Abstract
Objective
To provide histological evidence to investigate a theory for post-tonsillectomy secondary hemorrhage (PTH) in a mouse model and to evaluate the potential for heparin-binding epidermal growth factor-like growth factor (HB-EGF) treatment on wound healing in this model.
Methods
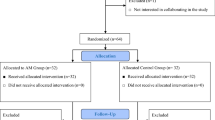
A prospective randomized single-blinded cohort study. A uniform tongue wound was created in 84 mice (day 0). Mice were randomized to HB-EGF (treatment, n = 42) or saline (control, n = 42). In treatment mice, HB-EGF 5 µg/ml was administered intramuscularly into the wound daily (days 0–14). In control mice, normal saline was administered daily. Three mice from each group were sacrificed daily through day 14 and the wounds evaluated histologically by blinded reviewers.
Results
Key stages of wound healing, including keratinocyte proliferation and migration, wound contraction, epithelial separation, and neoangiogenesis, are defined with implications for post-tonsillectomy wound healing. Epithelial separation (59 vs. 100%, p = 0.003) and wound reopening (8 vs. 48%, p < 0.001) were reduced with HB-EGF. Epithelial thickness (220 vs. 30 µm, p = 0.04) was greater with HB-EGF. Wound closure (days 4–5 vs. day 6, p = 0.01) occurred earlier with HB-EGF.
Conclusions
In healing of oral keratinocytes on muscle epithelial separation secondary to muscle, contraction occurs concurrently with neoangiogenesis in the base of the wound, increasing the risk of hemorrhage. This potentially explains why post-tonsillectomy secondary hemorrhage occurs and its timing. HB-EGF-treated wounds showed greater epithelial thickness, less frequent epithelial separation and wound reopening, and earlier wound closure prior to neovascularization, suggesting that HB-EGF may be a potential preventative therapy for PTH.
Level of evidence
NA—animal studies or basic research.

Illustration © Chris Gralapp


Illustration © Chris Gralapp


Similar content being viewed by others
References
Boss EF, Marsteller JA, Simon AE (2012) Outpatient tonsillectomy in children: demographic and geographic variation in the United States, 2006. J Pediatr 160:814–819
Cullen KA, Hall MJ, Golosinskiy A (2006) Ambulatory surgery in the United States. Natl Health Stat Rep 2009:1–25
Lafortune G, Balestat G, Durand A (2012) Comparing activities and performance of the hospital sector in Europe: how many surgical procedures performed as inpatient sand day cases? Directorate for Employment, Labour and Social Affairs, OECD, final report on work package II
Bhattacharyya N, Kepnes LJ (2014) Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope 124:1554–1556
Seshamani M, Vogtmann E, Gatwood J, Gibson TB, Scanlon D (2014) Prevalence of complications from adult tonsillectomy and impact on health care expenditures. Otolaryngol Head Neck Surg 150:574–581
Johnson LB, Elluru RG, Myer CM 3rd (2002) Complications of adenotonsillectomy. Laryngoscope 112:35–36
Gysin C, Dulguerov P (2013) Hemorrhage after tonsillectomy: does the surgical technique really matter? ORL J Oto-rhino-laryngol Relat Spec 75:123–132
Isaacson G (2012) Tonsillectomy healing. Ann Otol Rhinol Laryngol 121:645–649
Glim JE, van Egmond M, Niessen FB, Everts V, Beelen RH (2013) Detrimental dermal wound healing: what can we learn from the oral mucosa? Wound Repair Regen 21:648–660
Casteleyn C, Breugelmans S, Simoens P, Van den Broeck W (2011) The tonsils revisited: review of the anatomical localization and histological characteristics of the tonsils of domestic and laboratory animals. Clin Dev Immunol 2011:472460
Garber JC, Barbee RW, Bielitzki JT et al (2016) The guide for the care and use of laboratory animals. ILAR J 57
Santa Maria PL, Kim S, Varsak YK, Yang YP (2015) Heparin binding-epidermal growth factor-like growth factor for the regeneration of chronic tympanic membrane perforations in mice. Tissue Eng Part A 21:1483–1494
Santa Maria PL, Weierich K, Kim S, Yang YP (2015) Heparin binding epidermal growth factor-like growth factor heals chronic tympanic membrane perforations with advantage over fibroblast growth factor 2 and epidermal growth factor in an animal model. Otol Neurotol 36:1279–1283
Gwet K (2016) Handbook of inter-rater reliability: the definitive guide to measuring the extent of agreement among multiple reviewers. Advanced Analytics, Gaithersburg
Collison PJ, Mettler B (2000) Factors associated with post-tonsillectomy hemorrhage. Ear Nose Throat J 79:640–642 (644, 646 passim)
Krishna P, Lee D (2001) Post-tonsillectomy bleeding: a meta-analysis. Laryngoscope 111:1358–1361
Lowe D, van der Meulen J, National Prospective Tonsillectomy A (2004) Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet 364:697–702
Watson MG, Dawes PJ, Samuel PR et al (1993) A study of haemostasis following tonsillectomy comparing ligatures with diathermy. J Laryngol Otol 107:711–715
Blakley BW (2009) Post-tonsillectomy bleeding: how much is too much? Otolaryngol Head Neck Surg 140:288–290
Heidemann CH, Wallen M, Aakesson M, Skov P, Kjeldsen AD, Godballe C (2009) Post-tonsillectomy hemorrhage: assessment of risk factors with special attention to introduction of coblation technique. Eur Arch Oto-rhino-laryngol 266:1011–1015
Sarny S, Ossimitz G, Habermann W, Stammberger H (2011) Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 121:2553–2560
Shires CB, Saputra JM, King L et al (2012) Histopathological and postoperative behavioral comparison of rodent oral tongue resection: fiber-enabled CO2 laser versus electrocautery. Otolaryngol Head Neck Surg 147:716–721 (Epub 2012 Apr 2024)
Lee SK, Lee SS, Song IS et al (2004) Paradoxical effects of elastase inhibitor guamerin on the tissue repair of two different wound models: sealed cutaneous and exposed tongue wounds. Exp Mol Med 36:259–267
Dorr W, Spekl K, Farrell CL (2002) The effect of keratinocyte growth factor on healing of manifest radiation ulcers in mouse tongue epithelium. Cell Prolif 35:86–92
Usui ML, Underwood RA, Mansbridge JN, Muffley LA, Carter WG, Olerud JE (2005) Morphological evidence for the role of suprabasal keratinocytes in wound reepithelialization. Wound Repair Regen 13:468–479
Evrard L, Nammour S, Dourov N (1996) Scanning electron microscopic and immunocytochemical studies of contraction during secondary CO2 laser wound healing in rat tongue mucosa. J Oral Pathol Med 25:72–77
Marikovsky M, Vogt P, Eriksson (1996) Eet al. Wound fluid-derived heparin-binding EGF-like growth factor (HB-EGF) is synergistic with insulin-like growth factor-I for Balb/MK keratinocyte proliferation. J Investig Dermatol 106:616–621
Shirakata Y, Kimura R (2005) Nanba Det al. Heparin-binding EGF-like growth factor accelerates keratinocyte migration and skin wound healing. J Cell Sci 118:2363–2370
Johnson NR, Wang Y (2015) Coacervate delivery of HB-EGF accelerates healing of type 2 diabetic wounds. Wound Repair Regen 23:591–600
Besner G, Higashiyama S, Klagsbrun M (1990) Isolation and characterization of a macrophage-derived heparin-binding growth factor. Cell Regul 1:811–819
Davis-Fleischer KM, Besner GE (1998) Structure and function of heparin-binding EGF-like growth factor (HB-EGF). Front Biosci J Virtual Libr 3:d288–d299
Murayama Y, Miyagawa J, Higashiyama S et al (1995) Localization of heparin-binding epidermal growth factor-like growth factor in human gastric mucosa. Gastroenterology 109:1051–1059
Nakagawa T, Hayase Y, Sasahara M (1997) Distribution of heparin-binding EGF-like growth factor protein and mRNA in the normal rat kidneys. Kidney Int 51:1774–1779
Santa Maria PL, Kim S, Yang YP (2016) No systemic exposure of transtympanic heparin-binding epidermal growth factor like growth factor. Drug Chem Toxicol 39:451–454
Solares CA, Koempel JA, Hirose K et al (2005) Safety and efficacy of powered intracapsular tonsillectomy in children: a multi-center retrospective case series. Int J Pediatr Otorhinolaryngol 69:21–26
Lowe D, van der Meulen J, Cromwell D et al (2007) Key messages from the national prospective tonsillectomy audit. Laryngoscope 117:717–724
Tomkinson A, Harrison W, Owens D, Harris S, McClure V, Temple M (2011) Risk factors for postoperative hemorrhage following tonsillectomy. Laryngoscope 121:279–288
Praveen CV, Parthiban S, Terry RM (2013) High incidence of post-tonsillectomy secondary haemorrhage following coblation tonsillectomy. Indian J Otolaryngol Head Neck Surg 65:24–28
Setabutr D, Adil EA, Adil TK, Carr MM (2011) Emerging trends in tonsillectomy. Otolaryngol Head Neck Surg 145:223–229
Koltai PJ, Solares CA, Mascha EJ, Xu M (2002) Intracapsular partial tonsillectomy for tonsillar hypertrophy in children. Laryngoscope 112:17–19
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This project was funded by the Garnett Passe and Rodney Williams Memorial Foundation, Stanford’s SPARK, and the Stanford Child Health Research Institute.
Conflict of interest
Authors DMB, CSM, RC, and PSM are inventors on a patent, owned by Stanford University, which covers subject matter in this study. Author NFA has no conflict of interest.
Ethical standards
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Beswick, D.M., Santa Maria, C., Ayoub, N.F. et al. Epithelial separation theory for post-tonsillectomy secondary hemorrhage: evidence in a mouse model and potential heparin-binding epidermal growth factor-like growth factor therapy. Eur Arch Otorhinolaryngol 275, 569–578 (2018). https://doi.org/10.1007/s00405-017-4810-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4810-6