Abstract
Objectives
To evaluate the relationship between imperceptible T1 enhancement of papillary renal cell carcinoma (pRCC) on MR and intratumoral hemosiderin deposition.
Methods
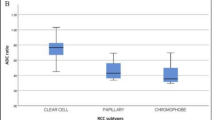
One hundred ten pRCCs (≤ 7 cm) were evaluated by MR with in- and opposed-phase spoiled gradient echo (GRE) and T1-weighted spoiled GRE with fat suppression before and after contrast. Hemosiderin deposition was assessed by SIindex and Dindex on in- and opposed-phase images. SIindex and Dindex are calculated as (SIin − SIopp)/(SIin) × 100, where SIin and SIopp are tumor signal intensities on in- and opposed-phase images and (Din)/(Dopp), where Din and Dopp are tumor diameters on in- and opposed-phase images, respectively. The degree of tumor enhancement was classified as grade 1 (no), grade 2 (subtle), or grade 3 (definite). Tumor enhancement on CT was assessed when available.
Results
Five (5%), 10 (9%), and 95 (86%) tumors were categorized as grades 1, 2, and 3 enhancement, respectively. The mean SIindex was − 33.9, − 25.3, and 1.00, whereas the mean Dindex was 1.26, 1.05, and 1.00 in tumors with grades 1, 2, and 3 enhancement, respectively. Tumors with grade 1 enhancement had significantly lower SIindex (p = 0.001) and higher Dindex (p = 0.005) than those with grade 3 enhancement. Among six tumors with grade 1 or 2 enhancement and available CT, four tumors showed > 20 HU enhancement.
Conclusions
pRCC with no subjective enhancement on contrast-enhanced MR showed hemosiderin deposition evident by lower SIindex and higher Dindex. Hemosiderin deposition might mask the tumor enhancement on MR.
Key Points
• 5% of papillary renal cell carcinoma showed imperceptible enhancement on contrast-enhanced MR.
• Hemosiderin deposition in papillary renal cell carcinoma might mask the tumor enhancement on contrast-enhanced MR due to T2/T2*-shortening effects.
• A renal lesion with extensive hemosiderin deposition but no perceptible enhancement on MR should be considered suspicious for papillary renal cell carcinoma.





Similar content being viewed by others
Abbreviations
- ER:
-
Enhancement ratio
- FSE:
-
Fast spin echo
- GRE:
-
Gradient echo
- ICC:
-
Interclass correlation coefficient
- pRCC:
-
Papillary renal cell carcinoma
- RCC:
-
Renal cell carcinoma
- ROI:
-
Region of interest
- SE:
-
Spin echo
- SI:
-
Signal intensity
References
Reuter VE (2006) The pathology of renal epithelial neoplasms. Semin Oncol 33:534–543
Mydlo JH, Bard RH (1987) Analysis of papillary renal adenocarcinoma. Urology 30:529–534
Vikram R, Ng CS, Tamboli P et al (2009) Papillary renal cell carcinoma: radiologic-pathologic correlation and spectrum of disease. Radiographics 29:741–754 discussion 755-747
Roy C, Sauer B, Lindner V, Lang H, Saussine C, Jacqmin D (2007) MR imaging of papillary renal neoplasms: potential application for characterization of small renal masses. Eur Radiol 17:193–200
Sun MR, Ngo L, Genega EM et al (2009) Renal cell carcinoma: dynamic contrast-enhanced MR imaging for differentiation of tumor subtypes--correlation with pathologic findings. Radiology 250:793–802
Young JR, Margolis D, Sauk S, Pantuck AJ, Sayre J, Raman SS (2013) Clear cell renal cell carcinoma: discrimination from other renal cell carcinoma subtypes and oncocytoma at multiphasic multidetector CT. Radiology 267:444–453
Jinzaki M, Tanimoto A, Mukai M et al (2000) Double-phase helical CT of small renal parenchymal neoplasms: correlation with pathologic findings and tumor angiogenesis. J Comput Assist Tomogr 24:835–842
Wingen M, Alzen G, Gunther RW (1998) MR imaging fails to detect bone marrow oedema in osteomyelitis: report of two cases. Pediatr Radiol 28:189–192
Roy C, El Ghali S, Buy X, Lindner V, Gangi A (2005) Papillary renal cell carcinoma in allograft kidney. Eur Radiol 15:661–665
Sussman SK, Glickstein MF, Krzymowski GA (1990) Hypointense renal cell carcinoma: MR imaging with pathologic correlation. Radiology 177:495–497
Yoshimitsu K, Kakihara D, Irie H et al (2006) Papillary renal carcinoma: diagnostic approach by chemical shift gradient-echo and echo-planar MR imaging. J Magn Reson Imaging 23:339–344
Egbert ND, Caoili EM, Cohan RH et al (2013) Differentiation of papillary renal cell carcinoma subtypes on CT and MRI. AJR Am J Roentgenol 201:347–355
Dilauro M, Quon M, McInnes MD et al (2016) Comparison of contrast-enhanced multiphase renal protocol CT versus MRI for diagnosis of papillary renal cell carcinoma. AJR Am J Roentgenol 206:319–325
Zand KR, Reinhold C, Haider MA, Nakai A, Rohoman L, Maheshwari S (2007) Artifacts and pitfalls in MR imaging of the pelvis. J Magn Reson Imaging 26:480–497
Wang S, Filipowicz EA, Schnadig VJ (2001) Abundant intracytoplasmic hemosiderin in both histiocytes and neoplastic cells: a diagnostic pitfall in fine-needle aspiration of cystic papillary renal-cell carcinoma. Diagn Cytopathol 24:82–85
Yan S, Chen Q, Zhang X et al (2016) Extensive blooming artifact predicts no recanalization after intravenous thrombolysis. Eur J Neurol 23:737–743
Bradley WG Jr (1993) MR appearance of hemorrhage in the brain. Radiology 189:15–26
Roubidoux MA (1994) MR imaging of hemorrhage and iron deposition in the kidney. Radiographics 14:1033–1044
McKee TC, Dave J, Kania L et al (2019) Are hemorrhagic cysts hyperintense enough on T1-weighted MRI to be distinguished from renal cell carcinomas? A retrospective analysis of 204 patients. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.19.21257:1-7
Davarpanah AH, Spektor M, Mathur M, Israel GM (2016) Homogeneous T1 hyperintense renal lesions with smooth borders: is contrast-enhanced MR imaging needed? Radiology 281:326
Yoshida K, Takahashi N, King BF et al (2019) Multiple unilateral subcapsular cortical hemorrhagic cystic disease of the kidney: CT and MRI findings and clinical characteristic. Eur Radiol 29:4843–4850
Herts BR, Silverman SG, Hindman NM et al (2018) Management of the incidental renal mass on CT: a white paper of the ACR Incidental Findings Committee. J Am Coll Radiol 15:264–273
Couvidat C, Eiss D, Verkarre V et al (2014) Renal papillary carcinoma: CT and MRI features. Diagn Interv Imaging 95:1055–1063
Ho VB, Allen SF, Hood MN, Choyke PL (2002) Renal masses: quantitative assessment of enhancement with dynamic MR imaging. Radiology 224:695–700
Hecht EM, Israel GM, Krinsky GA et al (2004) Renal masses: quantitative analysis of enhancement with signal intensity measurements versus qualitative analysis of enhancement with image subtraction for diagnosing malignancy at MR imaging. Radiology 232:373–378
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Naoki Takahashi.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in “Small (<4 cm) renal mass: differentiation of angiomyolipoma without visible fat from renal cell carcinoma utilizing MR imaging” in Radiology.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takahashi, H., Kawashima, A., Inoue, A. et al. Hemosiderin deposition in papillary renal cell carcinoma and its potential to mask enhancement on MRI: analysis of 110 cases. Eur Radiol 30, 6033–6041 (2020). https://doi.org/10.1007/s00330-020-06994-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06994-4