Abstract
Objectives
Staging of upper extremity lymphedema is needed to guide surgical management, but is not standardized due to lack of accessible, quantitative, or precise measures. Here, we established an MRI-based staging system for lymphedema and validate it against existing clinical measures.
Methods
Bilateral upper extremity MRI and lymphoscintigraphy were performed on 45 patients with unilateral secondary lymphedema, due to surgical intervention, who were referred to our multidisciplinary lymphedema clinic between March 2017 and October 2018. MRI short-tau inversion recovery (STIR) images were retrospectively reviewed. A grading system was established based on the cross-sectional circumferential extent of subcutaneous fluid infiltration at three locations, labeled MRI stage 0–3, and was compared to L-Dex®, ICG lymphography, volume, lymphedema quality of life (LYMQOL), International Society of Lymphology (ISL) stage, and lymphoscintigraphy. Linear weighted Cohen’s kappa was calculated to compare MRI staging by two readers.
Results
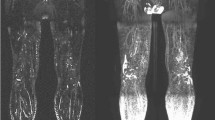
STIR images on MRI revealed a predictable pattern of fluid infiltration centered on the elbow and extending along the posterior aspect of the upper arm and the ulnar side of the forearm. Patients with higher MRI stage were more likely to be in ISL stage 2 (p = 0.002) or to demonstrate dermal backflow on lymphoscintigraphy (p = 0.0002). No correlation was found between MRI stages and LYMQOL. Higher MRI stage correlated with abnormal ICG lymphography pattern (rs = 0.63, p < 0.0001), larger % difference in limb volume (rs = 0.68, p < 0.0001), and higher L-Dex® ratio (rs = 0.84, p < 0.0001). Cohen’s kappa was 0.92 (95% CI, 0.85–1.00).
Conclusion
An MRI staging system for upper extremity lymphedema offers an improved non-invasive precision marker for lymphedema for therapeutic planning.
Key Points
• Diagnosis and staging of patients with secondary upper extremity lymphedema may be performed with non-contrast MRI, which is non-invasive and more readily accessible compared to lymphoscintigraphy and evaluation by lymphedema specialists.
• MRI-based staging of secondary upper extremity lymphedema is highly reproducible and could be used for long-term follow-up of patients.
• In patients with borderline clinical measurements, MRI can be used to identify patients with early-stage lymphedema.





Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- DB:
-
Dermal backflow
- ICG:
-
Indocyanine green
- ISL:
-
International Society of Lymphology
- LYMQOL:
-
Lymphedema Quality of Life
- MRI:
-
Magnetic resonance imaging
- QoL:
-
Quality of life
- STIR:
-
Short-tau inversion recovery
References
Nguyen TT, Hoskin TL, Habermann EB, Cheville AL, Boughey JC (2017) Breast cancer-related lymphedema risk is related to multidisciplinary treatment and not surgery alone: results from a large cohort study. Ann Surg Oncol 24(10):2972–2980. https://doi.org/10.1245/s10434-017-5960-x
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
Rockson SG (2018) Lymphedema after breast cancer treatment. N Engl J Med 379(20):1937–1944. https://doi.org/10.1056/NEJMcp1803290
Garza RM, Ooi ASH, Falk J, Chang DW (2018) The relationship between clinical and indocyanine green staging in lymphedema. Lymphat Res Biol. https://doi.org/10.1089/lrb.2018.0014
Lee TS, Morris CM, Czerniec SA, Mangion AJ (2018) Does lymphedema severity affect quality of life? Simple question. Challenging answers. Lymphat Res Biol 16(1):85–91. https://doi.org/10.1089/lrb.2016.0049
Patel KM, Lin C-Y, Cheng M-H (2015) A prospective evaluation of lymphedema-specific quality-of-life outcomes following vascularized lymph node transfer. Ann Surg Oncol 22(7):2424–2430. https://doi.org/10.1245/s10434-014-4276-3
Narushima M, Yamamoto T, Ogata F, Yoshimatsu H, Mihara M, Koshima I (2016) Indocyanine green lymphography findings in limb lymphedema. J Reconstr Microsurg 32(1):72–79. https://doi.org/10.1055/s-0035-1564608
Qin ES, Bowen MJ, Chen WF (2018) Diagnostic accuracy of bioimpedance spectroscopy in patients with lymphedema: a retrospective cohort analysis. J Plast Reconstr Aesthetic Surg 71(7):1041–1050. https://doi.org/10.1016/j.bjps.2018.02.012
Coroneos CJ, Wong FC, DeSnyder SM, Shaitelman SF, Schaverien MV (2018) Correlation of L-Dex bioimpedance spectroscopy with limb volume and lymphatic function in lymphedema. Lymphat Res Biol. https://doi.org/10.1089/lrb.2018.0028
Lohrmann C, Foeldi E, Speck O, Langer M (2006) High-resolution MR lymphangiography in patients with primary and secondary lymphedema. AJR Am J Roentgenol 187(2):556–561. https://doi.org/10.2214/AJR.05.1750
Notohamiprodjo M, Weiss M, Baumeister RG et al (2012) MR lymphangiography at 3.0 T: correlation with lymphoscintigraphy. Radiology 264(1):78–87. https://doi.org/10.1148/radiol.12110229
Cellina M, Oliva G, Menozzi A, Soresina M, Martinenghi C, Gibelli D (2019) Non-contrast magnetic resonance lymphangiography: an emerging technique for the study of lymphedema. Clin Imaging 53:126–133. https://doi.org/10.1016/j.clinimag.2018.10.006
Pappalardo M, Cheng M-H (2018) Abstract: a new lymphoscintigraphy staging for unilateral extremity lymphedema. Plast Reconstr Surg Glob Open 6:74–75. https://doi.org/10.1097/01.GOX.0000546918.33068.82
Hassanein AH, Maclellan RA, Grant FD, Greene AK (2017) Diagnostic accuracy of lymphoscintigraphy for lymphedema and analysis of false-negative tests. Plast Reconstr Surg Glob Open 5(7):e1396. https://doi.org/10.1097/GOX.0000000000001396
Dylke ES, McEntee MF, Schembri GP et al (2013) Reliability of a radiological grading system for dermal backflow in lymphoscintigraphy imaging. Acad Radiol 20(6):758–763. https://doi.org/10.1016/j.acra.2013.01.018
Yamamoto T, Yamamoto N, Doi K et al (2011) Indocyanine green–enhanced lymphography for upper extremity lymphedema: a novel severity staging system using dermal backflow patterns. Plast Reconstr Surg 128(4):941–947. https://doi.org/10.1097/PRS.0b013e3182268cd9
Franconeri A, Ballati F, Panzuto F et al (2020) A proposal for a semiquantitative scoring system for lymphedema using non-contrast magnetic resonance lymphography (NMRL): reproducibility among readers and correlation with clinical grading. Magn Reson Imaging 68:158–166. https://doi.org/10.1016/j.mri.2020.02.004
Arrivé L, Derhy S, Dahan B et al (2018) Primary lower limb lymphoedema: classification with non-contrast MR lymphography. Eur Radiol 28(1):291–300. https://doi.org/10.1007/s00330-017-4948-z
Arrivé L, Derhy S, Dlimi C, El Mouhadi S, Monnier-Cholley L, Becker C (2017) Noncontrast magnetic resonance lymphography for evaluation of lymph node transfer for secondary upper limb lymphedema. Plast Reconstr Surg 140(6):806e–811e. https://doi.org/10.1097/PRS.0000000000003862
van de Pas CB, Biemans AA, Boonen RS, Viehoff PB, Neumann HA (2016) Validation of the lymphoedema quality-of-life questionnaire (LYMQOL) in Dutch patients diagnosed with lymphoedema of the lower limbs. Phlebology 31(4):257–263. https://doi.org/10.1177/0268355515586312
Sty JR, Boedecker RA, Scanlon GT, Babbitt DP (1979) Radionuclide “dermal backflow” in lymphatic obstruction. J Nucl Med 20(8):905–906
Armer JM, Stewart BR (2005) A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol 3(4):208–217. https://doi.org/10.1089/lrb.2005.3.208
Sanders JE, Allyn KJ, Harrison DS, Myers TR, Ciol MA, Tsai EC (2012) Preliminary investigation of residual-limb fluid volume changes within one day. J Rehabil Res Dev 49(10):1467–1478
Mitsumori LM, McDonald ES, Neligan PC, Maki JH (2016) Peripheral magnetic resonance lymphangiography: techniques and applications. Tech Vasc Interv Radiol 19(4):262–272. https://doi.org/10.1053/j.tvir.2016.10.007
Mihara M, Hara H, Araki J et al (2012) Indocyanine green (ICG) lymphography is superior to lymphoscintigraphy for diagnostic imaging of early lymphedema of the upper limbs. PLoS One 7(6):e38182. https://doi.org/10.1371/journal.pone.0038182
Case TC, Witte CL, Witte MH, Unger EC, Williams WH (1992) Magnetic resonance imaging in human lymphedema: comparison with lymphangioscintigraphy. Magn Reson Imaging 10(4):549–558
Czerniec SA, Ward LC, Kilbreath SL (2016) Breast cancer-related arm lymphedema: fluctuation over six months and the effect of the weather. Lymphat Res Biol 14(3):148–155. https://doi.org/10.1089/lrb.2015.0030
Ridner SH, Dietrich MS, Stewart BR, Armer JM (2011) Body mass index and breast cancer treatment-related lymphedema. Support Care Cancer 19(6):853–857. https://doi.org/10.1007/s00520-011-1089-9
Fu MR, Cleland CM, Guth AA et al (2013) L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology 46(2):85–96
Mehrara BJ, Greene AK (2014) Lymphedema and obesity: is there a link? Plast Reconstr Surg 134(1):154e–160e. https://doi.org/10.1097/PRS.0000000000000268
Zampell JC, Aschen S, Weitman ES et al (2012) Regulation of adipogenesis by lymphatic fluid stasis: part I. Adipogenesis, fibrosis, and inflammation. Plast Reconstr Surg 129(4):825–834. https://doi.org/10.1097/PRS.0b013e3182450b2d
Funding
This study has received funding by the RSNA R&E Resident Research Grant RR1820.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Geunwon Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Kim, G., Smith, M.P., Donohoe, K.J. et al. MRI staging of upper extremity secondary lymphedema: correlation with clinical measurements. Eur Radiol 30, 4686–4694 (2020). https://doi.org/10.1007/s00330-020-06790-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06790-0