Abstract
Introduction
A pituicytoma in the sellar area is extremely rare in children and, due to its highly vascularized nature, can be difficult to address using the transsphenoid approach (TSA) to surgery. Here, we report a rare case of a pituicytoma that was completely removed from a child through a staged operation using the TSA.
Case summary
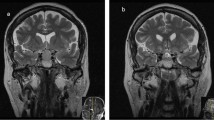
A 13-year-old girl was admitted with a 1-year history of visual disturbance and amenorrhea. Visual field examination showed left total blindness and right temporal hemianopsia. Laboratory results revealed hormonal levels all within normal ranges. Brain magnetic resonance imaging (MRI) showed a homogeneous, highly enhancing sellar and suprasellar mass, typically suggestive of a pituitary adenoma. TSA surgery revealed the tumor had a rubbery-firm consistency, hypervascularity, and profuse bleeding. We removed the tumor partially and planned a second-stage operation.
Discussion
Gross total removal is the treatment of choice for this type of tumor. Attempted resection of these presumed adenomas or meningiomas using the TSA often results in unexpectedly heavy intraoperative bleeding due to the high vascularity of this rare tumor, making surgery challenging, especially in children where the tumor is within a relatively narrow corridor. While pituicytomas are a rare differential diagnosis for sellar or parasellar tumors in children, total removal by second-stage TSA surgery is indicated in the case of profuse bleeding or uncertainty of biopsy. Following first-stage TSA surgery and pathologic confirmation of pituicytoma, the strategy is typically gross total removal during second-stage TSA surgery.
Conclusions
Although very rare in children, a pituicytoma should be included in the differential diagnosis of a mass in the sellar area if the tumor is highly enhancing or very vascular. Second-stage TSA surgery is another strategy when the pathology is not clear during the first-stage TSA surgery.



Similar content being viewed by others
References
Wolfe SQ, Bruce J, Morcos JJ (2008) Pituicytoma: case report. Neurosurgery 63:E173–174, discussion E174
Yilmaz O, Turan A, Yigit H, Duymus M, Kosar U (2012) Case of pituicytoma in childhood. Childs Nerv Syst 28:11–12
Louis DN, Ohgaki H, Weistler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (eds) (2007) WHO classification of tumours of the central nervous system. IARC Press, Lyon
Takei Y, Seyama S, Pearl GS, Tindall GT (1980) Ultrastructural study of the human neurohypophysis. II. Cellular elements of neural parenchyma, the pituicytes. Cell Tissue Res 205:273–287
Phillips JJ, Misra A, Feuerstein BG, Kunwar S, Tihan T (2010) Pituicytoma: characterization of a unique neoplasm by histology, immunohistochemistry, ultrastructure, and array-based comparative genomic hybridization. Arch Pathol Lab Med 134:1063–1069
Pirayesh Islamian A, Buslei R, Saeger W, Fahlbusch R (2012) Pituicytoma: overview of treatment strategies and outcome. Pituitary 15:227–236
Ulm AJ, Yachnis AT, Brat DJ, Rhoton AL Jr (2004) Pituicytoma: report of two cases and clues regarding histogenesis. Neurosurgery 54:753–757, discussion 757-758
Covington MF, Chin SS, Osborn AG (2011) Pituicytoma, spindle cell oncocytoma, and granular cell tumor: clarification and meta-analysis of the world literature since 1893. AJNR Am J Neuroradiol 32:2067–2072
Chakraborti S, Mahadevan A, Govindan A, Sridhar K, Mohan NV, Satish IR, Rudrappa S, Mangshetty S, Shankar SK (2013) Pituicytoma: report of three cases with review of literature. Pathol Res Pract 209:52–58
Hurley TR, D'Angelo CM, Clasen RA, Wilkinson SB, Passavoy RD (1994) Magnetic resonance imaging and pathological analysis of a pituicytoma: case report. Neurosurgery 35:314–317, discussion 317
Katsuta T, Inoue T, Nakagaki H, Takeshita M, Morimoto K, Iwaki T (2003) Distinctions between pituicytoma and ordinary pilocytic astrocytoma. Case report. J Neurosurg 98:404–406
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Cenacchi G, Giovenali P, Castrioto C, Giangaspero F (2001) Pituicytoma: ultrastructural evidence of a possible origin from folliculo-stellate cells of the adenohypophysis. Ultrastruct Pathol 25:309–312
Figarella-Branger D, Dufour H, Fernandez C, Bouvier-Labit C, Grisoli F, Pellissier JF (2002) Pituicytomas, a mis-diagnosed benign tumor of the neurohypophysis: report of three cases. Acta Neuropathol 104:313–319
Brat DJ, Scheithauer BW, Staugaitis SM, Holtzman RN, Morgello S, Burger PC (2000) Pituicytoma: a distinctive low-grade glioma of the neurohypophysis. Am J Surg Pathol 24:362–368
Gibbs WN, Monuki ES, Linskey ME, Hasso AN (2006) Pituicytoma: diagnostic features on selective carotid angiography and MR imaging. AJNR Am J Neuroradiol 27:1639–1642
Menon G, Easwer HV, Radhakrishnan VV, Nair S (2008) Symptomatic granular cell tumour of the pituitary. Br J Neurosurg 22:126–130
Zygourakis CC, Rolston JD, Lee HS, Partow C, Kunwar S, Aghi MK (2015) Pituicytomas and spindle cell oncocytomas: modern case series from the University of California, San Francisco. Pituitary 18:150–158
Brandao RA, Braga MH, de Souza AA, Reis BL, Faraj de Lima FB (2010) Pituicytoma. Surg Neurol Int 1:79
Acknowledgments
This work was supported by a National Research Foundation of Korea Grant funded by the Korean Government (NRF-2012R1A1A1042282).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, Y.G., Park, Y.S. Second-stage transsphenoidal approach (TSA) for highly vascular pituicytomas in children. Childs Nerv Syst 31, 985–989 (2015). https://doi.org/10.1007/s00381-015-2668-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2668-8