Abstract
Background
Controversy exists about the pathophysiology of different hemodynamic subgroups of AS. In particular, the mechanism of the paradoxical low-flow, low-gradient (PLFLG) AS with preserved ejection fraction (EF) is unclear.
Methods
A total of 41 patients with severe, symptomatic AS were divided into the following 4 subgroups based on the echocardiographically determined hemodynamics: (1) normal-flow, high-gradient (NFHG) AS; (2) low-flow, high-gradient AS; (3) paradoxical low-flow, low-gradient (PLFLG) AS with preserved EF and (4) low-flow, low-gradient (LFLG) AS with reduced EF. As part of the comprehensive invasive examinations, the analyses of the PV loops were performed with the IntraCardiac Analyzer (CD-Leycom, The Netherlands).
Results
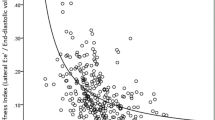
PLFLG was characterized by small left ventricular volumes as well as a decreased cardiac index, a decreased systolic contractility and a lower stroke work, than the conventional NFHG AS. Alterations in effective arterial elastance (2.36 ± 0.67 mmHg/ml in NFHG versus 3.01 ± 0.79 mmHg/ml in PLFLG, p = 0.036) and end-systolic elastance (3.72 ± 1.84 mmHg/ml in NFHG versus 5.53 ± 2.3 mmHg/ml in PLFLG, p = 0.040) indicated impaired vascular function and increased chamber stiffness.
Conclusions
The present study suggests that the hemodynamics of PLFLG AS can be explained by two mechanisms: (1) stiffness of the small left ventricle with reduced contractility, and (2) increased afterload due to the impairment of vascular function. Both mechanisms have similarities to those of heart failure with preserved EF. This type of remodeling may explain the poor prognosis of PLFLG AS.




Similar content being viewed by others
Abbreviations
- AS:
-
Aortic valve stenosis
- AVA:
-
Aortic valve area
- BNP:
-
B-type natriuretic peptide
- EF:
-
Ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- LFLG:
-
Low-flow, high-gradient
- NFHG:
-
Normal-flow, high-gradient
- PLFLG:
-
Paradoxical low-flow, low-gradient
- SVI:
-
Stroke volume index
- \(\tau\) :
-
Relaxation time constant
References
Kim WK, Hamm CW (2018) Transcatheter aortic valve implantation in Germany. Clin Res Cardiol 107(Suppl 2):81–87
Doenst T, Kirov H, Moschovas A et al (2018) Cardiac surgery 2017 reviewed. Clin Res Cardiol 107(12):1087–1102. https://doi.org/10.1007/s00392-018-1280-9 (PMID: 29777372)
Nishimura RA, Otto CM, Bonow RO, American College of Cardiology/American Heart Association Task Force on Practice Guidelines et al (2014) AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63:2438–2488
Otto CM, Prendergast B (2014) Aortic-valve stenosis—from patients at risk to severe valve obstruction. N Engl J Med 371:744–756
Clavel MA, Magne J, Pibarot P (2016) Low-gradient aortic stenosis. Eur Heart J 37:2645–2657
Jander N, Minners J, Holme I et al (2011) Outcome of patients with low-gradient “severe” aortic stenosis and preserved ejection fraction. Circulation 123:887–895 (Erratum in: Circulation. 2011;124:e336)
Chhabra L (2016) Inconsistency of hemodynamic data in low-gradient severe aortic stenosis. J Am Coll Cardiol 67:2446–2447
Clavel MA, Dumesnil JG, Capoulade R, Mathieu P, Sénéchal M, Pibarot P (2012) Outcome of patients with aortic stenosis, small valve area, and low-flow, low-gradient despite preserved left ventricular ejection fraction. J Am Coll Cardiol 60:1259–1267
Dayan V, Vignolo G, Magne J, Clavel MA, Mohty D, Pibarot P (2015) Outcome and impact of aortic valve replacement in patients with preserved LVEF and low-gradient aortic stenosis. J Am Coll Cardiol 66:2594–2603
Chin CWL, Ding ZP, Lam CSP, Ling LH (2016) Paradoxical low-gradient aortic stenosis: the HFpEF of aortic stenosis. J Am Coll Cardiol 67:2447–2448
Borlaug BA, Kass DA (2009) Invasive hemodynamic assessment in heart failure. Heart Fail Clin 5:217–228
Baumgartner H, Hung J, Bermejo J et al (2017) Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr 30:372–392
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14
Lancellotti P, Tribouilloy C, Hagendorff A, Scientific Document Committee of the European Association of Cardiovascular Imaging et al (2013) Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 14:611–644
Briand M, Dumesnil JG, Kadem L et al (2005) Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: implications for diagnosis and treatment. J Am Coll Cardiol 46:291–298
Baan J, Jong TT, Kerkhof PL et al (1981) Continuous stroke volume and cardiac output from intra-ventricular dimensions obtained with impedance catheter. Cardiovasc Res 15:328–334
Baan J, van der Velde ET, de Bruin HG et al (1984) Continuous measurement of left ventricular volume in animals and humans by conductance catheter. Circulation 70:812–823
ten Brinke EA, Klautz RJ, Verwey HF et al (2010) Single-beat estimation of the left ventricular end-systolic pressure-volume relationship in patients with heart failure. Acta Physiol (Oxf) 198:37–46
Burkhoff D, Mirsky I, Suga H (2005) Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 289:H501–H512
Tribouilloy C, Lévy F, Rusinaru D et al (2009) Outcome after aortic valve replacement for low-flow/low-gradient aortic stenosis without contractile reserve on dobutamine stress echocardiography. J Am Coll Cardiol 53:1865–1873
Schymik G, Tzamalis P, Herzberger V et al (2017) Transcatheter aortic valve implantation in patients with a reduced left ventricular ejection fraction: a single-centre experience in 2000 patients (TAVIK Registry). Clin Res Cardiol 106:1018–1025
Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P (2007) Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 115:2856–2864
Zheng Q, Djohan AH, Lim E et al (2017) Effects of aortic valve replacement on severe aortic stenosis and preserved systolic function: systematic review and network meta-analysis. Sci Rep 7:5092
Adda J, Mielot C, Giorgi R et al (2012) Low-flow, low-gradient severe aortic stenosis despite normal ejection fraction is associated with severe left ventricular dysfunction as assessed by speckle-tracking echocardiography: a multicenter study. Circ Cardiovasc Imaging 5:27–35
Herrmann S, Störk S, Niemann M et al (2011) Low-gradient aortic valve stenosis myocardial fibrosis and its influence on function and outcome. J Am Coll Cardiol 58:402–412
Kawaguchi M, Hay I, Fetics B, Kass DA (2003) Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation 107:714–720
Borlaug BA, Paulus WJ (2011) Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J 32:670–679
Gotzmann M (2018) Renin-angiotensin system blockade after TAVI: is there a link between regression of left ventricular hypertrophy and prognosis? Heart 104:628–629
Acknowledgements
This work was supported by the German Heart Foundation/German Foundation of Heart Research (F/32/12).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gotzmann, M., Hauptmann, S., Hogeweg, M. et al. Hemodynamics of paradoxical severe aortic stenosis: insight from a pressure–volume loop analysis. Clin Res Cardiol 108, 931–939 (2019). https://doi.org/10.1007/s00392-019-01423-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01423-z