Abstract
Purpose
To evaluate the possibility of using maternal anthropometric measurements for prediction of low birth weight in developing and developed countries.
Methods
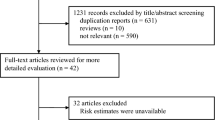
Bivariate diagnostic meta-analysis was performed with hierarchical summary receiver operating characteristic curves. Ten databases, i.e., PubMed, EMBASE, CINAHL, PsycINFO, Wiley InterScience, ProQuest Health and Medical Complete™, ProQuest Dissertations and Theses Database, the entire Cochrane Library (e.g., CENTRAL), Google Scholar, and Scopus were searched. The references and PubMed-related citations of potentially eligible articles and reviews were also investigated.
Results
With regard to maternal height, weight, arm circumference, abdominal circumference, body mass index (BMI), and weight gain, 111, 126, 25, 4, 131, and 59 studies extracted from 49, 38, 12, 1, 50, and 23 data sources, respectively, were finally included in the analysis. The sensitivity [=0.46, 95 % confidence interval (CI) 0.35–0.52 to 0.64, 95 % CI 0.56–0.71], specificity (=0.46, 95 % CI 0.38–0.54 to 0.72, 95 % CI 0.64–0.79) and diagnostic odds ratios (=2, 95 % CI 1–2 to 3, 95 % CI 3–4) for maternal height, weight, arm circumferences, BMI, and weight gain were low and 95 % confidence and prediction regions were too large for practical use. The findings for abdominal circumference were not generalizable because only one data source was available.
Conclusions
There is no evidence that maternal anthropometric measurements are good predictors of low birth weight.



Similar content being viewed by others
References
World Health Organization (2014) Feto-maternal nutrition and low birth weight. http://www.who.int/nutrition/topics/feto_maternal/en/. Accessed 18 March 2015
Temerinac D, Chen X, Sütterlin M et al (2014) Influence of fetal birth weight on perinatal outcome in planned vaginal births. Arch Gynecol Obstet 2014:313–318
Colman A, Maharaj D, Hutton J et al (2006) Reliability of ultrasound estimation of fetal weight in term singleton pregnancies. NZ Med J 119:U2146
Scioscia M, Scioscia F, Scioscia G et al (2015) Statistical limits in sonographic estimation of birth weight. Arch Gynecol Obstet 291:59–66
Malin G, Anblagan D, Bugg G et al (2014) PM. 39 diagnostic accuracy of antenatal magnetic resonance imaging (MRI) to predict birth weight 90th or 10th centile in the third trimester. Arch Dis Child Fetal Neonatal Ed 99(Suppl 1):94–95
Goto E (2013) Prediction of low birthweight and small for gestational age from symphysis-fundal height mainly in developing countries: a meta-analysis. J Epidemiol Community Health 67:999–1005
Peregrine E, O’Brien P, Jauniaux E (2007) Clinical and ultrasound estimation of birth weight prior to induction of labor at term. Ultrasound Obstet Gyncol 29:304–309
Baum JD, Gussman D, Wirth JC 3rd (2002) Clinical and patient estimation of fetal weight vs. ultrasound estimation. J Reprod Med 47:194–198
Goto E Diagnostic value of maternal anthropometric measurements for predicating low birthweight in developing countries: a meta-analysis. Asia Pac J Clin Nutr (in press)
World Health Organization (1995) Maternal anthropometry and pregnancy outcome. A WHO collaborative study. Bull World Health Organ 73(Suppl):1–98
World Health Organization (2006) The WHO child growth standards. http://www.who.int/childgrowth/en/. Accessed 18 March 2015
Villar J, Cheikh Ismail L, Victora CG (2014) International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st project. Lancet 384:857–868
Papageorghiou AT, Kennedy SH, Salomon LJ (2014) International standards for early fetal size and pregnancy dating based on ultrasound measurement of crown–rump length in the first trimester of pregnancy. Ultrasound Obstet Gynecol 44:641–648
The Oxford Maternal and Perinatal Health Institute, Green Templeton College, University of Oxford (2008) INTERGROWTH-21st Project. http://www.intergrowth21.org.uk/. Accessed 18 March 2015
Falck-Ytter Y, Motschall E (2004) New search filter for diagnostic studies: Ovid and Pubmed versions not the same. BMJ 328:1040
Whiting P, Rutjes AW, Reitsma JB et al (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25
Harbord RM, Whiting P (2009) Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. In: Sterne JAC (ed) Meta-analysis in Stata: an updated collection from the Stata Journal. Stata Press, Texas, pp 181–199
Reitsma JB, Glas AS, Rutjes AW et al (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Arends LR, Hamza TH, van Houwelingen JC et al (2008) Bivariate random effects meta-analysis of ROC curves. Med Decis Making 28:621–638
Jaeschke R, Guyatt GH, Sackett DL (1994) Users’ guides to medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The evidence-based medicine working group. JAMA 271:703–707
Swets JA (1988) Measuring the accuracy of diagnostic systems. Science 240:1285–1293
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Organisation for Economic Co-operation and Development (2012) The DAC list of ODA recipients. http://www.oecd.org/dac/stats/49483614.pdf. Accessed 18 March 2015
Ljimer JG, Mol BM, Heisterkap S et al (1999) Empirical evidence of design-related bias in studies of diagnostic tests. JAMA 282:1061–1066
Rutjes AW, Reitsma JB, Di Nisio M et al (2006) Evidence of bias and variation in diagnostic accuracy studies. CMAJ 174:469–476
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic accuracy was assessed. J Clin Epidemiol 58:882–893
Akobeng AK (2007) Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 96:644–647
Janjua NZ, Delzell E, Larson RR et al (2009) Determinants of low birth weight in urban Pakistan. Public Health Nutr 12:789–798
Villar J, Papageorghiou AT, Pang R et al (2014) The likeness of fetal growth and newborn size across non-isolated populations in the INTERGROWTH-21st project: the fetal growth longitudinal study and newborn cross-sectional study. Lancet Diabetes Endocrinol 2:781–792
Gardosi J, Figueras F, Clausson B et al (2011) The customised growth potential: an international research tool to study the epidemiology of fetal growth. Paediatr Perinat Epidemiol 25:2–10
Hutcheon JA, Zhang X, Cnattingius S et al (2008) Customised birthweight percentiles: does adjusting for maternal characteristics matter? BJOG 115:1397–1404
Egger M, Smith GD, Altman DG (2001) Systematic reviews in healthcare: meta-analysis in context, 2nd edn. BMJ, London
Centre for Reviews and Dissemination (2009) 2.2 Diagnostic tests. In: Systematic reviews: CRD’s guidance for undertaking reviews in health care. York, Centre for Reviews and Dissemination. http://www.york.ac.uk/inst/crd/pdf/Systematic_Reviews.pdf. Accessed 18 March 2015
Diagnostic Test Accuracy Working Group (2009) Handbook for DTA reviews. The cochrane collaboration. http://srdta.cochrane.org/handbook-dta-reviews. Accessed 18 March 2015
Acknowledgments
The author is grateful to the personnel of the Medical Library at the Japan Medical Association (Tokyo, Japan) who contributed to article retrieval. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goto, E. Maternal anthropometric measurements as predictors of low birth weight in developing and developed countries. Arch Gynecol Obstet 292, 829–842 (2015). https://doi.org/10.1007/s00404-015-3721-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3721-2