Abstract
Purpose
To describe the design, implementation, and adoption of a simplified electronic medical record (EMR) and its use in documenting pediatric central nervous system (CNS) tumors at a tertiary care referral hospital in South-East Asia.
Methods
A novel EMR, cataloguing pediatric CNS tumors was used to collect data from August 2017 to March 2020 at National Institute of Neurosciences and Hospital (NINS&H) in Dhaka, Bangladesh.
Results
Two hundred forty-nine pediatric patients with a CNS tumor were admitted to NINS&H. Fifty-eight percent of patients were male, and the median age was 8 years. A total of 188/249 patients (76%) underwent surgery during their index admission. Radiographic locations were known for 212/249 (85%) of cases; the most common radiographic locations were infratentorial (81/212; 38%), suprasellar (45/212; 21%), and supratentorial (29/212; 14%). A histopathological classification was reported on 156/249 (63%) of patients’ cytology. The most common infratentorial pathologies were medulloblastoma (22/47; 47%) and pilocytic astrocytoma (14/47; 30%). The median time between admission and surgery was 36 days, while the median post-operation stay was 19.5 days.
Conclusions
The feasibility of a basic EMR platform for a busy pediatric neurosurgery department in a lower-middle income country is demonstrated, and preliminary clinical data is reviewed. A wide variety of pediatric CNS tumors were observed, spanning the spectrum of anatomic locations and histopathologic subtypes. Surgical intervention was performed for the majority of patients. Barriers to care include limited molecular diagnostics and unavailable data on adjuvant therapy. Future targets include improvement of clinical documentation in the pre-operative and post-operative period.
Similar content being viewed by others
Introduction
Neurosurgeons, medical assistants, and auxiliary staff face many challenges — both clinically and organizationally — when managing hundreds of individuals’ neurosurgical care in a large tertiary referral center. Many institutions based in high-income countries (HICs) have utilized electronic medical records (EMRs) to maximize organizational efficiency [1, 2]. Alternatively, most hospitals based in low- and middle-income countries (LMICs) rely on paper-based documentation, thus providing fertile grounds for EMR adoption [3, 4]. While EMR implementation has been well-documented in various spheres in LMICs, no study to date has analyzed the impacts of EMR implementation on pediatric neurosurgical care in an LMIC neurosurgery department [4,5,6,7,8,9]. This study describes the design, implementation, and adoption of a novel EMR and its use in documenting pediatric central nervous system (CNS) tumors at a large national referral hospital in Dhaka, Bangladesh.
Methods
Software design
The EMR-BD software (http://emrbd.com/; Dhaka, Bangladesh) was designed at the National Institute of Neurosciences and Hospital (NINS&H) in November 2017. The first author (SKM) was inspired to implement an EMR system from personal experiences working with various neurosurgical departments in other countries. EMR-BD’s design was achieved in a cost-conscious manner through collaboration between local Dhaka-based computer programmers and the first author (SKM). Important features include generating patient reports, conducting medication reconciliation, and viewing hospital bed availability on the online home screen dashboard. Other components include online support for telemedicine patients, technical support for users via search-engine functionality, and a patient-provider messaging system. Additionally, the EMR-BD software collects data on tumor radiographic location, tumor pathology, presenting symptoms, follow-up care, and patient demographic data. Initial difficulties in software design included accessing the EMR-BD within areas with low-internet connectivity, facilitating uptake among colleagues at NINS&H, and maintaining technological upkeep. As of December 2020, the EMR system’s yearly maintenance fee is approximately 5000 Bangladeshi Taka (approximately US$59) and internet connectivity is provided at no additional cost from NINS&H’s hospital network. The EMR-BD software was privately financed through pediatric neurosurgeons at NINS&H. In addition, manual data entry is facilitated by a local EMR specialist for quality control and to promote system utilization among attending neurosurgeons. Last, EMR-BD’s on-site computer programmer provided technological maintenance and direct troubleshooting support.
Software implementation
The EMR-BD software was first implemented in November 2017. Key initial steps toward software implementation included identifying key stakeholders, facilitating utilization among attending neurosurgeons, and creating responsive feedback mechanisms among users. In addition, an implementation lead was identified — in this case an attending neurosurgeon — to help organize and promote implementation. Key stakeholders included various local software engineers, programmers, and attending pediatric neurosurgeons at NINS&H. To date, EMR-BD is consistently utilized by three attending neurosurgeons at NINS&H (SKM, DMA, SME), one neurosurgery division in a nearby teaching hospital (Bangladesh Medical College Hospital, Dhaka, Bangladesh), and a local non-governmental organization (NGO) for teleconferencing with patients outside of Dhaka. Several neurosurgeons outside of NINS&H have expressed interest, and they are currently exploring adoption of EMR software comparable to the EMR-BD model.
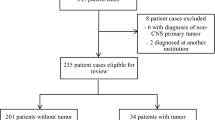
EMR database analysis
This study utilizes a database analysis to determine the advantages and shortcomings of EMR implementation in Dhaka, Bangladesh. To start, data collection systematically evaluated characteristics of each neurosurgical electronic medical record involving pediatric central nervous system tumors from August 2017 to March 2020. Table 1 demonstrates basic demographic data (i.e., presenting symptoms, date of presentation, city, etc.) collected from the EMR. Pathological diagnoses by radiographic location were also recorded where applicable.
Wherever the EMR documentation was incomplete or inconclusive, researchers described the records as best possible with existing data. Records lacking basic data were removed from the final dataset. Any discrepancies in data collections were relayed to the senior authors on the team (MCD, SKM, SME, CMB, EM) for further discussion. Collected, non-identifiable information was exported to Microsoft Excel (Albuquerque, NM, USA) for data analysis and verification. Last, this study obtained ethical review clearance at NINS&H.
Results
Two hundred forty-nine patients with a CNS tumor were admitted to NINS&H. Fifty-eight percent of patients were male, and the median age was 8 years old. The patients traveled an average of 125 km (range: 2–397 km) to NINS&H (Table 2). The most common primary presenting signs were headache/nausea/vomiting (38%; 95/249), motor weakness (22%; 54/249), visual disturbance (19%; 48/249), and seizure (8%; 20/249). The median time between index admission and surgery was 36 days, and 76% (188/249) underwent an operation with a goal of maximal safe resection. Final EOR was unable to be determined on 73% (138/188) of patients who underwent an operation due to a lack of reported post-operative imaging. In patients with complete documentation and pathologic analysis, 60% (30/50) achieved gross total resection and 40% (20/50) achieved subtotal resection. For cases not undergoing resection, a biopsy was performed on 19% (7/36) of patients, and 55% (20/36) underwent CSF-diversion only. Additional surgeries were performed on 33% (82/249) of patients. The most common additional surgeries were post-resection ventriculoperitoneal shunt insertion (71%; 58/82) and endoscopic third ventriculostomy (12%; 10/82). The median post-op length of hospital stay was 19.5 days.
Next, Table 3 describes the radiographic locations and pathologic classification of the tumors. Radiographic locations were determined for 85% (212/249) of cases; the most common radiographic locations were infratentorial (38%; 81/212), suprasellar (21%; 45/212), and supratentorial (14%; 29/212). A histopathological classification was obtained on 63% (156/249) of patients’ cytology. The most common infratentorial pathologies were medulloblastoma (47%; 22/47) and pilocytic astrocytoma (30%; 14/47). Correspondingly, the most common supratentorial pathology was ependymoma (14%; 4/29), and the most common suprasellar pathology was craniopharyngioma (87%; 34/39). Of note, 42% (34/81) of infratentorial, 13% (6/45) of suprasellar, and 14% (4/29) of supratentorial tumors lacked a final pathologic classification due to lack of available tools for pathologic analysis, insufficient tissue sample, and/or incomplete documentation. Finally, an average of six patients per day utilized the NINS&H’s EMR for neurosurgical follow-up from their home during the 2020–2021 COVID-19 pandemic. No results were obtained regarding the number of patients who passed away while admitted to NINS&H. Last, data were obtained from the outpatient department (OPD) at NINS&H and not all patients were later admitted for surgery to NINS&H.
Discussion
The design and implementation of a basic EMR platform at NINS&H offers a broad overview of the pediatric neuro-oncologic patients evaluated and services delivered within Bangladesh’s busiest neurosurgery department. EMR implementation enhanced data collection, identified areas for improvement within the department, and exposed challenges related to post-operative care and long-term follow-up, teleconferencing, outpatient follow-up appointments, and research activities. More generally, EMR implementation in LMIC neurosurgical departments can improve overall departmental efficiency, reduce financial costs, and decrease the administrative burden among medical and non-medical professionals [4, 10, 11]. On the local level, EMR implementation promotes a more accurate estimation of long-term neurosurgical outcomes of various operations performed and diseases treated [9]. Examples of such organizational benefits of EMR adoption at NINS&H include streamlined patient tracking, reduced paperwork for neurosurgical department house-staff, and pre-propagated paperwork to facilitate hospital discharge and outpatient follow-up.
Next, improved EMR documentation can help facilitate institutional data collection. Enhanced EMR documentation can provide institutions with the infrastructure necessary to contribute to important population-based cancer registries. Such efforts can improve measurements of incidence, prevalence, and treatment patterns of pediatric CNS tumors at the hospital and national level. This documentation can provide stakeholders with a comprehensive analysis of a particular geographic area’s healthcare resource distribution and needs especially in LMICs lacking robust cancer registries; in turn, EMRs can aid overall national health care delivery and facilitate stakeholder collaboration [1, 9, 12, 13]. For example, EMR implementation in Dhaka demonstrates NINS&H’s impressive reach as an average patient travels 125 km, or 77 miles, to seek neurosurgical care. For reference, 125 km is also the distance of Dhaka to the nearest city in India, Agartala; Bangladesh’s borders extend approximately 820 km (510 miles) from North to South and 600 km (370 miles) East to West. Last, while this EMR system is not currently a formal part of an institutional or national cancer registry, it demonstrates feasibility of such a model. Accordingly, in its role as a proof-of-concept, other fields could easily adapt a registry for their own medical and surgical specialties. In addition, NINS&H’s role as the country’s central hub for neuroscience health can help circumvent traditional administrative barriers and contribute to such efforts. This is an area of great interest for the authors.
Barriers to EMR acceptance in LMIC neurosurgical and medical departments are contextual, professional, and technical [14]. These barriers — including initial start-up costs, concerns about maintenance, and individual stakeholder acceptance — are well-described in the HIC-based literature [13,14,15,16,17]. At NINS&H, context-specific challenges to EMR data collection included insufficient initial data collection, inadequate data recording into the EMR, and lack of local EMR technological support. Professional challenges toward EMR utilization include competing demands on neurosurgeon’s time, and technical challenges include corrupted or locked records and incorrect or incomplete data entry. One proposed solution to this problem is to delegate EMR entry tasks to specific medical auxiliary staff to facilitate utilization [4, 9]. Additional platform-specific improvements include “flagging” records with non-existent or incorrect data entry (i.e., listed date of surgery precedes date of hospital admission). Flagged records should alert supportive medical professionals to assist the neurosurgical team in data collection, correction, or verification. Other recommendations include creating “radio buttons” or “tic boxes” to facilitate comprehensive tumor description (i.e., documentation of multifocal lesions). Reducing free-text fields expedites user interaction, meanwhile enhancing the analytic and research capability of the EMR on the backend.
In addition, it is important to document the cost of EMR implementation at NINS&H [13, 18]. While NINS&H’s yearly system maintenance fee is approximately 5000 Bangladeshi Taka or US$57, these amounts fail to account for the initial start-up fees and design costs. Additionally, EMR maintenance costs may increase with greater provider utilization at NINS&H. Potential ways to offset the cost of initial EMR purchase and system maintenance include utilizing open-source EMR systems and government-driven national EMR programs to facilitate adoption [18, 19]. Another proposed solution is to utilize global neurosurgical collaboration to finance, implement, and help manage EMR implementation in low-resource settings [20, 21]. One important example includes “twinning” neurosurgery departments in distinct countries to help facilitate an exchange of information, resources, and research [20, 22, 23]. HIC partners can provide technical support, system design, and financial contributions to streamline neurosurgical care in low-resource regions. Such HIC-based contributions help facilitate LMIC-focused partnership provision, a key component of efficacious HIC–LMIC neurosurgical partnerships [4, 18, 19, 21]. In addition, twinning at similar-country income-levels (i.e., LMIC–LMIC partnerships) can help overcome more practical barriers to EMR implementation including initial set-up, data collection, and quality assurance. NINS&H’s EMR represents an LMIC-driven model which overcame barriers to design and cost through private financing from departmental pediatric neurosurgeons. NINS&H also benefited from HIC partnership in EMR design (University of Washington) and data analysis (Vanderbilt University). Finally, while we do not explicitly document this partnership as twinning due to the lack of extensive collaboration, it can be viewed in a similar light [20, 22]. Thus, NINS&H presents one innovative model for LMIC-driven EMR design and financing.
Next, EMR implementation at NINS&H can help elucidate and inform various global pediatric neurosurgical disparities. To start, limited molecular diagnostic tools and unavailable adjuvant therapy demonstrates opportunities for improved global neurosurgical collaboration. In the case of NINS&H, applicable patients are typically referred for adjuvant therapy to local governmental facilities outside NINS&H; thus, the corresponding lack of in-house adjuvant therapy represents a fragmentation in care among pediatric neurosurgical patients. Next, analysis of the EMR reveals more overt financial and capacity-related limitations in low-resourced settings. Despite this, NINS&H’s EMR facilitated an increase in virtual telemedicine follow-up appointments among neurosurgical patients. For example, patients can utilize EMR-BD to confirm or re-schedule any upcoming follow-up appointments. NINS&H’s large geographical catchment area, the existing transportation infrastructure, and telecommunications availability all likely exacerbate these challenges to follow-up care. More intensive EMR monitoring and clinical coordination within and outside of the NINS&H Department of Pediatric Neurosurgery can help ameliorate disparities in follow-up care. This study also documents a median time between admission and surgery of 36 days and a median post-op length of hospital stay of 19.5 days. Potential reasons for this disparity include lack of post-operative care beds, lack of operating room time, and prioritizing critical care patients at NINS&H. Specifically, in the case of NINS&H’s patient population, more complex patients with hydrocephalus often require longer post-operation hospital stays. A root cause analysis of delays in care and prolonged hospitalizations is an active area of interest among the authors.
Finally, potential improvements for EMR system-integration in LMICs include systemic EMR integration among provider networks, allocating neurosurgical departmental funding for personnel trained in information technology, and adopting national open-source EMR platforms [3,4,5, 18]. Systemic EMR integration among healthcare providers can centralize care, improve data collection and coordination, and help shift the financial burden of EMR maintenance from neurosurgical departments to hospital networks [4, 24]. Hiring in-house IT personnel is one example to help troubleshoot EMR difficulties and facilitate EMR uptake among medical providers. In addition, systemic EMR integration can help mitigate challenges with internet connectivity, which may negatively impact longitudinal data monitoring.
Limitations
Further analysis is needed on the financial and economic barriers of EMR implementation in LMICs and on evidence-based strategies for EMR implementation [4]. Additionally, it is important to note that these results and analysis might not be generalizable outside of NINS&H. Research is also needed to analyze qualitative barriers to EMR design and uptake among medical professionals in LMICs. This EMR adoption study depicted various disparities in our data collection. Namely, there are gaps in mortality data, intermediate-term and long-term follow-up data, surgical details and extent of resection, pathological specimen classification, rates of treatment abandonment, and transfer of regional patients. More specifically, gaps in extent of surgical resection (EOR) are due to cases without a documented estimated EOR in the attending surgeon’s final note, cases which lacked sufficient post-operative scans, or both. In addition, reasons for lack of radiographic and/or histopathological classification include lack of available diagnostic imaging, unavailable pathologic analysis, and incomplete documentation in the EMR system. Potential opportunities to streamline documentation include developing a standardized surgical note to report estimated EOR and creating a separate tab to allow pathologists or technicians to upload results directly into the patient’s chart. This is an active area of interest among the authors. Finally, we were unable to provide objective measures of EMR adoption, update, or data collection given the current extent of NINS&H’s EMR implementation at this time. Preliminary subjective feedback from attending neurosurgeons at NINS&H is very positive and optimistic for future growth and applicability to other low-resource settings. In addition, NINS&H also created a separate outpatient clinic to help better document and collect long-term follow-up data. In turn, we hope to encourage peer institutions in low-resource settings to document shortcomings to help better define current disparities and address challenges in long-term neurosurgical follow-up care. These gaps in data collection underscore disparities in global neurosurgical care and help elucidate specific areas for future improvement and benchmarks for program evaluation at NINS&H. Analyzing EMR implementation in low-resource settings on a more systemic level remains an area of great interest among the authors.
Conclusion
NINS&H's Department of Pediatric Neurosurgery presents one feasible model for LMIC EMR design, implementation, and adoption through private financing and LMIC-based software development; this model provides pediatric neurosurgeons with a medium for data collection, follow-up care coordination, and research promotion. Collected data on pediatric CNS tumors in EMR-BD demonstrated an expected variety of tumor locations, histologic subtypes, and lack of follow-up care. Noted barriers to EMR effectiveness include limited molecular diagnostics and unavailable adjuvant therapy. Finally, NINS&H’s EMR implementation helped identify various areas for improvement in global partnerships and long-term data collection and led to the establishment of a separate outpatient clinic to improve follow-up care. We hope the analysis presented herein can serve as a template for EMR design and implementation in other LMIC neurosurgical departments.
Presented (virtually) at the 2021 International Society for Pediatric Neurosurgery Annual Meeting in Singapore, Republic of Singapore.
Data availability
Summative data has been anonymized as tables in the text.
Code availability
N/A.
Abbreviations
- NINS&H:
-
National Institute of Neurosciences and Hospital
- EMR:
-
Electronic medical record
- HIC :
-
High-income country
- LMIC:
-
Low- and middle-income country
- GTR:
-
Gross total resection
- STR:
-
Sub total resection
- SOL:
-
Space-occupying lesion
- PDU:
-
Pathological diagnosis uncertain
References
Kazley AS, Ozcan YA (2007) Organizational and environmental determinants of hospital EMR adoption: a national study. J Med Syst 31(5):375–384. https://doi.org/10.1007/s10916-007-9079-7
Lee J, Kuo YF, Goodwin JF (2013) The effect of electronic medical record adoption on outcomes in US hospitals. BMC Health Serv Res 13(1):39. https://doi.org/10.1186/1472-6963-13-39
Gyamfi A, Mensah KA, Oduro G, Donkor P, Mock CN (2017) Barriers and facilitators to electronic medical records usage in the Emergency Centre at Komfo Anokye Teaching Hospital. Kumasi-Ghana African Journal of Emergency Medicine 7(4):177–182. https://doi.org/10.1016/j.afjem.2017.05.002
Kumar M, Mostafa J (2019) Research evidence on strategies enabling integration of electronic health records in the health care systems of low-and middle-income countries: a literature review. Int J Health Plann Manage 34(2):e1016–e1025. https://doi.org/10.1002/hpm.2754
Ohuabunwa EC, Sun J, Jubanyik KJ, Wallis LA (2016) Electronic medical records in low to middle income countries: the case of Khayelitsha Hospital, South Africa. Afr J Emerg Med 6(1):38–43. https://doi.org/10.1016/j.afjem.2015.06.003
Akhlaq A, McKinstry B, Muhammad KB, Sheikh A (2016) Barriers and facilitators to health information exchange in low-and middle-income country settings: a systematic review. Health Policy Plan 31(9):1310–1325. https://doi.org/10.1093/heapol/czw056
Allorant A, Desforges G, Robin E, Honore JG, Puttkammer N (2020) Closing the gap in implementation of HIV clinical guidelines in a low resource setting using electronic medical records. BMC Health Serv Res 20(1):1–12. https://doi.org/10.1186/s12913-020-05613-8
World Health Organization (WHO) (2006) Electronic Health Records: Manual for Developing Countries
Rock JP, Prentiss T, Mo SM, Aye NS, Asmaro K, Win AT, Phyu AM, Myat T, Maung TM, Khaing AA, Naung Z (2020) Traumatic brain injury in Myanmar: preliminary results and development of an adjunct electronic medical record. World Neurosurg 140:e260–e265. https://doi.org/10.1016/j.wneu.2020.05.016
Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R (2005) Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff 24(5):1103–1117. https://doi.org/10.1377/hlthaff.24.5.1103
MacKinnon W, Wasserman M (2009) Integrated electronic medical record systems: critical success factors for implementation. 42nd Hawaii International Conference on System Sciences. IEEE
Hartzler A, McCarty CA, Rasmussen LV, Williams MS, Brilliant M, Bowton EA, Clayton EW, Faucett WA, Ferryman K, Field JR, Fullerton SM (2013) Stakeholder engagement: a key component of integrating genomic information into electronic health records. Genet Med 15(10):792–801. https://doi.org/10.1038/gim.2013.127
Reisman M (2017) EHRs: the challenge of making electronic data usable and interoperable. Pharmacy and Therapeutics 42(9):572
Kruse CS, Mitchell E, Martinez A (2016) Barriers to electronic health record adoption: a systematic literature review. J Med Syst 40(12):252. https://doi.org/10.1007/s10916-016-0628-9
Kruse CS, Kothman K, Anerobi K, Abanaka L (2016) Adoption factors of the electronic health record: a systematic review. JMIR Med Inform 4(2):e19. https://doi.org/10.2196/medinform.5525
Ben-Zion R, Pliskin N, Fink L (2014) Critical success factors for adoption of electronic health record systems: literature review and prescriptive analysis. Inform Syst Manag 31(4):296–312
Beasley S, Girard J (2016) Office-based Physician EHR Adoption and Use in Southern US States. SAIS 2016 Proceedings 26
Syzdykova A, Malta A, Zolfo M, Diro E, Oliveira JL (2017) Open-source electronic health record systems for low-resource settings: systematic review. JMIR Med Inform 5(4):e8131. https://doi.org/10.2196/medinform.8131
Aminpour F, Sadoughi F, Ahamdi M (2014) Utilization of open source electronic health record around the world: a systematic review. J Res Med Sci 19(1):57
Olivieri DJ, Baticulon RE, Labuschagne JJ, Harkness W, Warf B, Dewan MC (2020) Geospatial mapping of international neurosurgical partnerships and evaluation of extent of training and engagement. World Neurosurg 144:e898-907. https://doi.org/10.1016/j.wneu.2020.09.107
Lepard JR, Akbari SH, Haji F, Davis MC, Harkness W, Johnston JM (2020) The initial experience of InterSurgeon: an online platform to facilitate global neurosurgical partnerships. Neurosurg Focus 48(3):E15. https://doi.org/10.3171/2019.12.FOCUS19859
Uche EO, Mezue WC, Ajuzieogu O, Amah CC, Onyia E, Iloabachie I, Ryttlefors M, Tisell M (2020) Improving capacity and access to neurosurgery in sub-Saharan Africa using a twinning paradigm pioneered by the Swedish African Neurosurgical Collaboration. Acta Neurochir (Wien) 162(5):973–981. https://doi.org/10.1007/s00701-019-04207-6 (Epub 2020 Jan 4 PMID: 31902003)
Haglund MM, Kiryabwire J, Parker S, Zomorodi A, MacLeod D, Schroeder R, Muhumuza M, Merson M (2011) Surgical capacity building in Uganda through twinning, technology, and training camps. World J Surg 35(6):1175–1182. https://doi.org/10.1007/s00268-011-1080-0 (PMID: 21487850)
Boonstra A, Versluis A, Vos JF (2014) Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res 4(14):370. https://doi.org/10.1186/1472-6963-14-370
Acknowledgements
We thank the following individuals for their assistance in this project: Utpol Chowdhury MBBS FCPS, MM Ehsanul Huq MBBS, and Monish Chakraborty.
Author information
Authors and Affiliations
Contributions
DJO: data curation/investigation, formal analysis, methodology, writing — original draft, review, and editing. SKM: software design, conceptualization, formal analysis, methodology, writing — review and editing. SIM: data curation/investigation, formal analysis, methodology, writing — original draft, review, and editing. CMB: writing — review and editing. EM: writing — review and editing. DMA: conceptualization, writing — review and editing. MCD: conceptualization, data curation/investigation, formal analysis, methodology, writing — original draft, review, and editing. SME: conceptualization, methodology, writing — review, and editing.
Corresponding author
Ethics declarations
Ethics approval
Ethical Review Committee (ERC) was obtained at the National Institute of Neurosciences and Hospital (NINS&H) in Dhaka, Bangladesh.
Consent to participate
N/A.
Consent for publication
N/A.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sudipta Kumer Mukherjee, Daniel J. Olivieri, and Sarosh Irfan Madhani are co-first authors.
Michael C. Dewan and Sheikh Muhammad Ekramullah are co-senior authors.
Rights and permissions
About this article
Cite this article
Mukherjee, S.K., Olivieri, D.J., Madhani, S.I. et al. EMR adoption in Dhaka, Bangladesh: a template to index pediatric central nervous system tumor care and a review of preliminary neuro-oncologic observations. Childs Nerv Syst 38, 1497–1504 (2022). https://doi.org/10.1007/s00381-022-05450-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05450-6