Abstract
Background
Tachycardia-induced cardiomyopathy (TCM) has been known for decades as a reversible form of non-ischemic cardiomyopathy. However, its mechanism and characteristics remain poorly understood.
Objectives
This retrospective study investigated endomyocardial biopsy (EMB) samples from consecutive patients with TCM and compared them with samples from patients with dilated cardiomyopathy (DCM) and inflammatory cardiomyopathy (InCM).
Materials and methods
A total of 684 patients (18 TCM, 170 DCM, 496 InCM) with recent-onset heart failure and reduced ejection fraction unrelated to valvular or ischemic heart disease were analyzed.
Results
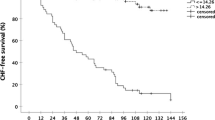
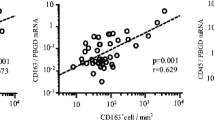
In the TCM group, 81% were male, the mean age was 60 ± 13 years, and 94% had heart failure symptoms ≥2 New York Heart Association (NYHA) class. At baseline (BL), 78% had atrial fibrillation/flutter and 12% other forms of tachycardia or frequent extrasystole. The ventricular rate was higher compared to DCM and InCM patients (122 ± 25 versus 78 ± 21; p < 0.001). Mean ejection fraction at BL was lower compared to DCM and InCM (27 ± 12% versus 39.0 ± 14.6%; p = 0.001), but improved to a significantly greater extent during follow-up (FU) (20% versus 6%; p < 0.001). At FU, heart rate and presence of sinus rhythm were similar in all groups; 69% of TCM patients underwent cardioversion or ablation. Compared with DCM patients, TCM patients had stronger myocardial expression of major histocompatibility complex (MHC) class II and an equal amount of infiltration with T‑cells/macrophages. Compared with InCM patients, the presence of T‑cells/macrophages was significantly lower in TCM. The marker of apoptosis (caspase 3) was comparably elevated in TCM/InCM patients.
Conclusion
Tachycardia-induced cardiomyopathy is characterized by immunohistological changes comparable to DCM except for caspase 3 levels, which were similar to those in InCM.
Zusammenfassung
Hintergrund
Die tachykardieinduzierte Kardiomyopathie (TCM) ist seit Jahrzehnten als reversible Form einer nichtischämischen Kardiomyopathie bekannt. Die zugrunde liegenden Mechanismen sind jedoch unzureichend verstanden.
Fragestellung
In dieser retrospektiven Studie wurden Endomyokardbiopsien (EMB) von konsekutiven Patienten mit TCM analysiert und mit EMB von Patienten mit dilatativer (DCM) und inflammatorischer Kardiomyopathie (InCM) verglichen.
Material und Methoden
Untersucht wurden 684 Patienten (18 TCM, 170 DCM, 496 InCM) mit kürzlich aufgetretener Herzinsuffizienz und reduzierter linksventrikulärer Pumpfunktion (LVEF), welche nicht durch Klappenvitien oder myokardiale Ischämie hervorgerufen wurde.
Ergebnisse
In der TCM-Gruppe waren 81 % männlich, das mittlere Alter lag bei 60 ± 13 Jahren, 94 % hatten Herzinsuffizienzsymptome der New-York-Heart-Association(NYHA)-Klasse ≥2. Zur Baseline (BL) hatten 78 % Vorhofflimmern/-flattern und 12 % andere Formen der Tachykardie oder häufige Extrasystolen; die Herzfrequenz war höher im Vergleich zu Patienten mit DCM und InCM (122 ± 25 vs. 78 ± 21; p < 0,001). Die mittlere LVEF zur BL war geringer im Vergleich zu DCM und InCM (27 ± 12 % vs. 39,0 ± 14,6 %; p = 0,001), besserte sich aber signifikant stärker während des Follow-ups (FU; 20 % vs. 6 %; p < 0,001). Zum FU waren die Herzfrequenz und die Häufigkeit eines Sinusrhythmus in allen Gruppen vergleichbar. 69 % der Patienten mit TCM unterzogen sich einer Kardioversion oder Ablationsbehandlung. Verglichen mit DCM-Patienten hatten TCM-Patienten eine ausgeprägtere myokardiale Expression des Haupthistokompatibilitätskomplexes (MHC) Klasse II und ein vergleichbares Ausmaß an Infiltration mit T‑Zellen/Makrophagen. Verglichen mit InCM-Patienten war die Infiltration mit T‑Zellen/Makrophagen bei TCM signifikant geringer. Der Apoptosemarker Caspase 3 war bei Patienten mit TCM bzw. InCM vergleichbar erhöht.
Schlussfolgerung
Die TCM ist charakterisiert durch immunhistologische Veränderungen, die mit denen einer DCM vergleichbar sind, mit Ausnahme des Apoptoseparameters Caspase 3, der mit der InCM vergleichbar ist.




Similar content being viewed by others
References
Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM (2013) European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on etiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 34:2636–2648
Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, Levine GN, Narula J, Starling RC, Towbin J, Virmani R (2007) The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Eur Heart J 28:3076–3093
Deshmukh PM, Krishnamani R, Romanyshyn M, Johnson AK, Noti JD (2004) Association of angiotensin-converting enzyme gene polymorphism with tachycardia cardiomyopathy. Int J Mol Med 13(3):455–458
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K (2008of) ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 29:2388–2442
Ellis ER, Josephson ME (2013) Heart failure and tachycardia-induced cardiomyopathy. Curr Heart Fail Rep 10(4):296–306
Gopinathannair R, Etheridge SP, Marchlinski FE, Spinale FG, Lakkireddy D, Olshansky B (2015) Arrhythmia-induced cardiomyopathies: mechanisms, recognition, and management. J Am Coll Cardiol 66(15):1714–1728
Gossage AM, Braxton Hicks JA (1913) On auricular fibrillation. Q J Med 6(4):435–440
Kajstura J, Zhang X, Liu Y, Szoke E, Cheng W, Olivetti G, Hintze H, Anversa P (1995) The cellular basis of pacing-induced dilated cardiomyopathy: myocyte cell loss and myocyte cellular reactive hypertrophy. Circulation 92:2306–2317
Kim DY, Kim SH, Ryu KH (2019) Tachycardia induced cardiomyopathy. Korean Circ J 49(9):808–817
Leone O, Veinot JP, Angelini A, Baandrup UT, Basso C, Berry G, Bruneval P, Burke M, Butany J, Calabrese F, d’Amati G, Edwards WD, Fallon JT, Fishbein MC, Gallagher PJ, Halushka MK, McManus B, Pucci A, Rodriguez ER, Saffitz JE, Sheppard MN, Steenbergen C, Stone JR, Tan C, Thiene G, van der Wal AC, Winters GL (2011) 2011 consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology. Cardiovasc Pathol 21:245–274
Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB (2006) American Heart Association; Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; Council on Epidemiology and Prevention Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 113:1807–1816
Mueller KAL, Heinzmann D, Klingel K, Fallier-Becker P, Kandolf R, Kilias A, Walker-Allgaier B, Borst O, Kumbrink J, Kirchner T, Langer H, Geisler T, Schreieck J, Gramlich M, Gawaz M, Seizer P (2017) Histopathological and immunological characteristics of tachycardia-induced cardiomyopathy. J Am Coll Cardiol 69(17):2160–2172
Nakamura R, Egashira K, Machida Y, Hayashidani S, Takeya M, Utsumi H, Tsutsui H, Takeshita A (2002) Probucol attenuates left ventricular dysfunction and remodeling in tachycardia-induced heart failure: roles of oxidative stress and inflammation. Circulation 106:362–367
Nerheim P, Birger-Botkin S, Piracha L, Olshansky B (2004) Heart failure and sudden death in patients with tachycardia-induced cardiomyopathy and recurrent tachycardia. Circulation 110:247–252
Neumann T, Ravens U, Heusch G (1998) Characterization of excitation-contraction coupling in conscious dogs with pacing-induced heart failure. Cardiovasc Res 37:456–466
Ohlow MA, Michel C, Chen TH, Schmidt A, Saenger J, Lauer B, Brunelli M (2018) Predictors of long-term outcome in patients with biopsy-proven inflammatory cardiomyopathy. J Geriatr Cardiol 15:363–371
Ohlow MA, Chen TH, Schmidt A, Saenger J, Lauer B (2015) Clinical profile of patients with advanced age and inflammatory dilated cardiomyopathy on endomyocardial biopsy. J Geriatr Cardiol 12:605–612
Pabel S (2019) Functional and molecular mechanisms in tachycardia-mediated cardiomyopathy. Dtsch Med Wochenschr 144(15):46 (suppl.)
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur Heart J 37(27):2129–2200
Ravens U, Davia K, Davies CH, O’Gara P, Drake-Holland AJ, Hynd JW, Noble MI, Harding SE (1996) Tachycardia-induced failure alters contractile properties of canine ventricular myocytes. Cardiovasc Res 32:613–621
Shinbane JS, Wood MA, Jensen DN, Ellenbogen KA, Fitzpatrick AP, Scheinman MM (1997) Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol 29:709–715
Wijesurendra RS, Liu A, Eichhorn C, Ariga R, Levelt E, Clarke WT, Rodgers CT, Karamitsos TD, Bashir Y, Ginks M, Rajappan K, Betts T, Ferreira VM, Neubauer S, Casadei B (2016) Lone atrial fibrillation is associated with impaired left ventricular energetics that persists despite successful catheter ablation. Circulation 134:1068–1081
Zellner JL, Spinale FG, Eble DM, Hewett KW, Crawford FA Jr (1991) Alterations in myocyte shape and basement membrane attachment with tachycardia-induced heart failure. Circ Res 69:590–600
Zhang Y, Guallar E, Blasco-Colmenares E, Butcher B, Norgard S, Nauffal V, Marine JE, Eldadah Z, Dickfeld T, Ellenbogen KA, Tomaselli GF, Cheng A (2015) Changes in follow-up left ventricular ejection fraction associated with outcomes in primary prevention implantable cardioverter-defibrillator and cardiac resynchronization therapy device recipients. J Am Coll Cardiol 66(5):524–531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Spahic, T.‑H. Chen, J.C. Geller, J. Saenger, and M.‑A. Ohlow declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. This retrospective study was performed after consultation with the institutional ethics committee and in accordance with national legal requirements.
Rights and permissions
About this article
Cite this article
Spahic, A., Chen, TH., Geller, J.C. et al. Life in the fast lane: clinical and immunohistological characteristics of tachycardia-induced cardiomyopathy—a retrospective study in 684 patients. Herzschr Elektrophys 31, 292–300 (2020). https://doi.org/10.1007/s00399-020-00709-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-020-00709-4