Sp:
-
Specificity
References
Watts DD, Fakhry SM (2003) Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 Trauma Admissions from the EAST Multi-Institutional Trial. J Trauma 54:289–294. https://doi.org/10.1097/01.TA.0000046261.06976.6A
Pande R, Saratzis A, Winter Beatty J et al (2017) Contemporary characteristics of blunt abdominal trauma in a regional series from the UK. Ann R Coll Surg Engl 99:82–87. https://doi.org/10.1308/rcsann.2016.0223
McNutt MK, Chinapuvvula NR, Beckmann NM et al (2015) Early surgical intervention for blunt bowel injury: the Bowel Injury Prediction Score (BIPS). J Trauma Acute Care Surg 78:105–111. https://doi.org/10.1097/TA.0000000000000471
Zingg T, Agri F, Bourgeat M et al (2017) Avoiding delayed diagnosis of significant blunt bowel and mesenteric injuries: can a scoring tool make the difference? A 7-year retrospective cohort study. Injury. https://doi.org/10.1016/j.injury.2017.09.004
Bège T, Chaumoître K, Léone M et al (2014) Blunt bowel and mesenteric injuries detected on CT scan: who is really eligible for surgery? Eur J Trauma Emerg Surg 40:75–81. https://doi.org/10.1007/s00068-013-0318-y
Zarour A, El-Menyar A, Khattabi M et al (2014) A novel practical scoring for early diagnosis of traumatic bowel injury without obvious solid organ injury in hemodynamically stable patients. Int J Surg 12:340–345. https://doi.org/10.1016/j.ijsu.2014.01.011
Faget C, Taourel P, Charbit J et al (2015) Value of CT to predict surgically important bowel and/or mesenteric injury in blunt trauma: performance of a preliminary scoring system. Eur Radiol 25:3620–3628. https://doi.org/10.1007/s00330-015-3771-7
Inaba K, Okoye OT, Rosenheck R et al (2013) Prospective evaluation of the role of computed tomography in the assessment of abdominal stab wounds. JAMA Surg 148:810–816. https://doi.org/10.1001/jamasurg.2013.2521
Malinoski DJ, Patel MS, Yakar DO et al (2010) A diagnostic delay of 5 hours increases the risk of death after blunt hollow viscus injury. J Trauma 69:84–87. https://doi.org/10.1097/TA.0b013e3181db37f5
Fakhry SM, Watts DD, Luchette FA, EAST Multi-Institutional Hollow Viscus Injury Research Group (2003) CURRENT diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trial. J Trauma 54:295–306. https://doi.org/10.1097/01.TA.0000046256.80836.AA
Tan K-K, Liu JZ, Go T-S et al (2010) Computed tomography has an important role in hollow viscus and mesenteric injuries after blunt abdominal trauma. Injury 41:475–478. https://doi.org/10.1016/j.injury.2009.09.028
Petrosoniak A, Engels PT, Hamilton P, Tien HC (2013) Detection of significant bowel and mesenteric injuries in blunt abdominal trauma with 64-slice computed tomography. J Trauma Acute Care Surg 74:1081–1086. https://doi.org/10.1097/TA.0b013e3182827178
McCombie SP, Thyer I, Corcoran NM et al (2014) The conservative management of renal trauma: a literature review and practical clinical guideline from Australia and New Zealand: Conservative management of renal trauma. BJU Int 114:13–21. https://doi.org/10.1111/bju.12902
Goin G, Massalou D, Bege T et al (2017) Feasibility of selective non-operative management for penetrating abdominal trauma in France. J Visc Surg 154:167–174. https://doi.org/10.1016/j.jviscsurg.2016.08.006
Lawson CM, Daley BJ, Ormsby CB, Enderson B (2011) Missed injuries in the era of the trauma scan. J Trauma 70:452–458. https://doi.org/10.1097/TA.0b013e3182028d71
Eurin M, Haddad N, Zappa M et al (2012) Incidence and predictors of missed injuries in trauma patients in the initial hot report of whole-body CT scan. Injury 43:73–77. https://doi.org/10.1016/j.injury.2011.05.019
Saku M, Yoshimitsu K, Murakami J et al (2006) Small bowel perforation resulting from blunt abdominal trauma: interval change of radiological characteristics. Radiat Med 24:358–364. https://doi.org/10.1007/s11604-006-0042-1
Raharimanantsoa M, Zingg T, Thiery A et al (2017) Proposal of a new preliminary scoring tool for early identification of significant blunt bowel and mesenteric injuries in patients at risk after road traffic crashes. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-017-0893-4
Mitsuhide K, Junichi S, Atsushi N et al (2005) Computed tomographic scanning and selective laparoscopy in the diagnosis of blunt bowel injury: a prospective study. J Trauma 58:696–701 discussion 701–703
Sitnikov V, Yakubu A, Sarkisyan V, Turbin M (2009) The role of video-assisted laparoscopy in management of patients with small bowel injuries in abdominal trauma. Surg Endosc 23:125–129. https://doi.org/10.1007/s00464-008-9910-3
Matsumoto S, Sekine K, Funaoka H et al (2017) Early diagnosis of hollow viscus injury using intestinal fatty acid–binding protein in blunt trauma patients. Medicine (Baltimore) 96:e6187. https://doi.org/10.1097/MD.0000000000006187
Acknowledgments
The authors would like to thank the Proof-Reading-Service for editing.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Thierry Bege.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Laurent Boyer; Aix-Marseille University, Marseille, France; Public Health and Chronic Disease Research Unit, APHM, CHU Timone, Marseille, France) carried out the statistics of this study.
We used computer software (IBM SPSS Statistics, Version 20, USA and XLStat-Premium v.2018.3) to do the statistics.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lannes, F., Scemama, U., Maignan, A. et al. Value of early repeated abdominal CT in selective non-operative management for blunt bowel and mesenteric injury. Eur Radiol 29, 5932–5940 (2019). https://doi.org/10.1007/s00330-019-06212-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06212-w