Abstract
The clinical diagnosis of Huntington’s disease (HD) is based on the motor symptoms, although these can be preceded by cognitive and behavioral changes. Biomarker studies have shown that structural imaging modalities are useful biomarkers of HD onset, while functional imaging measures have been studied less often for this purpose. Our aim was to investigate the combined value of 18-fluorodesoxyglucose (FDG)–PET and cognitive measures as biomarkers of HD onset. Twenty-two premanifest mutation carriers of HD (PMCs) and 11 healthy controls were assessed twice with FDG–PET scan, neurological and neuropsychological assessments over a 2-year interval. Seventeen PMCs had an additional third neurological evaluation, 10 years after baseline. Disease load was defined as the probability of motor onset within 5 years. Metabolism in putamen, caudate and pallidum of PMCs was significantly lower than that of controls, at both assessments. Almost half of the PMCs had converted to manifest HD 10 years later and all converters had low average or abnormal putaminal metabolism at 2 year follow-up. In contrast, all PMCs with normal putaminal metabolism at 2 year follow-up remained premanifest during the following 8 years. Furthermore, glucose metabolism of putamen explained a substantial part of the variance in disease load. A composite score of psychomotor tests contributed significantly to the prediction model as well, while cognitive performance was comparable for PMCs and controls. We conclude that in future clinical trials a combination of psychomotor tests and putaminal glucose metabolism may be used to identify PMCs close to motor onset of HD.
Similar content being viewed by others
Introduction
Huntington’s disease (HD) is an autosomal-dominant neurological disease characterized by progressive impairment of motor function, cognitive deterioration and psychiatric and behavioral symptoms. The underlying genetic defect is an expansion of a CAG trinucleotide repeat in the Huntingtin gene on chromosome 4, making predictive testing of at-risk individuals possible [1]. Currently, the clinical diagnosis of HD is based on the presence of characteristic and specific motor signs, confirmed by a positive genetic test result or a family history of HD. Up till now, gene mutation carriers without evident motor signs are considered to be in the premanifest stage of HD (premanifest mutation carriers: PMCs). Nevertheless, in PMCs cognitive impairment may be present before the onset of motor signs [2, 3]. Different HD phenotypes can already be distinguished in this premanifest stage, such as predominant cognitive impairment, behavioral impairment and cognitive preservation [4]. The age of onset of motor symptoms is variable and inversely related to the CAG repeat length [5, 6]. The exact moment of conversion to clinical HD cannot be predicted for an individual mutation carrier, but the probability of onset of motor signs within 5 years can be calculated with the Langbehn formula [7]. Although to date no cure is available, it would be helpful in identifying mutation carriers that are relatively close to clinical HD; thus, facilitating statistical power and efficacy of future disease-modifying intervention trials.
Data from two large multisite biomarker studies have shown that cognitive, imaging, sensory, and motor measures can be used as quantifiable endpoints in such clinical trials [8, 9]. With respect to cognitive biomarkers, measures of emotion recognition, psychomotor speed, working memory, and executive function are most sensitive to early cognitive changes in PMCs, sometimes even up to a decade before the estimated motor onset [3, 10]. Structural brain imaging measures are most effective for detecting early changes in the brains of PMCs, revealing reduced volumes of striatum and white matter [11]. Functional imaging changes such as reduced dopamine D2 receptor binding and alterations in brain glucose metabolism, even a specific HD related pattern of metabolism, may precede these structural changes in PMC brains [12–15]. Increases in regional glucose metabolism may reflect compensation for early neuronal loss or dysfunction; decline in these measures may herald clinical onset [16]. However, insufficient data are available about how exactly in PMCs functional imaging parameters change over time and whether cortical degeneration precedes or follows subtle striatal changes in HD [17]. Tang et al. [18] found recently that metabolic network measurements provide a sensitive method to quantify disease progression in premanifest HD. The relationship between the onset of cognitive dysfunction and the underlying neuropathological and structural changes remains unclear [10].
A combination of functional imaging and cognitive biomarkers may provide better prediction of HD onset than single measures [17]. We combined 18-fluorodesoxyglucose (FDG)–PET measurements with cognitive assessments in a PMC cohort that was examined longitudinally. Previously, we could not detect a significant decline in striatal glucose metabolism or dopamine D2 receptor (raclopride) binding in these subjects over a 2-year period, although both measures were lower than in controls [19]. Now we re-analyzed the FDG-PET data in relation to the cognitive measures. We wanted to know which combinations of metabolic and cognitive measures best predict the probability of motor onset within 5 years for our cohort. In retrospect we were able to stratify our PMC cohort in those far from and those close to motor onset of HD at baseline; this could be achieved by a repeat neurological evaluation 10 years after the first assessments.
Materials and methods
Participants
The participants are part of the original cohort of 27 PMCs and 14 controls (Cs) that has been described in detail earlier [15, 19]. All subjects underwent predictive genetic testing for HD at the University Medical Center Groningen (UMCG) or the Leiden University Medical Center (LUMC) and all gave their written informed consent. Those subjects with a CAG repeat length of 36 or more, without HD motor signs (motor score below 5) on the Unified Huntington’s Disease Rating Scale (UHDRS) [20] were considered PMCs. For PMCs the probability of motor onset within 5 years, given a person’s current age and CAG repeat length was obtained from the Langbehn formula [7]:
This ‘disease load’ at baseline was on average 0.21 with a median of 0.16; at follow-up this had only slightly increased towards 0.25 (Table 1). Individuals from HD families without the HD mutation participated as controls (Co). At baseline, all participants had a normal neurological examination and MRI scans were normal. Furthermore all participants had an mini mental status examination score higher than 24 [21]. The educational level was scored with a Dutch classification scale [22].
Of the original group of 41, 33 participants (22 PMCs and 11 Co) were seen after 2 years (see Fig. 1). The reason for drop out was self-withdrawal (n = 4) or technical failures in obtaining repeat PET-scans (n = 4). We analyzed the baseline (T0) and follow-up (T1) results from the FDG–PET scan and neuropsychological assessment (NPA). Data were complete for nearly all participants, except for 2 PMCs who had missing data for NPA at T0 and two Co by whom FDG–PET scans could not be carried out successfully.
Flow chart of participants and drop out during follow up. T0 baseline, T1 follow up two-and-a-half years after baseline, T2 follow up 10 years after baseline, PMCs premanifest mutation carriers of Huntington’s disease, Co controls NA neurological assessment, PET positron emission tomography, NPA neuro psychological assessment
5 of the 22 PMCs did not have a neurological examination 10 years after baseline; 3 persons could not be contacted anymore and 2 PMCs declined further participation. 8 of the remaining 17 PMCs (47 %) had converted to the clinical (motor) stage of HD (UHDRS motor score: M = 11.9; SD = 4.2) after 10 years. The other 9 PMCs did not have significant motor symptoms (UHDRS motor score: M = 4.8; SD = 3.5) at that time. Those PMCs that had converted to HD during the 10 years are hereafter designated as PMCs close to motor onset of HD (PMC ‘close’), the other 9 PMCs are designated as PMCs far from motor onset of HD (PMC ‘far’). The PMCs and Co were comparable with respect to age, educational level and gender (Table 1). The two PMC subgroups (‘close’ and ‘far’) had comparable demographic characteristics as well (Table 1). The disease load for PMCs ‘close’ was higher than for PMCs ‘far’, but this did not reach significance. UHDRS total functional capacity at baseline was comparable for both PMC subgroups (scores 12 or 13).
Procedure
Neurological assessment and assessments of FDG–PET scans were done by a single blinded movement disorder neurologist at the UMCG (JvO). The NPA took place in a fixed order and was carried out by trained neuropsychologists, either at the UMCG (MHD) or the LUMC (MNW, CKJ). All subjects were tested and scanned twice, with a mean interval of about 2.5 years. For most subjects the NPA was performed prior to the FDG–PET scan on 1 or 2 subsequent days, with a maximum interval of 3 months. At baseline this could unfortunately not be realised for a subgroup of our participants (median interval = 9 months, range 0–21 months). Neurological assessment 10 years after baseline was carried out by a movement disorder neurologist.
Measures
Neuropsychological assessment
NPA took place based on the CAPIT-HD protocol [23]. In the current study we analyzed the results of only those tests known to be sensitive to early cognitive change in premanifest HD: the stroop colour word test [24], the trail making test (TMT) [25] and the symbol digit modalities test (SDMT) [26]. In addition we analyzed scores on letter fluency (FAS) [27] and some subtests of the Wechsler memory scale (WMS); logical memory (total immediate recall), digit span (forward and backward) and associate learning [28].
Test scores were analysed separately, but were also combined to represent three cognitive domains: psychomotor speed (PmS), memory (M) and executive function (EF). Stroop and SDMT scores, both representing the number of correct answers, were transformed to time scores (time needed to complete the whole test). Subsequently, all test scores were converted to z-scores based on the means and standard deviations of the control data. The PmS score was calculated as the non-weighted average z-score of time scores on the stroop colour naming, stroop word reading, SDMT and TMT part A. The same was done for the M score based on the WMS subtasks logical memory immediate recall, associate learning, and digit span forward, representing working memory and episodic memory. The EF score contains the non-weighted average z-score for the stroop interference index (interference card/colour card), the TMT index (part B/part A), the digit span backwards total correct span and the letter fluency (using the letters F-A-S; total correct answers). This combined EF score represents aspects of inhibitory control, cognitive flexibility, generating and manipulating information from memory.
Imaging measures
Static 18-fluorodesoxyglucose (FDG)-PET scans were performed and analyzed according to previously published protocols [15, 19], aiming to minimize variability due to operator and analysis factors. We expressed FDG–PET data as a normalized regional glucose metabolic index (GMI), indicating regional activity relative to average brain metabolism. The results are presented as means of left and right GMI. We analyzed GMI in the caudate nucleus, putamen, pallidum, and dorsolateral prefrontal cortex (DLPFC). The latter was composed as an average score of the Montreal Neurological Institute (MNI) coordinates for superior and middle frontal gyrus.
Statistical analyses
Given the great individual variability in onset and presentation of first cognitive symptoms, we also calculated individual classification scores for PmS, M, and EF as well as GMI in each selected brain region. These classification scores were considered ‘abnormal’ for an individual when below two standard deviations (SD) of the control mean (M), ‘low average’ when between one and two SD below M and ‘normal’ above one SD below the control mean.
Data were analyzed with IBM SPSS statistics 20 for Windows. Nonparametric tests were used since the data were not normally distributed and the sample size is rather small. Group comparisons were made with Chi-squared tests and Mann–Whitney tests when appropriate. General linear model repeated measures Ancova analyses were carried out to analyze possible group, time, and interaction effects for the cognitive and imaging data. The age was included as a covariate to control for possible age-related differences within and between groups. For correlations between the measures, partial correlations were computed, controlling for the influence of age as well. Spearman’s Rho was computed when appropriate. Linear regression analyses were carried out to analyze the contribution of these variables to the prediction of disease load. We took one-sided alpha levels, since we expected the PMC group to perform worse on all measures as compared to Co. For post hoc multiple comparisons, the Bonferroni–Holm correction was applied [29].
Results
Group comparisons
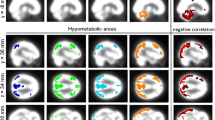
PMCs showed a significantly lower glucose metabolism than Co in putamen [F(1, 28) = 17.3, p = 0.0001], caudate nucleus [F(1, 28) = 5.5, p = 0.01] and pallidum [F(1, 28) = 5.3, p = 0.01] at T0 as well as at T1 (Table 2). Frontal metabolism was comparable for both groups at both assessments. Furthermore, group analyses for the cognitive measures did not reveal any significant differences between PMCs and Co at both assessments. Additional comparisons between PMCs ‘far’ and PMCs ‘close’ did not show any significant differences as well, neither on imaging, nor on cognition measures. All scores remained stable during the 2 year follow-up period, for PMCs as well as Co (Table 2).
Individual performances
The frequencies of individual classifications of glucose metabolism and cognitive performance (normal, low average, abnormal) of both PMCs and Co are shown in Table 3. PMCs had significantly more abnormal putaminal GMI scores than Co at T0 (p = 0.0006) as well as at T1 (p = 0.0002). Fourteen PMCs (63.6 %) had an abnormal putaminal classification score at T0, while 3 PMCs (13.6 %) had a low average score and 5 PMCs (22.8 %) had a normal score. At T1, 11 PMCs (50 %) had an abnormal score for putaminal metabolism, while 5 PMCs (22.7 %) had a low average score and 6 PMCs (27.3 %) had a normal score. Further inspection of the data shows that 11 of the original 14 PMCs with abnormal putaminal metabolism at baseline still had an abnormal score at follow-up. The other 3 PMCs with an abnormal putaminal score at baseline now had a low average putaminal score at T1. The caudate, DLPFC and pallidum showed comparable distributions of these scores for PMCs and Cs at both assessments.
As to cognitive performance, PMCs had significantly worse baseline scores on psychomotor speed (PmS) than Co (p = 0.015): 20 % of PMCs had an abnormal PmS score, 15 % had a low normal PmS score and 65 % had a normal PmS score, while all Co had normal scores. At T1 the distributions of PmS scores were comparable for PMCs and Co. Classification scores for executive function (EF) and memory (M) were comparable as well, at both assessments.
In retrospect, when comparing on these classification scores PMCs ‘far’ and PMCs ‘close’, we only found a borderline significant difference for putaminal GMI (p = 0.04) at T1. More specifically, all PMCs ‘close’ then had an abnormal or low average putaminal score and none of them had a normal putaminal score, while 45 % of PMCs ‘far’ still had a normal putaminal GMI score. In other words, none of the PMCs with still a normal putaminal score at T1, had developed motor symptoms of HD 10 years after baseline (T2). PMCs ‘far’ and PMCs ‘close’ had comparable distributions on the other imaging and cognition classification scores at both measurements (see Table 3).
To find out whether the classification scores of PMCs glucose metabolism and cognitive performance were correlated to each other, Spearman correlations were computed (the results are shown in Table 4). After Bonferroni–Holm correction, we did not find any significant correlations between the individuals imaging and cognitive classification scores, but at T0 a trend was seen for a positive correlation between glucose metabolism in caudate and PmS performance (p = 0.02). At T1 a comparable trend was found (p = 0.03) and additional even stronger trends were seen for positive correlations of PmS with pallidum and putamen metabolism (p = 0.01 and p = 0.02, respectively).
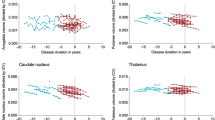
Correlations between disease load and other measures
Table 5 shows that the conditional probability of onset of motor symptoms within 5 years (disease load) from T0 was most strongly and negatively correlated with putaminal metabolism (p ≤ 0.001) and the PmS score (p ≤ 0.001), after correction for age. All the separate test scores that PmS consists of, as well as the WMS logical memory score, were also significantly correlated with disease load (p values between 0.003 and 0.01). In addition striatal and pallidal metabolism showed significant negative correlations with disease load (p = 0.004 and p = 0.005, respectively).
At T1, comparable and in part even stronger results were found (Table 5). In addition disease load was now significantly correlated with the colour word card of the stroop test (p = 0.01) and the TMT part B (p = 0.03).
Prediction model
The measures with the highest, significant, correlations with disease load at T0 (see Table 5) were included, one by one, in a linear regression analysis. Age did not contribute significantly to the model and was therefore left out of the analyses. The largest adjusted R 2 for the contributions of the separate measures to disease load were found for the PmS score (45 %) and putaminal GMI (44 %); F(1, 19) = 16.32, p ≤ 0.001 and F(1, 21) = 17.73, p ≤ 0.001, respectively (see Table 6). Most psychomotor (sub-) tests contributed significantly to the variance in disease load. The SDMT explained 35 % of total variance, TMT part A 26 %, stroop colour naming card 25 % and the stroop word reading card explained 23 % of total variance (corrected p values between 0.002 and 0.01). The WMS subtest logical memory explained 22 % of the variance in disease load (p = 0.01). Of the imaging measures the pallidal GMI accounted for 24 % of the variance (p = 0.007) but the caudate GMI did not contribute significantly to disease load.
Given the small sample size the final prediction model was restricted to a maximum of three predictors that were entered together, in a multiple linear regression model. The best model for predicting disease load at baseline consisted of the putaminal GMI and the PmS score, together explaining 67 % of the total variance in disease load; F(2, 19) = 20.06, p < 0.001, described in the following regression formula: disease load = 1.94–1.61 × GMI Putamen + 0.078 × PmS.
The same regression analyses were carried out for the T1 data and resulted in comparable, even stronger findings. Putaminal GMI and PmS together explained 68 % of total variance in disease load [F(2, 21) = 22.87, p < 0.001], now yielding the following equation: disease load = 1.19–0.89 × GMI Putamen + 0.11 × PmS.
Discussion
We studied a well-defined group of premanifest mutation carriers of HD with imaging and cognitive assessment at two time points, 2 years apart, in order to identify the best combination of clinical markers to predict the probability of HD motor onset. This motor onset could be determined accurately as patients were re-assessed 10 years after the initial examination. The combination of glucose metabolism in putamen and a composite score for psychomotor speed accounts for two-thirds of variance in the calculated probability of motor onset within 5 years. This model holds true—and thus should be considered validated—for measurements obtained at 2-year-follow-up. The relevance of combined clinical measures in predicting disease onset and disease progression had been established before [8, 9, 30], as well has the value of FDG–PET to detect early functional brain changes in PMCs [14]. Our study is the first to show that the combination of FDG–PET and cognitive (psychomotor speed) measures has significant predictive value.
Our functional imaging data replicate earlier findings on metabolic alterations in premanifest HD. We showed that putaminal metabolism was abnormal in almost two-thirds of PMCs at baseline and in half of PMCs at 2-year-follow-up. This slight paradoxical decrease in the number of abnormal putaminal metabolism scores may be explained by the phenomenon of ‘regression towards the mean’. We made a rather artificial classification for individual imaging and cognitive performances on the basis of z-scores. Three PMCs with an abnormal putaminal score at baseline (z-scores slightly below−2), ‘improved’ to the low average level at follow-up (with z-scores slightly above−2), while their absolute putaminal scores did not change that much. Furthermore, the average putaminal metabolism of the PMC group remained stable during follow-up. We also found abnormal caudate and pallidal metabolism in smaller subgroups of our cohort; however, these were not significantly different from Co. In line with the previous evidence, this illustrates that the striatum is one of the first brain regions affected in HD [15, 16, 31]. In contrast to some other studies [11], we found metabolic alterations to be most profound in the putamen, whereas they found the caudate nucleus to show the first (structural) changes in HD. We did not find a significant difference in DLPFC metabolism for PMCs as compared to controls. This is in contrast with Wolf et al. [32], who found left DLPFC hypo activation in PMCs with increasing working memory load, while cognition was still preserved. An explanation for this may be that different paradigms were used, putting another demand on DLPFC function of PMCs; i.e., during task performance with event-related fMRI (the Wolf study) and in resting state with static FDG–PET (this study). Yet, Wolf et al. did not find any differences in striatal activation for PMCs and controls, while in our cohort the striatum is clearly affected in a substantial part of PMCs. Perhaps, the Wolf cohort was still farther from expected motor onset than our cohort. Their PMCs indeed seem on average slightly younger, with slightly lower CAG repeat lengths. It could be that the earliest functional changes in DLPFC are best demonstrated while the brain is confronted with higher cognitive demands; comparison of the two imaging paradigms in a larger PMC cohort may elucidate the discrepancy in findings on DLPFC function in PMCs.
In our study psychomotor tasks are particularly sensitive to cognitive decline in premanifest HD, which is in line with the literature [2, 10]. In addition, our data suggest that a composite score of several psychomotor tasks performance may have better predictive value than the test scores separately. Harrington et al. [33] recently suggested that two factors, ‘motor planning/speed’ and ‘sensory-perceptual processing’, may be the best indicators of time to diagnosis, after controlling for disease load and motor function. However, as the authors mentioned, the tests they employed are experimental and lack normative data [33]. In contrast, the tests we included possess established clinical usefulness, already. It must be mentioned although, that some PMCs already had abnormal psychomotor speed before onset of overt motor symptoms, while others performed within normal range. These individual scores of psychomotor speed performance showed trends of meaningful correlations with regional striatal metabolism, which is in line with the earlier evidence from (structural) imaging studies [34, 35]. Nearly all PMCs had normal scores with respect to executive function and memory and this is in line with the existing evidence that alterations in information processing speed precede memory and executive dysfunction in PMCs [8, 36]. Cognitive performance did not change over the 2 years, in line with reports by others [37, 38]. Our results are in line with several studies that have shown a discrepancy between the progression of brain atrophy on structural MRI in the preclinical phase and stable, largely intact cognitive and clinical functioning [11]. This means, that in a situation of progressive neuronal cell loss, compensatory mechanisms must be at play to minimize functional effects of these changes. In addition, during increasing exposure to mutant huntingtin, neuronal dysfunction probably precedes neuronal cell death. In this situation it may not be surprising, that a combination of functional imaging (i.e., FDG–PET) and NPA appears as the most sensitive combined measure for predicting HD motor onset in our study.
We had the unique opportunity to evaluate the neurological status of 17 of the 22 PMCs 10 years after baseline, thus enabling us to classify these subjects in retrospect as either far from or close to HD motor onset at study entry. Eight PMCs were diagnosed with manifest HD after 10 years and none had normal putaminal glucose metabolism scores at follow-up, about 8 years earlier. Of the other 9 PMCs, who did not develop motor symptoms during the study, 4 PMCs had normal putaminal glucose metabolism scores at follow-up. Statistical analyses showed a trend for worse putaminal metabolism at 2-year follow-up of PMCs close to motor onset as compared to PMCs far from motor onset. Cognition scores were comparable for both subgroups. Although one must be cautious given the small number of participants, a normal putaminal glucose metabolism score may imply that a PMC will not develop motor symptoms within 8 years.
The strengths of this biomarker study lie in the longitudinal design in which a well characterized cohort of PMCs was assessed using several clinical measures. Particularly the third neurological evaluation at 10 years after baseline provided us with important information about the actual closeness to motor onset of HD for most of our subjects, although we cannot say at what moment during follow they actually converted to HD. Limitations of our study are the small sample size, drop out, and incomplete data for a few subjects. Furthermore, radiation exposure, ligand production, and cost may limit the use of FDG–PET scanning. However, in recent years, FDG–PET has become more widely available, mainly through markedly increased demands for oncological patients. It will be important to validate our results in a much larger cohort to make sure that these still hold within a heterogeneous population of PMCs.
In conclusion, we found a combination of functional imaging and cognitive measures to be of predictive value for motor onset of HD within 5 years. More specifically, the combination of glucose metabolism of the putamen and a composite score for psychomotor speed is a powerful and better predictor of motor onset of HD than each measure separately. The additional information about the real neurological status of most PMCs (half of them converted to manifest HD) 10 years after baseline, supports this conclusion. The presented model explained a large part of the variance in the motor onset measure at baseline, and an even higher amount after 2 years follow-up. Therefore, in future clinical trials a combination of the SDMT, TMT, stroop colour word test and putaminal glucose metabolism can be used to identify late-converter-PMCs.
References
The Huntington’s Disease Collaborative Research Group (1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell 72(6):971–983
Kirkwood SC, Siemers E, Hodes ME, Conneally PM, Christian JC, Foroud T (2000) Subtle changes among presymptomatic carriers of the Huntington’s disease gene. J Neurol Neurosurg Psychiatry 69(6):773
Paulsen JS, Zhao H, Stout JC, Brinkman RR, Guttman M, Ross CA, Como P, Manning C, Hayden MR, Shoulson I, Huntington Study Group (2001) Clinical markers of early disease in persons near onset of Huntington’s disease. Neurology 57(4):658–662
Biglan KM, Zhang Y, Long JD, Geschwind M, Kang GA, Killoran A, Lu W, McCusker E, Mills JA, Raymond LA, Testa C, Wojcieszek J, Paulsen JS, PREDICT-HD Investigators of the Huntington Study Group (2013) Refining the diagnosis of Huntington disease: the PREDICT-HD study. Front Aging Neurosci 5:12. doi:10.3389/fnagi.2013.00012
Andrew SE, Goldberg YP, Kremer B, Telenius H, Theilmann J, Adam S, Starr E, Squitieri F, Lin B, Kalchman MA (1993) The relationship between trinucleotide (CAG) repeat length and clinical features of Huntington’s disease. Nat Genet 4(4):398–403. doi:10.1038/ng0893-398
Duyao M, Ambrose C, Myers R, Novelletto A, Persichetti F, Frontali M, Folstein S, Ross C, Franz M, Abbott M et al (1993) Trinucleotide repeat length instability and age of onset in Huntington’s disease. Nat Genet 4(4):387–392. doi:10.1038/ng0893-387
Langbehn DR, Brinkman RR, Falush D, Paulsen JS, Hayden MR, International Huntington’s Disease Collaborative Group (2004) A new model for prediction of the age of onset and penetrance for Huntington’s disease based on CAG length. Clin Genet 65(4):267–277. doi:10.1111/j.1399-0004.2004.00241.x
Paulsen JS, Langbehn DR, Stout JC, Aylward E, Ross CA, Nance M, Guttman M, Johnson S, MacDonald M, Beglinger LJ, Duff K, Kayson E, Biglan K, Shoulson I, Oakes D, Hayden M, PREDICT-HD Investigators and Coordinators of the Huntington Study Group (2008) Detection of Huntington’s disease decades before diagnosis: the PREDICT-HD study. J Neurol Neurosurg Psychiatry 79(8):874–880
Tabrizi SJ, Langbehn DR, Leavitt BR, Roos RA, Durr A, Craufurd D, Kennard C, Hicks SL, Fox NC, Scahill RI, Borowsky B, Tobin AJ, Rosas HD, Johnson H, Reilmann R, Landwehrmeyer B, Stout JC, TRACK-HD investigators (2009) Biological and clinical manifestations of Huntington’s disease in the longitudinal TRACK-HD study: cross-sectional analysis of baseline data. Lancet Neurol 8(9):791–801. doi:10.1016/S1474-4422(09)70170-X
Stout JC, Paulsen JS, Queller S, Solomon AC, Whitlock KB, Campbell JC, Paulsen JS, Queller S, Solomon AC, Whitlock KB, Campbell JC, Carlozzi N, Duff K, Beglinger LJ, Langbehn DR, Johnson SA, Biglan KM, Aylward EH (2011) Neurocognitive signs in prodromal Huntington disease. Neuropsychology 25(1):1–14. doi:10.1037/a0020937
Tabrizi SJ, Reilmann R, Roos RA, Durr A, Leavitt B, Owen G, Jones R, Johnson H, Craufurd D, Hicks SL, Kennard C, Landwehrmeyer B, Stout JC, Borowsky B, Scahill RI, Frost C, Langbehn DR, TRACK-HD investigators (2012) Potential endpoints for clinical trials in premanifest and early Huntington’s disease in the TRACK-HD study: analysis of 24 month observational data. Lancet Neurol 11(1):42–53. doi:10.1016/S1474-4422(11)70263-0
Kuhl DE, Markham CH, Metter EJ, Riege WH, Phelps ME, Mazziotta JC (1985) Local cerebral glucose utilization in symptomatic and presymptomatic Huntington’s disease. Res Publ Assoc Res Nerv Ment Dis 63:199–209
Antonini A, Leenders KL, Spiegel R, Meier D, Vontobel P, Weigell-Weber M, Sanchez-Pernaute R, de Yébenez JG, Boesiger P, Weindl A, Maguire RP (1996) Striatal glucose metabolism and dopamine D2 receptor binding in asymptomatic gene carriers and patients with Huntington’s disease. Brain J Neurol 119(6):2085–2095
Feigin A, Leenders KL, Moeller JR, Missimer J, Kuenig G, Spetsieris P, Antonini A, Eidelberg D (2001) Metabolic network abnormalities in early Huntington’s disease: an [18F]FDG PET study. J Nucl Med 42(11):1591–1595
Van Oostrom JCH, Maguire RP, Verschuuren-Bemelmans CC, Veenma-van der Pruim J, Roos RAC, Leenders KL (2005) Striatal dopamine D2 receptors, metabolism, and volume in preclinical Huntington disease. Neurology 65(6):941–943
Feigin A, Tang C, Ma Y, Mattis P, Zgaljardic D, Guttman M, Paulsen JS, Dhawan V, Eidelberg D (2007) Thalamic metabolism and symptom onset in preclinical Huntington’s disease. Brain J Neurol 130(11):2858–2867
Paulsen JS (2009) Functional imaging in Huntington’s disease. Exp Neurol 216(2):272–277. doi:10.1016/j.expneurol.2008.12.015
Tang CC, Feigin A, Ma Y, Habeck C, Paulsen JS, Leenders KL, Teune LK, van Oostrom JCH, Guttman M, Dhawan V, Eidelberg D (2013) Metabolic network as a progression biomarker of premanifest Huntington’s disease. J Clin Investig 123(9):4076–4088. doi:10.1172/JCI69411
Van Oostrom JCH, Dekker M, Willemsen AT, De Jong BM, Roos RA, Leenders KL (2009) Changes in striatal dopamine D2 receptor binding in pre-clinical Huntington’s disease. Eur J Neurol 16(2):226–231. doi:10.1111/j.1468-1331.2008.02390.x
Huntington Study Group (1996) Unified Huntington’s disease rating scale: reliability and consistency. Mov Disord 11(2):136–142
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Verhage F (1964) Intelligentie en leeftijd: Onderzoek bij Nederlanders van twaalf tot zevenenzeventig jaar (Proefschrift). Van Gorcum, Assen
Quinn N, Brown R, Craufurd D, Goldman S, Hodges J, Kieburtz K, Lindvall O, MacMillan J, Roos R (1996) Core assessment program for intracerebral transplantation in Huntington’s disease (CAPIT-HD). Mov Disord 11(2):143–150
Stroop JR (1935) Studies of interference in serial verbal reactions. J Exp Psychol 18:643–662
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 8:271–276
Smith A (1968) The symbol digit modalities test: a neuropsychologic test for economic screening of learning and other cerebral disorders. Learn Disord 3:83–91
Benton AL (1976) Multilingual aphasia examination. University of Iowa Press, Iowa City
Wechsler DA (1945) A standardized memory scale for clinical use. J Psychol 19:87–95
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70
Tabrizi SJ, Scahill RI, Owen G, Durr A, Leavitt BR, Roos RA, Borowsky B, Landwehrmeyer B, Frost C, Johnson H, Craufurd D, Reilmann R, Stout JC, Langbehn DR, The TRACK-HD Investigators (2013) Predictors of phenotypic progression and disease onset in premanifest and early-stage Huntington’s disease in the TRACK-HD study: analysis of 36-month observational data. Lancet Neurol 12(7):637–649. doi:10.1016/S1474-4422(13)70088-7
Aylward EH, Brandt J, Codori AM, Mangus RS, Barta PE, Harris GJ (1994) Reduced basal ganglia volume associated with the gene for Huntington’s disease in asymptomatic at-risk persons. Neurology 44(5):823–828
Wolf RC, Vasic N, Schönfeldt-Lecuona C, Landwehrmeyer GB, Ecker D (2007) Dorsolateral prefrontal cortex dysfunction in presymptomatic Huntington’s disease: evidence from event-related fMRI. Brain nov 130(Pt 11):2845–2857 Epub 2007 sep 13
Harrington DL, Smith MM, Zhang Y, Carlozzi NE, Paulsen JS, The PREDICT-HD Investigators of the Huntington Study Group (2012) Cognitive domains that predict time to diagnosis in prodromal Huntington disease. J Neurol Neurosurg Psychiatry 83:612–619. doi:10.1136/jnnp-2011-301732
Campodonico JR, Aylward E, Codori A, Yound C, Krafft L, Magdalinski M, Ranen N, Slavney PR, Brandt J (1998) When does Huntington’s disease begin? J Int Neuropsychol Soc 4:467–473
Jurgens CK, van de Wiel L, van Es A, Grimbergen YM, Witjes-Ané MN, van der Grond J, Middelkoop HA, Roos RA (2008) Basal ganglia volume and clinical correlates in ‘preclinical’ Huntington’s disease. J Neurol 255(11):1785–1791. doi:10.1007/s00415-008-0050-4
Snowden JS, Craufurd D, Thompson J, Neary D (2002) Psychomotor, executive, and memory function in preclinical Huntington’s disease. Neuropsychol Dev Cognit Sect A 24(2):133
Stout JC, Jones R, Labuschagne I, O’Regan AM, Say MJ, Dumas EM, Queller S, Justo D, Santos RD, Coleman A, Hart EP, Dürr A, Leavitt BR, Roos RA, Langbehn DR, Tabrizi SJ, Frost C (2012) Evaluation of longitudinal 12 and 24 month cognitive outcomes in premanifest and early Huntington’s disease. J Neurol Neurosurg Psychiatry 83(7):687–694. doi:10.1136/jnnp-2011-301940
Witjes-Ané MN, Mertens B, van Vugt JP, Bachoud-Lévi AC, van Ommen G, Roos RA (2007) Longitudinal evaluation of “presymptomatic” carriers of Huntington’s disease. J Neuropsychiatry Clin Neurosci 19(3):310–317
Acknowledgments
The authors thank all participants for their effort and A.T.M. Willemsen for his help with the FDG–PET data analysis. This work was financed by the Prinses Beatrix Fonds, Project No. 99-0209.
Ethical standards
This study was approved by the local ethics committee and the research was conducted in compliance with institutional guidelines. All subjects gave their written informed consent.
Conflicts of interest
The research was conducted in compliance with institutional guidelines. There are no potential conflicts of interest in this study. This manuscript, or parts of it, has not been previously published elsewhere nor has it been submitted simultaneously for publication elsewhere.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herben-Dekker, M., van Oostrom, J.C.H., Roos, R.A.C. et al. Striatal metabolism and psychomotor speed as predictors of motor onset in Huntington’s disease. J Neurol 261, 1387–1397 (2014). https://doi.org/10.1007/s00415-014-7350-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7350-7