Abstract
Purpose
The aims of this paper were to evaluate the clinical features of patients with primary duodenal adenocarcinoma and to address the prognostic relevance of different surgical and pathological variables after potentially curative pancreaticoduodenectomy.
Methods
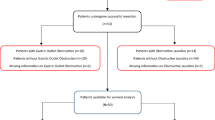
Patients with primary duodenal adenocarcinoma observed from 2000 through 2009 were identified from a single-institution electronic database. Univariate and multivariate analyses were performed to identify factors associated with survival.
Results
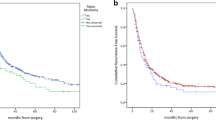
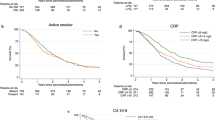
The study population consisted of 37 patients. Of these, 25 underwent pancreaticoduodenectomy, while the remaining 12 were not amenable to resection and underwent bypass operations or were given best supportive care. Overall survival after radical resection (R0) was significantly longer than after palliative surgery (180 versus 35 months, p = 0.013). On multivariate analysis, tumor grade (hazard ratio (HR) = 1.345, 95% CI = 1.28–1.91, p = 0.03) and the occurrence of postoperative or abdominal complications (HR = 1.781, 95% CI = 1.10–2.89, p = 0.037; HR = 1.878, 95% CI = 1.21–3.08, p = 0.029) were found to be significant prognostic factors for survival in patients undergoing potentially curative resection. In particular, median survival was 180 months in patients with an uneventful postoperative course and 52 months in those with abdominal complications. The 5-year overall survival rates were 100 and 60 %, respectively.
Conclusions
According to the present findings, the development of postoperative complications may be an additional prognostic factor after potentially curative pancreaticoduodenectomy for primary duodenal adenocarcinoma. This emphasizes the need for centralization to high-volume centers where an appropriate postoperative care can be delivered.




Similar content being viewed by others
References
Spira IA, Ghazi A, Wolff WI (1977) Primary adenocarcinoma of the duodenum. Cancer 39:1721–1726
Barclay TH, Kent HP (1962) The diagnosis of primary tumors of the duodenum. Gut 3:49–53
van Ooijen B, Kalsbeek HL (1988) Carcinoma of the duodenum. Surg Gynecol Obstet 166:343–347
Joesting DR, Beart RW, van Heerden JA, Weiland LH (1981) Improving survival in adenocarcinoma of the duodenum. Am J Surg 141:228–231
Rose DM, Hochwald SN, Klimstra DS, Brennan MF (1996) Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg 183:89–96
Barnes G Jr, Romero L, Hess KR, Curley SA (1994) Primary adenocarcinoma of the duodenum: management and survival in 67 patients. Ann Surg Oncol 1:73–78
Santoro E, Sacchi M, Scutari F, Carboni F, Graziano F (1997) Primary adenocarcinoma of the duodenum: treatment and survival in 89 patients. Hepatogastroenterology 44:1157–1163
Sohn TA, Lillemoe KD, Cameron JL, Pitt HA, Kaufman HS, Hruban RH, Yeo CJ (1998) Adenocarcinoma of the duodenum: factors influencing long-term survival. J Gastrointest Surg 2:79–87
Bucher P, Gervaz P, Morel P (2005) Long-term results of radical resection for locally advanced duodenal adenocarcinoma. Hepatogastroenterology 52:1727–1729
Cecchini S, Correa-Gallego C, Desphande V, Ligorio M, Dursun A, Wargo J, Fernàndez-Del Castillo C, Warshaw AL, Ferrone CR (2012) Superior prognostic importance of perineural invasion vs. lymph node involvement after curative resection of duodenal adenocarcinoma. J Gastrointest Surg 16:113–120
Zhang S, Cui Y, Zhong B, Xiao W, Gong X, Chao K, Chen M (2011) Clinicopathological characteristics and survival analysis of primary duodenal cancers: a 14-year experience in a tertiary centre in South China. Int J Colorectal Dis 26:219–226
Chung WC, Paik CN, Jung SH, Lee KM, Kim SW, Chang UI, Yang JM (2011) Prognostic factors associated with survival in patients with primary duodenal adenocarcinoma. Korean J Intern Med 26:34–40
Howe JR, Klimstra DS, Moccia RD, Conlon KC, Brennan MF (1998) Factors predictive of survival in ampullary carcinoma. Ann Surg 228:87–94
Conlon KC, Klimstra DS, Brennan MF (1996) Long-term survival after curative resection for pancreatic ductal adenocarcinoma: clinicopathological analysis of 5-year survivors. Ann Surg 223:273–279
Brennan MF (1990) Duodenal cancer. Asian J Surgery 13:204–209
Bakaeen FG, Murr MM, Sarr MG, Thompson GB, Farnell MB, Nagorney DM, Farley DR, van Heerden JA, Wiersema LM, Schleck CD, Donohue JH (2000) What prognostic factors are important in duodenal adenocarcinoma? Arch Surg 135:635–641
Sarela AI, Brennan MF, Karpeh MS, Klimstra D, Conlon KC (2004) Adenocarcinoma of the duodenum: importance of accurate lymph node staging and similarity in outcome to gastric cancer. Ann Surg Oncol 11:380–386
Tocchi A, Mazzoni G, Puma F, Miccini M, Cassini D, Bettelli E, Tagliacozzo S (2003) Adenocarcinoma of the third and fourth portions of the duodenum: results of surgical treatment. Arch Surg 138:80–85
Poultsides GA, Huang LC, Cameron JL, Tuli R, Lan L, Hruban RH, Pawlik TM, Herman JM, Edil BH, Ahuja N, Choti MA, Wolfgang CL, Schulick RD (2012) Duodenal Adenocarcinoma: clinicopathologic analysis and implications for treatment. Ann Surg Oncol 19:1923–1935
Onkendi EO, Boostrom SY, Sarr MG, Farnell MB, Nagorney DM, Donohue JH, Kendrick ML, Reid-Lombardo KM, Harmsen WS, Que FG (2012) 15-year experience with surgical treatment of duodenal carcinoma: a comparison of periampullary and extra-ampullary duodenal carcinomas. J Gastrointest Surg 16:682–691
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2009) AJCC cancer staging manual, 7th edn. Springer, New York
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition (2005) Postoperative pancreatic fistula: an International Study Group (ISGPF) definition. Surgery 138:8–13
Ryder NM, Ko CY, Hines OJ, Gloor B, Reber HA (2000) Primary duodenal adenocarcinoma: a 40-year experience. Arch Surg 135:1070–1074
Han SL, Cheng J, Zhou HZ, Zeng QQ, Lan SH (2010) The surgical treatment and outcome for primary duodenal adenocarcinoma. J Gastrointest Cancer 41:243–247
Stell D, Mayer D, Mirza D, Buckels J (2004) Delayed diagnosis and lower resection rate of adenocarcinoma of the distal duodenum. Dig Surg 21:434–438
Hung FC, Kuo CM, Chuah SK, Kuo CH, Chen YS, Lu SN, Chang Chien CS (2007) Clinical analysis of primary duodenal adenocarcinoma: an 11-year experience. J Gastroenterol Hepatol 22:724–728
Lee HG, You DD, Paik KY, Heo JS, Choi SH, Choi DW (2008) Prognostic factors for primary duodenal adenocarcinoma. World J Surg 32:2246–2252
Yeo CJ, Sohn TA, Cameron JL, Hruban RH, Lillemoe KD, Pitt HA (1998) Periampullary adenocarcinoma: analysis of 5-year survivors. Ann Surg 227:821–831
Hirai T, Yamashita Y, Mukaida H, Kuwahara M, Inoue H, Toge T (1998) Poor prognosis in esophageal cancer patients with postoperative complications. Surg Today 28:576–579
Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, Brennan MF, Rusch VW (2004) The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 198:42–50
McArdle CS, McMillan DC, Hole DJ (2005) Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 92:1150–1154
Law WL, Choi HK, Lee YM, Ho JW (2007) The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol 14:2559–2566
Laurent C, Sa Cunha A, Couderc P, Rullier E, Saric J (2003) Influence of postoperative morbidity on long-term survival following liver resection for colorectal metastases. Br J Surg 90:1131–1136
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Jamieson NB, Glen P, McMillan DC, McKay CJ, Foulis AK, Carter R, Imrie CW (2005) Systemic inflammatory response predicts outcome in patients undergoing resection for ductal adenocarcinoma head of pancreas. Br J Cancer 92:21–23
Sharaiha RZ, Halazun KJ, Mirza F, Port JL, Lee PC, Neugut AI, Altorki NK, Abrams JA (2011) Elevated preoperative neutrophil: lymphocyte ratio as a predictor of postoperative disease recurrence in oesophageal cancer. Ann Surg Oncol 18:3362–3369
Ding PR, An X, Zhang RX, Fang YJ, Li LR, Chen G, Wu XJ, Lu ZH, Lin JZ, Kong LH, Wan DS, Pan ZZ (2010) Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage IIA colon cancer. Int J Colorectal Dis 25:1427–1433
Kneuertz PJ, Patel SH, Chu CK, Maithel SK, Sarmiento JM, Delman KA, Staley CA 3rd, Kooby DA (2011) Effects of perioperative red blood cell transfusion on disease recurrence and survival after pancreaticoduodenectomy for ductal adenocarcinoma. Ann Surg Oncol 18:1327–1334
Swartz MJ, Hughes MA, Frassica DA, Herman J, Yeo CJ, Riall TS, Lillemoe KD, Cameron JL, Donehower RC, Laheru DA, Hruban RH, Abrams RA (2007) Adjuvant concurrent chemoradiation for node-positive adenocarcinoma of the duodenum. Arch Surg 142:285–288
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Giuseppe Malleo and Alfredo Tonsi equally contributed to the present findings and share the first authorship.
Rights and permissions
About this article
Cite this article
Malleo, G., Tonsi, A., Marchegiani, G. et al. Postoperative morbidity is an additional prognostic factor after potentially curative pancreaticoduodenectomy for primary duodenal adenocarcinoma. Langenbecks Arch Surg 398, 287–294 (2013). https://doi.org/10.1007/s00423-012-0978-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-0978-9