Abstract
Purpose
To (i): examine whether maternal dietary inflammation assessed using the dietary inflammatory index (DII) is associated with gestational weight gain (GWG) and delivery outcomes in urban South African women from the Soweto First 1000-Day Study (S1000); and (ii): explore whether serum high-sensitivity c-reactive protein (hs-CRP) levels mediate these associations.
Methods
Energy-adjusted-DII (E-DII™) scores were calculated for 478 pregnant women using a quantitative food frequency questionnaire. GWG (kg/week) was assessed via anthropometry and hs-CRP concentrations were assessed in a sub-sample at < 14 (n = 263) and at 24–28 (n = 270) weeks gestational age. Multivariable linear and logistic regression models were used to examine associations between maternal E-DII scores, GWG, hs-CRP concentrations, and delivery outcomes.
Results
Positive vs. negative E-DII scores were associated with an increased odds of excessive weight gain (OR (95% CI): 2.23 (1.20; 4.14); P = 0.01) during pregnancy. Higher hs-CRP concentrations in the first trimester were associated with lower weight-for-length z-score (β (95% CI): −0.06 (−0.11; −0.01) per 1 mg/l hs-CRP; P = 0.02) and a reduction in odds of a large-for-gestational age delivery (OR (95% CI): 0.66 (0.47; 0.94); P = 0.02). Higher hs-CRP concentrations in the second trimester were associated with an increased odds of delivering preterm (OR (95% CI): 1.16 (1.01; 1.32); P = 0.03).
Conclusions
Consumption of an anti-inflammatory diet during pregnancy reduced the risk of excessive GWG in a rapidly urbanising setting (Soweto, South Africa), where obesity prevalence rates are high. Further research is needed to better understand how maternal diet may ameliorate the effects of maternal adiposity on inflammatory milieu and fetal programming.
Similar content being viewed by others
Introduction
In low- and middle-income countries, rapid urbanisation and the transition to increasingly westernized, energy-dense and ultra-processed diets alongside sedentary lifestyles and low levels of physical activity, have resulted in a double burden of under- and over-nutrition [1, 2]. While chronic undernutrition persists in childhood and one in four children under five are stunted in South Africa, a substantial burden of overweight and obesity has emerged; particularly affecting women of reproductive age [3].
In a longitudinal pregnancy cohort study in Soweto, Johannesburg (the Soweto First 1000-Day Study; S1000), we previously showed that maternal obesity in early pregnancy and greater adherence to more westernized and high-sugar diets were associated with higher maternal weight gain and fetal growth during pregnancy [4, 5]. In addition, greater adherence to a more traditional dietary pattern—characterized by higher intakes of whole grains, beans and legumes, traditional meats and vegetables—was associated with lower gestational weight gain (GWG), as well as with lower newborn body size (weight-to-length ratio) and adiposity (fat mass index) [6].
The Developmental Origins of Health and Disease (DOHaD) paradigm shows that fetal programming of the structure and function of body organs and tissues as a result of an adverse maternal nutrition environment has long-term consequences on growth, adiposity and metabolic health of the offspring, and may increase the risk of developing non-communicable diseases (NCDs) in later life [7, 8]. Excessive fetal growth and adiposity may be of particular concern in populations with high rates of obesity; increasing the likelihood of delivering large-for-gestational age (LGA) and/or macrosomic (≥ 4kgs) infants who are predisposed to developing obesity through the life course [8, 9]. Thus, poor maternal nutrition not only poses a risk for the health and well-being of the mother and her baby in the short and longer term, but may be responsible for propagating the cycle of obesity and NCDs through future generations [9, 10].
Proposed mechanisms for the relationships between maternal exposures, such as obesity, and adverse pregnancy outcomes include inflammatory pathways [11]. Specifically, it is possible that a pre-existing state of chronic inflammation interacts with that induced by pregnancy, thereby elevating levels beyond those compatible with a healthy pregnancy [11, 12]. Recently, it has been suggested that an anti-inflammatory diet may be useful in mitigating the effects of heightened inflammatory states on pregnancy outcomes [13]. The dietary inflammatory index (DII®) is a literature-derived tool used to assess the inflammatory potential of the diet and has been construct validated against inflammatory biomarkers—including high-sensitivity c-reactive protein (hs-CRP)—in 29 different populations (Saghafi-Asl et al., in press). Use of this tool has provided evidence supporting associations between pro-inflammatory diets during pregnancy and adverse outcomes, such as preterm birth, low birth weight and caesarean deliveries [13,14,15]. In addition, higher DII scores (indicating higher inflammatory potential of the diet) have been positively associated with neonatal adiposity; particularly in obese women [16]. Excessive GWG may further contribute to maternal inflammation [17]; however, the limited studies exploring the link between DII scores and maternal weight gain during pregnancy have shown mixed results [14, 16]. In addition, data exploring the relationships between dietary inflammatory potential, circulating inflammatory cytokines, GWG and delivery outcomes in transitioning African populations are scarce.
Given this background, this study aims to (i): examine whether maternal dietary inflammation assessed using the DII is associated with GWG and delivery outcomes in urban South African women and (ii): explore whether levels of hs-CRP during pregnancy mediate these associations.
Methods
Study setting and participants
This study was nested within a longitudinal pregnancy cohort study (Soweto First 1000-Day Study; S1000), based at the South African Medical Research Council (SAMRC)/Wits Developmental Pathways for Health Research Unit (DPHRU) at the Chris Hani Baragwanath Academic Hospital (CHBAH) in Soweto, Johannesburg, South Africa. Soweto is a large urban area of Johannesburg, where the majority of inhabitants live in low-income households. Recruitment for the study took place at the Antenatal Clinic and Fetal Medicine Unit at CHBAH; with data collection conducted between 2013 and 2016. Women were eligible for inclusion in the study if they were a black South African (self-reported ethnicity) who resided in Soweto, or the greater Soweto area, were preferably < 14 weeks, but no more than 20 weeks, pregnant with a singleton, and naturally conceived pregnancy, had no known diagnosis of epilepsy or diabetes mellitus at the time of recruitment and were 18 years or older. Data collection for S1000 took place at six timepoints during pregnancy (< 14 weeks; 14–18 weeks; 19–23 weeks; 24–28 weeks; 29–33 weeks and 34–38 weeks gestational age) and at delivery. All women provided written informed consent prior to their inclusion in the study and ethical approval was obtained from the University of the Witwatersrand’s Research Ethics Committee (Medical) (ethical clearance number: M120524). In all, 559 women were recruited into this sub-study and had dietary intake assessed at 14–18 weeks.
Data collection
Demographic, health and socio-economic variables
Maternal demographic, health and socio-economic variables were collected using interviewer-administered questionnaires at the baseline visit (< 14-weeks) as described in detail elsewhere [4,5,6]. Maternal education was defined according to the highest level of education completed (primary, secondary or tertiary). Haemoglobin levels (g/dl) were assessed using a HemoCue at baseline and anaemia was classified as a haemoglobin level of < 11.0 g/dL [18]. In cases, where haemoglobin levels were not assessed during the first visit, the haemoglobin level at visit 2 (14–18-weeks) was used to classify anaemia status.
Maternal anthropometry
A wall-mounted Stadiometer (Holtain, UK) was used to measure height to the nearest 1 mm during the baseline visit. Weight was measured to the nearest 0.1 kg at each pregnancy visit using a digital scale. Weight at baseline (< 14 weeks) was used as a proxy for pre-pregnancy weight and, together with height, was used to calculate BMI (weight (kg)/height (m)2). As there were no underweight women in this sample, BMI was classified according to the following categories defined by the World Health Organization (WHO) and used extensively in the literature: normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) or obese (≥ 30.0 kg/m2). GWG (kg/week) was calculated as: [(weight at final pregnancy visit − weight at baseline)/duration of follow-up]. GWG was classified according to the Institute of Medicine (IoM) BMI-specific weight gain ranges [19].
Dietary intake and the energy-adjusted DII (E-DII.™)
Habitual dietary intake was assessed at the second pregnancy visit (14–18 weeks) using an interviewer-administered quantitative food-frequency questionnaire (QFFQ) described in detail elsewhere [4, 20, 21]. In brief, retrospective data were collected on the frequency and quantity of food and beverage intake during the previous week. QFFQ data were captured using REDCap electronic data capture tools hosted at The University of the Witwatersrand [22]. Daily energy and nutrient intakes were then calculated from conversion of single food item intakes by the SAMRC using the South African Food Composition Tables.
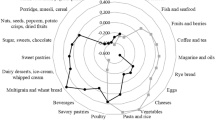
The inflammatory potential of the diet was calculated based on the DII which converts nutrient intakes from the FFQ into an equivalent DII score for each participant. The development of the DII has been described in detail elsewhere [23]. In brief, the mean intakes of each food item were translated into z-scores using a global comparative database consisting of data from 11 countries. These scores were then converted to proportions and centred on zero by doubling and subtracting 1. These cantered proportions were then multiplied by their respective coefficients (overall food parameter-specific inflammatory effect scores) to calculate DII scores per food parameter which were summed to obtain the overall DII score. A positive DII score corresponds to a pro-inflammatory dietary habit and a negative DII score indicates an anti-inflammatory dietary habit. The following 21 food parameters were available to calculate the DII scores in the present study: carbohydrates, fat, protein, cholesterol, saturated fatty acids, monounsaturated fatty acids, polyunsaturated fatty acids, vitamin B12, vitamin B6, vitamin A, vitamin C, vitamin D, vitamin E, riboflavin, thiamine, iron, magnesium, folic acid, zinc, niacin, fibre. Energy-adjusted DII (E-DII™) scores were calculated using the density approach by calculating DII per 1000 kcal consumption that employed the same procedure for disease scoring based on an energy-adjusted global comparison database [24, 25].
Biochemical measurements
Fasting blood samples were collected by trained nurses at the baseline visit (< 14-weeks) and at visit 4 (24–28-weeks). hs-CRP concentrations were measured in serum using a particle-enhanced immunoturbidometric assay (RX Daytona Plus RX series analyser, Randox Laboratories, Crumlin, United Kingdom). At both timepoints, values of hs-CRP > 10 mg/l were excluded from the sub-sample for analyses, as this may be a result of acute inflammation.
Delivery outcomes
Gestational age at delivery (weeks) was calculated as: [duration of pregnancy follow-up (date of delivery − date of baseline ultrasound dating scan) + gestational age at baseline (crown-to-rump length measured by ultrasound; days)]. Birth weight and length were measured by trained research nurses using a calibrated SECA Baby Scale 376 (SECA) and a Harpenden Infantometer (Holtain, London, UK), respectively, within 24 h of delivery for 82% of newborns. Where assessment within this window was not possible—for example due to the infant being admitted to the hospital for observation—measurements were taken within 48 h. Head circumference was measured using a metal head circumference tape measure (CMS ref.3105) (Chasmors Ltd, London, UK). The International Newborn Size at Birth Standards Application tool was used to calculate birth weight centiles, as well as weight-to-length z-scores, according to newborn sex and gestational age at delivery (total days) [26]. The following criteria were used to classify newborns according to their birth weight: small-for-gestational age (SGA), < 10th centile; appropriate-for-gestational age (AGA), 10th–90th centile; LGA, > 90th centile. Low birth weight was defined as a birth weight < 2.5 kg and macrosomia was defined as a birth weight ≥ 4.0 kg.
Statistical analysis
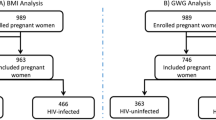
Data were analysed for 478 mother–newborn pairs with complete maternal and neonatal anthropometric data using StataSE version 16.0 (StataCorp, College Station, TX, USA). The flow of participants through the study to reach the final sample size is depicted in Supplementary Fig. 1 (online resource). Continuous variables were described as median (interquartile range; IQR) and categorical variables were described as percentages (%). Maternal dietary parameters used for calculating the E-DII scores, as well as maternal characteristics and birth outcomes, were summarised according to negative (anti-inflammatory) vs. positive (pro-inflammatory) E-DII scores and compared using Kruskal–Wallis (continuous variables) and Chi2 (categorical variables) tests. Multivariable logistic regression models (categorical outcomes) and linear regression models (continuous outcomes) were used to test the associations between maternal E-DII scores (positive vs. negative; reference category) and IoM GWG categories (inadequate and excessive GWG vs. adequate GWG; reference category), as well as delivery outcomes. Delivery outcomes included in the models (i.e., preterm birth, SGA, LGA and weight-for-length z-score) were those hypothesised to be associated with maternal dietary inflammation from the literature. In the case of GWG, models were run as follows: Model 1 (M1): DII category; Model 2 (M2): M1 with hs-CRP concentration (mg/l) at visit 1 or visit 4 (separate models per timepoint); Model 3 (M3): M2 adjusted for maternal BMI at recruitment, HIV status and parity. For birth outcomes, the following three models were run: Model 1 (M1): DII category adjusted for newborn sex; Model 2 (M2): M1 with hs-CRP concentration (mg/l) at visit 1 and visit 4 (separate models per timepoint); Model 3 (M3): M2 adjusted for maternal BMI at recruitment, GWG (kg/week), HIV status, parity and smoking status. Covariates included in the analyses were those conclusively associated with maternal dietary patterns and GWG and/or infant outcomes in previous research [4, 6]. R2 values were used to assess the degree of variation explained by final models for all significant associations.
Results
Dietary parameters and E-DII scores
Maternal E-DII scores and the dietary parameters used in their calculation are presented in Table 1. Women in the pro-inflammatory diet group (i.e., those with positive E-DII scores) reported higher intakes of carbohydrate, protein, fat, cholesterol and vitamin A and lower intakes of fibre, folate and vitamin E than those in the anti-inflammatory group (i.e., those with negative E-DII scores).
Participant characteristics
Maternal characteristics and delivery outcomes for mother–newborn pairs are presented in Table 2. Approximately two thirds of women were affected by overweight or obesity at recruitment and 46% gained excessive weight during pregnancy. Women in the pro-inflammatory diet group were significantly younger (P < 0.001) and were more likely to be single (P = 0.001) than those in the anti-inflammatory diet group. They also were more likely to gain excessive weight during pregnancy (P = 0.04). Median hs-CRP concentrations increased between visit 1 and visit 4; however, there were no significant differences in hs-CRP levels between the anti-inflammatory and the pro-inflammatory diet groups at either timepoint. There were no differences in delivery outcomes between the anti-inflammatory and pro-inflammatory diet groups.
Associations between dietary inflammation, hs-CRP and GWG
The associations between E-DII scores, hs-CRP concentrations and GWG are presented in Table 3. A pro-inflammatory diet (i.e., a positive E-DII score) was associated with an increased odds of excessive weight gain, independent of maternal BMI at recruitment, HIV-status and parity (M2, OR (95% CI): 2.23 (1.20; 4.14); P = 0.01). Similarly, in sub-analyses, positive E-DII scores were associated with an increased odds of excessive weight gain, independent of hs-CRP concentrations at visit 4 and other covariates (M3, OR (95% CI): 2.53 (1.12; 5.72) P = 0.03). The final models explained < 5% of the variation in the odds of excessive weight gain (data not shown).
Associations between dietary inflammation, hs-CRP and delivery outcomes
There were no associations found between E-DII scores and any delivery outcomes (preterm birth, SGA, LGA or weight-for-length z-score) in unadjusted or adjusted models (Tables 4 and 5). However, in the sub-sample of participants with hs-CRP values, hs-CRP concentration at visit 4 was associated with an increase in odds of preterm birth in fully adjusted models (M3, OR (95% CI): 1.16 (1.01; 1.32); P = 0.03) and hs-CRP concentration at visit 1 was associated with a reduced odds of a LGA delivery (M3, OR (95% CI): 0.66 (0.47; 0.94); P = 0.02) (Table 4). These final models explained < 5% of the variation in the odds of preterm birth, but 21.6% of the variation in the odds of a LGA delivery. Similarly, hs-CRP concentration at visit 1 was negatively associated with weight-for-length z-score, after adjustment for all covariates (M3, β (95% CI): −0.06 (−0.11; −0.01) per 1 mg/l hs-CRP; P = 0.02) (Table 5). This final model explained 8.9% of the variation in weight-for-length z-score.
Discussion
This study examined the associations between maternal dietary inflammatory potential and GWG and delivery outcomes in urban South African women, as well as whether these associations were mediated by circulating hs-CRP levels during the first and second trimesters of pregnancy. We found that a pro-inflammatory diet was associated with a higher odds of excessive weight gain during pregnancy, independent of hs-CRP concentrations. While there were no associations between E-DII scores and delivery outcomes, higher hs-CRP concentrations in the first trimester were associated with smaller birth size (lower weight-for-length z-score), as well as with a reduction in the odds of a LGA delivery. In addition, higher hs-CRP concentrations in the second trimester were associated with an increase in the odds of delivering preterm.
Our data support and build on previous findings from this cohort; particularly showing an association between greater adherence to a maternal “traditional” dietary pattern, high in whole grains, traditional meats, beans, legumes and vegetables, and a reduction in the odds of excessive GWG [4]. In this, and other, cohort studies positive associations between more westernized, highly processed and high-sugar dietary patterns and pregnancy weight gain have also been shown [4, 27,28,29]. As seen here, the inflammatory potential of an energy dense diet high in refined carbohydrates, protein and fat (particularly saturated fat) and low in fibre, may be contributing to the likelihood of excessive weight gain during pregnancy. Previous studies in high-income populations have shown mixed results for the associations between DII scores and GWG [14, 16]. Discrepancies in relationships, or null findings, may be partly explained by the use of unadjusted DII scores in these studies; with the E-DII scores used here showing improved prediction due to the use of energy-adjusted nutrient scores [25]. In settings, such as South Africa, where two-thirds of women experience overweight or obesity when they conceive [3], promoting healthy weight gain during pregnancy is important for optimising fetal growth and development, as well as reducing the risk of obesity as infants age [8, 30, 31].
In non-pregnant adult populations from high income countries, previous studies have demonstrated inverse associations between the consumption of whole grains, fruit, dietary fibre, and polyunsaturated fatty acids and biomarkers of inflammation, such as hs-CRP and interleukin-6, in non-pregnant adult populations [32,33,34,35]. Similarly, positive associations between dietary patterns high in processed meat and saturated fat and inflammatory markers have been documented [33, 35]. While our study showed the association between E-DII scores and GWG to be independent of hs-CRP concentrations, Sen et al., found positive associations between DII scores and CRP concentrations in pregnant women from Project Viva [14]. On the other hand, Moore et al., found that higher DII scores were associated with elevated interleukin-6, but not CRP, concentrations during pregnancy [16]. Since the production of inflammatory biomarkers is a complex cascade, and the production of one may depend on that of another, it has been suggested that discrepancies across studies may, at least in part, be related to the timing of cytokine assessment in the study population [16].
As with our findings for dietary inflammatory potential and weight gain, the associations between hs-CRP concentrations and birth outcomes demonstrated here are supported by some, but not all, previous studies. For example, in two US cohorts and one Chinese cohort study, dietary inflammatory potential and elevated CRP have been associated with preterm birth for female fetuses, as well as with smaller birth size and increased risk of low birth weight [13,14,15]. In contrast, associations between DII scores, elevated interleukin-6 concentration and higher birth size and adiposity have been shown in a US-based cohort [16]. Similarly, while our study showed no association between E-DII scores and birth outcomes, we have previously demonstrated an inverse association between adherence to the “traditional” dietary pattern and birth size and neonatal adiposity [6]. In addition, we have provided evidence of a pathway for greater neonatal adiposity in this cohort via an effect of higher GWG on fetal growth—particularly at the abdominal circumference [36].
Potential differences between the effects of diet, adiposity and inflammation during pregnancy on birth outcomes may be due to the complexity of the relationships between these factors and the overall health and nutritional status of the population prior to, and during, pregnancy, as well as the methodology used to assess dietary inflammation and inflammatory biomarkers. For example, the Chinese cohort was limited to women within a healthy BMI range who did not demonstrate inflammatory symptoms pre-pregnancy; which may explain the increased likelihood of low birth weight deliveries for women with pro-inflammatory diets and higher circulating CRP concentrations [15]. Furthermore, although overweight and obesity prevalence rates were high in the remaining studies, as in the study by Sen et al., women in our study were more likely to have an anti-inflammatory diet compared to those in the study by Moore et al., where the mean DII score was positive [14, 16]. In addition, while we and Sen et al. showed associations between elevated CRP concentrations and lower birth size, Moore et al. found that dietary inflammatory potential and elevated interleukin-6 were positively associated with neonatal adiposity; suggesting that the pathways may differ for individual markers of inflammation across pregnancy.
Taken together, findings from this and other studies, suggest that ensuring a healthy weight prior to pregnancy, as well as consuming an anti-inflammatory diet throughout pregnancy, may contribute to a reduced risk of excessive weight gain and lower levels of systemic inflammation during pregnancy. This, in turn, may reduce the risk of adverse delivery outcomes while contributing to healthy growth and development of the fetus; thus, optimising metabolic health trajectories and reducing the risk of obesity and NCDs across the life course. However, this also shows that the pathways of inflammation during pregnancy are complex and interrelated—making a holistic approach to preconception and pregnancy health which considers all risk factors important in providing the best support for mom and baby. For example, while our findings were independent of maternal BMI at study recruitment, it is likely that obesity-induced inflammation—as well as that potentially induced by other co-morbidities (e.g., HIV/treatment, anaemia and gestational diabetes mellitus)—would contribute to the overall inflammatory state during pregnancy and thus, to outcomes in the short and longer term.
This, and previous, findings from S1000 emphasise the need to prioritise preconception health of adolescent girls and young women to establish healthy dietary practices, body size and metabolic profiles prior to pregnancy [4,5,6, 36]. However, in low-income settings such as Soweto, poverty and limited financial resources restrict access to diverse, high quality diets [37]. It has been proposed that the arrival of the COVID-19 pandemic and the restrictions in movement and economic activity to curb the spread of the virus, may have exacerbated inequalities in access to healthy diet and lifestyle behaviours [38]. However, rapid responses to the pandemic across economic, political, food and built environment sectors in low- and middle-income countries also provide promising insight into the potential for whole-of-society approaches to interventions which promote sustainable behaviour change in the future [38].
Strengths and limitations
Our study benefited from use of the DII—a globally recognised and comparable tool which is based on robust scientific literature, rather than population specific intakes or recommendations, and is linked to measurable health outcomes [23]. Rather than exploring the effects of individual nutrients, this method allows for assessment of the inflammatory potential of the overall diet; with use of E-DII scores ensuring any effects of dietary inflammation are independent of the total energy consumed [23]. However, the lack of representation of African populations in the global dietary database used for calibration of the DII may reduce the tools ability to accurately depict the inflammatory profile of the South African diet [23, 39]. Extension of the database to include more under-represented populations should, therefore, continue to better describe dietary diversity between populations [39]. Typically, FFQs focus on a period of 3 months or longer during which the respondent is asked to provide an estimate of frequency of exposure. The FFQ used in this study included only a 7-day recall period and this may have limited the ability to reflect habitual intake over a longer period of time. As we noted earlier in developing the 7-day diet recall [40], a reference period of one week mixes both episodic and habitual memory that should improve accuracy of exposure. Thus, our approach, while perhaps not capturing habitual intake optimally, minimised the recall bias introduced by relying on a longer recall period. In addition, only 21 of the 45 potential food parameters used to calculate the DII score were available for this analysis. While this may have restricted our ability to obtain a full picture of the inflammatory potential of the diet, many previous studies have shown the DII/E-DII as a robust tool to test the association between the DII and inflammation using fewer parameters [41,42,43]. Further limitations of our study were the small sample size with dietary data available from the S1000 study and that only one inflammatory biomarker was assessed in a smaller sub-sample of participants. This limited our ability to determine whether the association between dietary inflammation and GWG was mediated via an effect on inflammatory cytokines. The mechanisms whereby a pro-inflammatory diet may influence maternal adiposity and fetal metabolic programming are complex and currently not well understood—particularly in rapidly urbanising low- and middle-income populations, where data are scarce [44]. Further exploration into the relationship between a pro-inflammatory diet, inflammatory milieu during pregnancy (including other co-morbidities, such as gestational diabetes mellitus) and outcomes, is, therefore, needed.
Conclusions
This study showed that an anti-inflammatory diet during pregnancy was associated with a reduced risk of excessive weight gain in a rapidly urbanising setting (Soweto) in South Africa where obesity prevalence rates are high. However, findings also demonstrate the complexity of the associations between maternal diet, adiposity and inflammation during pregnancy, as well as the implications for fetal growth and development in the short and longer term. Further exploration into the drivers of maternal inflammation during pregnancy using diverse inflammatory markers is, therefore, needed to better understand how maternal diet may ameliorate the effects of maternal adiposity on inflammatory milieu and fetal programming.
References
Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395:65–74. https://doi.org/10.1016/S0140-6736(19)32497-3
Popkin BM, Adair LS, Ng SW (2012) Now and then: the global nutrition transition: the pandemic of obesity in developing countries. Nutr Rev 70:3–21. https://doi.org/10.1111/j.1753-4887.2011.00456.x
Statistics South Africa (2017) South Africa Demographic and Health Survey 2016. Key indicators report. Statistics South Africa, Pretoria
Wrottesley SV, Pisa PT, Norris SA (2017) The influence of maternal dietary patterns on body mass index and gestational weight gain in urban black South African women. Nutrients 9:732. https://doi.org/10.3390/nu9070732
Wrottesley SV, Prioreschi A, Kehoe SH et al (2020) A maternal “mixed, high sugar” dietary pattern is associated with fetal growth. Matern Child Nutr 16:e12912. https://doi.org/10.1111/mcn.12912
Wrottesley SV, Ong KK, Pisa PT, Norris SA (2018) Maternal traditional dietary pattern and antiretroviral treatment exposure are associated with neonatal size and adiposity in urban, black South Africans. Br J Nutr 120:557–566. https://doi.org/10.1017/S0007114518001708
Mandy M, Nyirenda M (2018) Developmental origins of health and disease: the relevance to developing nations. Int Health 10:66–70. https://doi.org/10.1093/inthealth/ihy006
Poston L, Caleyachetty R, Cnattingius S et al (2016) Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol 4:1025–1036. https://doi.org/10.1016/S2213-8587(16)30217-0
Dabelea D, Crume T (2011) Maternal environment and the transgenerational cycle of obesity and diabetes. Diabetes 60:1849–1855. https://doi.org/10.2337/db11-0400
Ladfors L, Shaat N, Wiberg N et al (2017) Fetal overgrowth in women with type 1 and type 2 diabetes mellitus. PLoS ONE 12:e0187917. https://doi.org/10.1371/journal.pone.0187917
Denison FC, Roberts KA, Barr SM, Norman JE (2010) Obesity, pregnancy, inflammation, and vascular function. Reproduction 140:373–385. https://doi.org/10.1530/REP-10-0074
Segovia SA, Vickers MH, Reynolds CM (2017) The impact of maternal obesity on inflammatory processes and consequences for later offspring health outcomes. J Dev Orig Health Dis 8:529–540. https://doi.org/10.1017/S2040174417000204
McCullough LE, Miller EE, Calderwood LE et al (2017) Maternal inflammatory diet and adverse pregnancy outcomes: circulating cytokines and genomic imprinting as potential regulators? Epigenetics 12:688–697. https://doi.org/10.1080/15592294.2017.1347241
Sen S, Rifas-Shiman SL, Shivappa N et al (2016) Dietary inflammatory potential during pregnancy is associated with lower fetal growth and breastfeeding failure: results from Project Viva. J Nutr 146:728–736. https://doi.org/10.3945/jn.115.225581
Yang Y, Kan H, Yu X et al (2020) Relationship between dietary inflammatory index, hs-CRP level in the second trimester and neonatal birth weight: a cohort study. J Clin Biochem Nutr 66:163–167. https://doi.org/10.3164/jcbn.19-100
Moore BF, Sauder KA, Starling AP et al (2018) Pro-inflammatory diets during pregnancy and neonatal adiposity in the Healthy Start Study. J Pediatr 195:121-127.e2. https://doi.org/10.1016/j.jpeds.2017.10.030
Hrolfsdottir L, Schalkwijk CG, Birgisdottir BE et al (2016) Maternal diet, gestational weight gain, and inflammatory markers during pregnancy. Obesity (Silver Spring) 24:2133–2139. https://doi.org/10.1002/oby.21617
World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization, Geneva, Switzerland
IOM (Institute of Medicine) and NRC (National Research Council) (2009) Weight gain during pregnancy: reexamining the guidelines. The National Academies Press, Washington, DC
Wrottesley SV, Micklesfield LK, Hamill MM et al (2014) Dietary intake and body composition in HIV-positive and -negative South African women. Public Health Nutr 17:1603–1613. https://doi.org/10.1017/S1368980013001808
Zingoni C, Norris SA, Griffiths PL, Cameron N (2009) Studying a population undergoing nutrition transition: a practical case study of dietary assessment in urban South African adolescents. Ecol Food Nutr 48:178–198. https://doi.org/10.1080/03670240902794713
Harris P, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Shivappa N, Steck SE, Hurley TG et al (2014) Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr 17:1689–1696. https://doi.org/10.1017/S1368980013002115
Harmon BE, Wirth MD, Boushey CJ et al (2017) The dietary inflammatory index is associated with colorectal cancer risk in the Multiethnic Cohort. J Nutr 147:430–438. https://doi.org/10.3945/jn.116.242529
Hébert JR, Shivappa N, Wirth MD et al (2019) Perspective: the dietary inflammatory index (DII)—lessons learned, improvements made, and future directions. Adv Nutr 10:185–195. https://doi.org/10.1093/advances/nmy071
INTERGROWTH-21st (2017) The international newborn size at birth standards application. Oxford University, Oxford
Tielemans MJ, Erler NS, Leermakers ETM et al (2015) A priori and a posteriori dietary patterns during pregnancy and gestational weight gain: the Generation R study. Nutrients 7:9383–9399. https://doi.org/10.3390/nu7115476
Guilloty NI, Soto R, Anzalota L et al (2015) Diet, pre-pregnancy BMI, and gestational weight gain in Puerto Rican women. Matern Child Health J 19:2453–2461. https://doi.org/10.1007/s10995-015-1764-4
Uusitalo U, Arkkola T, Ovaskainen M-L et al (2009) Unhealthy dietary patterns are associated with weight gain during pregnancy among Finnish women. Public Health Nutr 12:2392–2399. https://doi.org/10.1017/S136898000900528X
Voerman E, Santos S, Patro Golab B et al (2019) Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. https://doi.org/10.1371/journal.pmed.1002744
Josey MJ, McCullough LE, Hoyo C, Williams-DeVane C (2019) Overall gestational weight gain mediates the relationship between maternal and child obesity. BMC Public Health 19:1062. https://doi.org/10.1186/s12889-019-7349-1
Shin D, Hur J, Cho E-H et al (2017) Pre-pregnancy body mass index is associated with dietary inflammatory index and c-reactive protein concentrations during pregnancy. Nutrients. https://doi.org/10.3390/nu9040351
Nettleton JA, Steffen LM, Mayer-Davis EJ et al (2006) Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 83:1369–1379. https://doi.org/10.1093/ajcn/83.6.1369
North CJ, Venter CS, Jerling JC (2009) The effects of dietary fibre on C-reactive protein, an inflammation marker predicting cardiovascular disease. Eur J Clin Nutr 63:921–933. https://doi.org/10.1038/ejcn.2009.8
Clarke R, Shipley M, Armitage J et al (2009) Plasma phospholipid fatty acids and CHD in older men: Whitehall study of London civil servants. Br J Nutr 102:279–284. https://doi.org/10.1017/S0007114508143562
Wrottesley SV, Prioreschi A, Norris SA (2020) The association between fetal growth and neonatal adiposity in urban South African infants. Pediatr Obes 16:e12737. https://doi.org/10.1111/ijpo.12737
Farrell P, Thow AM, Abimbola S et al (2018) How food insecurity could lead to obesity in LMICs when not enough is too much: a realist review of how food insecurity could lead to obesity in low- and middle-income countries. Health Promot Int 33:812–826. https://doi.org/10.1093/heapro/dax026
Oni T, Micklesfield LK, Wadende P et al (2020) (2020) Implications of COVID-19 control measures for diet and physical activity, and lessons for addressing other pandemics facing rapidly urbanising countries. Glob Health Action. https://doi.org/10.1080/16549716.2020.1810415
Mtintsilana A, Micklesfield LK, Chorell E et al (2019) Adiposity mediates the association between the dietary inflammatory index and markers of type 2 diabetes risk in middle-aged black South African women. Nutrients. https://doi.org/10.3390/nu11061246
Hebert JR, Ockene IS, Hurley TG et al (1997) Development and testing of a seven-day dietary recall. Dietary Assessment Working Group of the Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). J Clin Epidemiol 50:925–937. https://doi.org/10.1016/s0895-4356(97)00098-x
Ruiz-Canela M, Zazpe I, Shivappa N et al (2015) Dietary inflammatory index and anthropometric measures of obesity in a population sample at high cardiovascular risk from the PREDIMED (PREvención con DIeta MEDiterránea) trial. Br J Nutr 113:984–995. https://doi.org/10.1017/S0007114514004401
Vahid F, Bourbour F, Gholamalizadeh M et al (2020) A pro-inflammatory diet increases the likelihood of obesity and overweight in adolescent boys: a case–control study. Diabetol Metab Syndr 12:29. https://doi.org/10.1186/s13098-020-00536-0
Denova-Gutiérrez E, Muñoz-Aguirre P, Shivappa N et al (2018) Dietary inflammatory index and type 2 diabetes mellitus in adults: the Diabetes Mellitus Survey of Mexico City. Nutrients 10:E385. https://doi.org/10.3390/nu10040385
Heerwagen MJR, Miller MR, Barbour LA, Friedman JE (2010) Maternal obesity and fetal metabolic programming: a fertile epigenetic soil. Am J Physiol Regul Integr Comp Physiol 299:R711-722. https://doi.org/10.1152/ajpregu.00310.2010
Funding
This research was funded by the South African Medical Research Council (SAMRC). SVW, AP and SAN was supported by the DSI–NRF Centre of Excellence in Human Development at the University of the Witwatersrand, Johannesburg, South Africa. SVW was also supported by the University Research Office and School of Clinical Medicine at the University of the Witwatersrand, Johannesburg, South Africa.
Author information
Authors and Affiliations
Contributions
SVW, AP and SAN designed the research; SVW, NS and JRH analysed data; SVW wrote the paper and had primary responsibility for final content; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclosure
Dr. James R. Hébert owns controlling interest in Connecting Health Innovations LLC (CHI), a company that has licensed the right to his invention of the dietary inflammatory index (DII®) from the University of South Carolina to develop computer and smart phone applications for patient counselling and dietary intervention in clinical settings. Dr. Nitin Shivappa is an employee of CHI. The subject matter of this paper will not have any direct bearing on that work, nor has that activity exerted any influence on this project.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wrottesley, S.V., Shivappa, N., Prioreschi, A. et al. Anti-inflammatory diets reduce the risk of excessive gestational weight gain in urban South Africans from the Soweto First 1000-Day Study (S1000). Eur J Nutr 61, 3929–3941 (2022). https://doi.org/10.1007/s00394-022-02931-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02931-x